Diagnostic Imaging of the Foot and Ankle for Physical Therapists
Original Editor - Mike Kecman as part of the The Jackson Clinics Residency Project
Top Contributors - Evan Thomas, Kris Porter, Michael Kecman, Laura Ritchie, Admin, Melissa Coetsee, Kim Jackson and Wanda van Niekerk
Introduction[edit | edit source]
In addition to a thorough history and clinical exam, imaging may be helpful in diagnosing and creating a plan of care for a patient with a foot or ankle injury. Imaging of the foot and ankle can be beneficial to rule in or rule out pathology after trauma to the foot or ankle, or when an injury is not responding to conservative management.
Types of Imaging[edit | edit source]
The types of imaging most commonly used include radiographs, ultrasound, CT-scans and MRI scans.
For bony pathology, there are 3 standard views for a radiograph (X-ray):
- The AP view is projected through the body of the talus and distal tibia
- The lateral view demonstrates the articulation of the distal tibia and talus, as well as a lateral view of the calcaneus and tarsal bones.
- The mortise view displays the talus and the distal tibia without overlay from the fibula
- If instability is suspected a stress image can be taken to determine ligamentous laxity. Imaging is then performed with the ankle in weight-bearing in order to determine whether seperation occurs at the syndesmosis when loaded
If severe soft tissue damage is suspected, an MRI or diagnostic ultrasound may be indicated.[1]
Common Conditions[edit | edit source]
Hallux Valgus[edit | edit source]
Hallux Valgus is a deformity where the great toe deviates laterally and the 1st metatarsal deviates medially to create a valgus angle at the 1st metatarsal-phalangeal joint (MTP). Because this is a bony deformity a radiograph is the gold standard for diagnosis.[2]
Reading a radiograph for Hallux Valgus:[edit | edit source]
- Preferred radiograph view is a dorsoplantar view in weight bearing
- The valgus angle is measured from the 1st metatarsal to the great toe
- An angle >15 degrees is considered a hallux valgus deformity.[3]
Lateral Ankle Sprain[edit | edit source]
The lateral ankle ligaments are involved in 95% of ankle sprains.[1] In lateral ankle sprains, 66% are isolated tears of the anterior talofibular ligament (ATFL), 20% have associated calcaneofibular ligament (CFL) sprains and the posterior talofibular ligament (PTFL) is rarely involved[3]. Imaging for a lateral ankle sprain may be indicated through mechanism of injury, location of pain and positive special tests (anterior drawer and talar tilt test). A study comparing the diagnostic accuracy of MRI, ultrasound, and stress radiograph to the “gold standard”, arthroscopic surgery, found accuracies of 97%, 91% and 67%, respectively in determining tears of the ATFL. The study also compared the ability to determine location of the tears and found that MRIs could accurately tell the location of the tear in 93% of cases and that ultrasound could tell the location in 63% of the cases. [4]
Reading an MRI for lateral ankle sprains[edit | edit source]
- Typically a T2 weighted image from an axial view is used to detect tears in the ATFL.[4]
- Ligamentous injury is indicated if there is discontinuity, a wavy or curved contour or increased signal intensity within the ligament.[4]
Reading an ultrasound for lateral ankle sprains[edit | edit source]
- Imaging is performed with the ankle in slight plantar flexion and inversion to put a stretch on the ATFL[4]
- Ligamentous injury is indicated if there is discontinuity of the ligament or the ligament is hypoechoic.[4]
Syndesmotic (High) Ankle Sprain[edit | edit source]
A syndesmotic ankle sprain occurs when there is an injury to the anterior inferior and posterior inferior tibiofibular ligament and/or the interosseous ligament. Syndesmotic ankle sprains are more common in contact sports and typically occur with external rotation of the tibia on a dorsiflexed ankle on a planted foot. [3]Clinical indications of a syndesmotic ankle sprain may be the mechanism of injury, pain at the distal tibiofibular joint and positive special tests (dorsiflexion external rotation test, squeeze test and cotton test). If a syndesmotic ankle sprain is suspected the initial imaging choice may be 3 view radiographs taken in single leg standing. Radiographs can be beneficial in determining an osseous avulsion, which is present in 50% of syndesmotic ankle sprains, and to determine syndesmotic widening. AP and mortise view radiographs have been shown to have 100% specificity, but poor sensitivity. If a syndesmotic sprain is not indicated on a radiograph, but there are still questions regarding the diagnosis, an MRI may be indicated.[5]
Reading a radiograph for syndesmotic ankle sprains[edit | edit source]
- 3 views taken in single leg weight bearing.[5]
- Look for osseous avulsions in the anterior or posterior aspects of the tibia
- Look for gapping or “clear space” in the posterior aspect of the syndesmosis.>5 mm measured on an AP or mortise view is considered abnormal.[5]
Reading and MRI for syndesmotic ankle sprains[edit | edit source]
- An axial view of T1 and T2 weighted MRIs can be indicated to determine syndesmotic ankle sprains.
- Positive MRI findings for syndesmotic ankle sprains on a plain T1 or T2 weighted image are abnormal course, irregular contour or increased signal intensity.[5]
- A positive finding on a T1 weighted image with contrast is marked signal intensity.[5]
- Additional positive findings with be discontinuity or not being able to visualize the ligament.
Foot and Ankle Fractures[edit | edit source]
If a foot or ankle fracture is suspected it is recommended to use the Ottawa Ankle Rules to screen whether a radiograph is needed. The Ottawa Ankle Rules indicate that a radiograph is indicated if any of the following are positive:
- Tenderness along the posterior medial or lateral malleoli
- Tenderness on the base of the 5th metatarsal
- Tenderness of the navicular
- If the patient is unable to bear weight for 4 steps following the injury
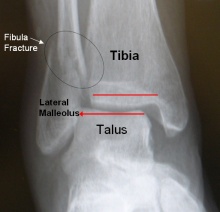
A radiograph with AP, lateral and mortise views are typically sufficient in detecting a foot or ankle fracture. [3]A CT Scan can be used to get a 3 dimensional view in the case of a suspected fracture. A bone scan can be used to detect small fractures or stress fractures within the first 24-48 hours, which may not be picked up by a radiograph or CT scan.[1] Common fracture areas for the foot and ankle are at the malleoli, 5th metatarsal and calcaneus. Malleolar fractures are typically dependent upon the foot position and direction of force. Metatarsal fractures typically occur with trauma, rotational forces or repetitive stress. Fractures of the calcaneus can occur with falls. [3]
Reading a radiograph for ankle/foot fractures[edit | edit source]
- Malleolar fracture: Observe lack of congruency in a bone and/or a low radiodensity black line through the bone.
- 5th Metatarsal fracture: Observe lack of congruency in a bone and/or a low radiodensity black line through the bone.
- Calcaneus fracture: Using a lateral view in non-weight bearing observe lack of congruency in a bone and/or a low radiodensity black line through the bone.
Reading a bone scan for a stress fracture[edit | edit source]
- Observe increased uptake of the radioactive compound at the area of injury.[1]
- In acute injuries the uptake may be more focal, while in chronic injuries the uptake could be throughout the bone
Posterior Tibial Tendinopathy[edit | edit source]
When a clinical exam indicates suspected posterior tibial tendinopathy that may require surgical intervention an MRI is considered the “gold standard” for imaging. MRI imaging for posterior tibial tendinopathy can be taken with T1 and T2 weighted images. Contrast can also be used to enhance the image. The foot is typically held in a neutral position and sagittal and axial images are taken of the tendon. Colour sonography can also been used to detect posterior tibial tendinopathy. Imaging is performed with the patient in prone. The tendon is imaged from posterior to the medial malleolus to the tendon insertion at the navicular. AP and transverse diameters are achieved by modifying the position of the transducer head. While MRI is considered the “gold standard”, one study showed that when comparing ultrasound to MRI, ultrasound had high specificity and sensitivity in diagnosing tendinopathy and peritendinosis.[6]
Reading MRI for Posterior Tibial Tendinopathy [6][edit | edit source]
- Observe an increase in signal intensity on T1 and T2 weighted images in the involved area
- Increased AP diameter of the tendon that creates a rounder tendon
- Increased signal intensity around the peritendinous tissue indicated peritendinosis
Reading ultrasound for posterior tibial tendinopathy [6][edit | edit source]
- Observe mixed echogenic fibers and increased flow in the involved tendon
- Increased AP diameter creating a rounder tendon
- Peritendinosis can be indicated by hyperechoic tissue around the tendon or increased flow in the peritendon
Indications for Imaging[edit | edit source]
It is important to always consider whether imaging will change the patient management plan. If not, it may be sufficient to make a diagnosis based on subjective and objective findings. Imaging may however by indicated in the following scenarios:
- To rule out any fractures in acute injuries, or malignancies in non-acute cases
- To assess stress fractures in patients with persistent foot/ankle pain during loading. Knowledge of common stress fracture sites and mechanisms will help to determine the likelihood
- If a patient fails to recover as expected or does not respond to conservative management
See also: Diagnostic Imaging: Best Practice
Links to Diagnostic Imaging Pages[edit | edit source]
Diagnostic Imaging for the Physical Therapist
Diagnostic Imaging of the Knee
Diagnostic Imaging for the Lumbar spine
References:[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Swain J, Bush K. Diagnostic Imaging for Physical Therapists. St. Louis: Saunders Elsevier; 2009; pg 152, 187
- ↑ Lee KM, Ahn S, Chung CY, Sung KH, Park MS. Reliability and Relationship of Radiographic Measurements in Hallux Valgus. Clinical Orthopedics and Related Research; 2012
- ↑ 3.0 3.1 3.2 3.3 3.4 Houck J, Neville C, Chimenti R. The Foot and Ankle: Physical Therapy Patient Management Utilizing Current Evidence. Current Concepts of Orthopedic Physical Therapy 2012; 3: 30-31
- ↑ 4.0 4.1 4.2 4.3 4.4 Oae K, Takao U Y, Ochi M. Evaluation of Anterior Talofibular Ligament injury with stress radiography, ultrasonography and MR imaging. Skeletal Radiol. Aug 15 2009; 39 (1): 41-47
- ↑ 5.0 5.1 5.2 5.3 5.4 Sheyerer M, Helfet D, Wirth S, Werner C. Diagnostics in suspicion of Ankle Syndesmotic Injury. Am J Orthop. 2011; 40(4): 192-197
- ↑ 6.0 6.1 6.2 Premkumar A, Perry MB, Dwyer AJ, Gerber LH, Johnson D, Venzon D, et al. Sonography and magnetic resonance imaging of posterior tibial tendinopathy. Am J Roentgenol, 2002; 178: 223-32