Liver Disease
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton and Kim Jackson
Introduction[edit | edit source]
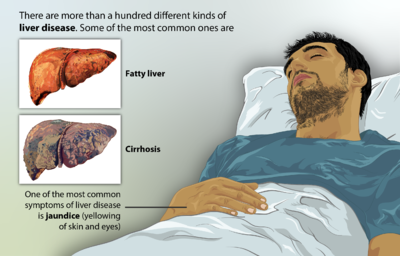
Liver disease is a general term that refers to any condition affecting the liver. These conditions may develop for different reasons, but they can all damage the liver and impact its function.
The spectrum of etiologies is broad for chronic liver disease and include:
- Toxins
- Alcohol abuse for a prolonged time
- Infection
- Autoimmune diseases
- Genetic and metabolic disorders.
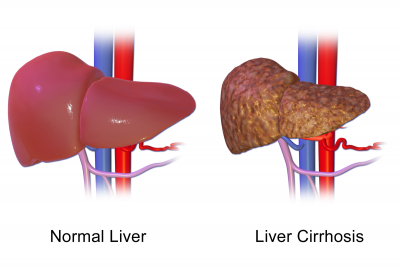
- Cirrhosis (fibrosis) is a final stage of chronic liver disease that results in disruption of liver architecture, the formation of widespread nodules, vascular reorganization, neo-angiogenesis, and deposition of an extracellular matrix.[1]
- Liver disease accounts for approximately 2 million deaths per year worldwide, 1 million due to complications of cirrhosis and 1million due to viral hepatitis and hepatocellular carcinoma. Cirrhosis is currently the 11th most common cause of death globally and liver cancer is the 16th leading cause of death; combined, they account for 3.5% of all deaths worldwide[2].
- The liver is a critical organ in the human body that is responsible for an array of functions that help support metabolism, immunity, digestion, detoxification, vitamin storage among other functions. It comprises around 2% of an adult's body weight. The liver is a unique organ due to its dual blood supply from the portal vein (approximately 75%) and the hepatic artery (approximately 25%).
Function[edit | edit source]
The liver regulates most chemical levels in the blood and produces bile. All the blood leaving the stomach and intestines passes through the liver. The liver processes this blood and breaks down, balances, and creates the nutrients and also metabolizes drugs into forms that are easier to use for the rest of the body or that are nontoxic.
More than 500 vital functions have been identified with the liver. Some of the more well-known functions include the following:[3][4]
- Bile Production - A substance needed to digest and absorb fats. Bile aids in digestion by helping the body absorb fat and certain vitamins, including Vitamins A, D, E and K. In addition, the liver converts the food we eat into nutrients the body can use.
- Fat-Soluble Vitamin Storage and/or Metabolism
- Drug Metabolism - A critical function of the liver is metabolism and/or detoxification of drugs. Other organs, such as the kidney and gut can aid in drug metabolism.
- Manages the synthesis of nearly every plasma protein in the body, some examples include albumin, binding globulins, protein C, protein S, and all the clotting factors of the intrinsic and extrinsic pathways besides factor VIII.
- A key, frontline immune tissue. Ideally positioned to detect pathogens entering the body via the gut, the liver appears designed to detect, capture, and clear bacteria, viruses, and macromolecules. Containing the largest collection of phagocytic cells in the body, this organ is an important barrier between us and the outside world. Importantly, as portal blood also transports a large number of foreign but harmless molecules (e.g., food antigens), the liver's default immune status is anti-inflammatory or immunotolerant (however, under appropriate conditions, the liver is able to mount a rapid and robust immune response)[5].
- Bilirubin Metabolism - Clearance of bilirubin (from red blood cells). If there is an accumulation of bilirubin jaundice results.
- Plays a role in thyroid hormone function as the site of deiodination of T4 to T3.[4]
- Conversion of excess glucose into glycogen for storage (glycogen can later be converted back to glucose for energy) and to balance and make glucose as needed[3]
Etiology[edit | edit source]
The following are the most common etiologies:
- Alcoholic Liver Disease
- Alcoholic liver disease is a spectrum of disease which includes alcoholic fatty liver with or without hepatitis, alcohol hepatitis (reversible because of acute ingestion) to cirrhosis (irreversible). Patients with severe alcohol use disorder mostly develop chronic liver disease; this is the most frequent cause of CLD.
2. Non-alcoholic Fatty Liver Disease (NAFLD/NASH)
- NAFLD has an association with metabolic syndrome (obesity, hyperlipidemia, and diabetes mellitus). Some of these patients develop non-alcoholic steatohepatitis, which leads to fibrosis of the liver. All the risk factors of metabolic syndrome can aggravate the disease process.
3. Chronic Viral Hepatitis
4. Genetic Causes
- Alpha-1 antitrypsin deficiency: This is the most common genetic cause of CLD among children.
- Hereditary hemochromatosis.
- Wilson disease
5. Other Causes of Chronic Liver Disease
- Drugs - amiodarone, isoniazid, methotrexate, phenytoin, nitrofurantoin.
- Idiopathic/cryptogenic, around 15%[1]
Epidemiology[edit | edit source]
Chronic liver disease is one of the frequent causes of death, especially in the developing world (the increasing prevalence of chronic liver disease has been noted in recent times).
The majority of chronic liver diseases in the developed world include alcoholic liver disease, chronic viral hepatitis, including hepatitis B and C, non-alcoholic fatty liver disease (NAFLD), and hemochromatosis[1].
- Liver disease accounts for approximately 2 million deaths per year worldwide, 1 million due to complications of cirrhosis and 1 million due to viral hepatitis and hepatocellular carcinoma.
- Cirrhosis (scarring) is currently the 11th most common cause of death globally and liver cancer is the 16th leading cause of death; combined, they account for 3.5% of all deaths worldwide.
- Cirrhosis is within the top 20 causes of disability-adjusted life years and years of life lost, accounting for 1.6% and 2.1% of the worldwide burden.
- About 2 billion people consume alcohol worldwide and upwards of 75 million are diagnosed with alcohol-use disorders and are at risk of alcohol-associated liver disease.
- Approximately 2 billion adults are obese or overweight and over 400 million have diabetes; both of which are risk factors for non-alcoholic fatty liver disease and hepatocellular carcinoma.
- The global prevalence of viral hepatitis remains high, while drug-induced liver injury continues to increase as a major cause of acute hepatitis.
- Liver transplantation is the second most common solid organ transplantation, yet less than 10% of global transplantation needs are met at current rates[2].
Pathophysiology[edit | edit source]
The chronic liver disease represents a continuous and progressive process of hepatic fibrosis (Cirrhosis), liver tissue architectural distortion, and regeneration nodule formation.
- Fibrosis is usually irreversible, but it can be reversible in the initial stage of development.
- The transition time point of reversible fibrosis to irreversible fibrosis is still not completely understood.
- In chronic liver disease, if not treated, the endpoint is usually irreversible fibrosis, regeneration nodule formation, and development of cirrhosis liver.
- The development rate of fibrosis is dependent on the underlying etiologies, environmental, and host factors[1].
Clinical Signs and Symptoms[edit | edit source]
Chronic liver disease (CLD) is a progressive deterioration of liver functions for more than six months, which includes synthesis of clotting factors, other proteins, detoxification of harmful products of metabolism and excretion of bile[1]. This loss of function leads to the common symptoms.
Liver disease symptoms vary, depending on the underlying cause. General symptoms may include:
- jaundice
- dark urine
- pale, bloody, or black stool
- edema
- nausea
- vomiting
- decreased appetite
- ongoing fatigue
- itchy skin
- easy bruising[6]
Treatment[edit | edit source]
The treatment goal is to stop the progression of the disease and complications and require a multidisciplinary approach. The principle of management is mainly underlying cause correction, Portal hypertension management, and specific treatments for individual disease.[1]
For some people, lifestyle changes are enough to keep symptoms as bay eg:
- limiting alcohol
- maintaining a healthy weight
- drinking more water
- adopting a liver-friendly diet that includes plenty of fiber while reducing fat, sugar, and salt
Depending on the specific liver condition the healthcare provider may recommend other dietary changes. eg. With Wilson’s disease should limit foods containing copper, including shellfish, mushrooms, and nuts.
Depending on the condition affecting the liver, you may also need medical treatment, such as:
- antiviral drugs to treat hepatitis
- steroids to reduce liver inflammation
- blood pressure medication
- antibiotics
- medications to target specific symptoms, such as itchy skin
- vitamins and supplements to boost liver health
In some cases surgery may be used to remove all or part of the liver. Generally, a liver transplant is only done when other options have failed[3].
Physiotherapy[edit | edit source]
More and more health professional are recognizing the value of exercise for liver patients as exercise cause improvements in quality of life and better prognoses.
The following liver benefits have been shown in research to be associated with regular exercise:
- Reduced risk of scarring and cirrhosis in Hepatitis C – Regular exercise reduces the incidence of obesity in HCV patients. Research shows that avoiding obesity helps prevent the resulting conditions – fatty liver, elevated blood glucose, diabetes, and elevated blood insulin – that lead to scarring and cirrhosis.
- Elevated mood – Depression is a common problem amongst people suffering from chronic liver disease.
- Enhanced blood oxygenation – The cardiovascular benefits of regular exercise enhance the oxygen carrying capability of the blood thus more oxygen delivered to the liver, which creates a higher functioning liver.
- Reduced atrophy – Strength-training supports muscle growth and maintenance which can prevent or delay the severe muscle wasting seen in advanced liver disease.
- Improved energy – Over time, regular exercise improves the efficiency of the Cardiovascular System This improves delivery of oxygen and nutrients to all cells, tissues, organs and systems, which leads to a higher energy level[7].
Exercise program - include aerobic/cardiovascular conditioning and strength training to have the greatest effect on liver function.
- Aerobic exercises like walking, bicycling, jogging and swimming will improve your cardiovascular system’s ability to oxygenate your blood and deliver it to the liver and the rest of the body.
- Strength training helps maintain bone mass, increases muscle strength and mass, and helps prevent weight gain through elevation of the metabolism.
- Construct a great home exercise program.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Sharma A, Nagalli S. Chronic Liver Disease. InStatPearls [Internet] 2020 Feb 28. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK554597/ (last accessed 31.10.2020)
- ↑ 2.0 2.1 Asrani SK, Devarbhavi H, Eaton J, Kamath PS. Burden of liver diseases in the world. J Hepatol. 2019 Jan;70(1):151-171. doi: 10.1016/j.jhep.2018.09.014. Epub 2018 Sep 26. PMID: 30266282.Available from:https://pubmed.ncbi.nlm.nih.gov/30266282/ (last accessed 31.10.2020)
- ↑ 3.0 3.1 3.2 John Hopkins Liver Available fromhttps://www.hopkinsmedicine.org/health/conditions-and-diseases/liver-anatomy-and-functions (last accessed 1.11.2020)
- ↑ 4.0 4.1 Kalra A, Tuma F. Physiology, Liver. InStatPearls [Internet] 2018 Dec 18. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK535438/ (last accessed 1.11.2020)
- ↑ Kubes P, Jenne C. Immune responses in the liver. Annual review of immunology. 2018 Apr 26;36:247-77.Available from:https://www.annualreviews.org/doi/abs/10.1146/annurev-immunol-051116-052415 (last accessed 1.11.2020)
- ↑ Healthline Liver disease Available from:https://www.healthline.com/health/liver-diseases#symptoms (last accessed 31.10.2020)
- ↑ Liver Support Exercise for Chronic Liver Disease Available from:https://www.liversupport.com/exercise-for-chronic-liver-disease/ (last accessed 1.11.2020)