Multimorbidity
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton
Introduction[edit | edit source]
Multimorbidity (MM) is commonly understood to be the coexistence of multiple health conditions in an individual (a related term, comorbidity, describes the burden of illness co-existing with a particular disease of interest)[1].
Multimorbidity
- Is a growing global public health challenge as populations age and the prevalence of long-term conditions rises.
- Has emerged as one of the greatest challenges facing health services, both presently and in coming decades.
- The prevalence increases with age, lower SES, and female sex[2].
The leading contributors to the increasing prevalence of multimorbidity are:
- Hypertension (prevalence 18·2%)
- Depression or anxiety (10·3%)
- Chronic pain (10·1%)
This crisis is partly driven by the ageing of the global population
- Prevalence of MM increases substantially with age, present in most people aged 65 years and older.
- Not confined to the older population, with 35% of people aged 55–64 years and 55% of people aged 65–74 years having multimorbidity[3]
- Onset of MM occurred 10–15 years earlier in people living in the most deprived areas compared with the most affluent,[3]
Harrison et al introduced the concept of complex MM (CMM), defined as ‘the co-occurrence of three or more chronic conditions affecting three or more different body systems within one person without an index chronic condition’
- Compared to the basic definition of two or more conditions, the construct of CMM leads to lower prevalence estimates and it has been proposed that it might better identify patients with higher needs[4].
Health Conditions in MM[edit | edit source]
All health conditions can contribute to multimorbidity, including:
- Physical illnesses such as diabetes, heart disease or rheumatoid arthritis.
- Mental health illnesses such as schizophrenia or anxiety.
- Learning disability.
- Hearing loss or poor vision.
- Conditions causing persisting pain.
- Frailty.
- Misuse of alcohol or drugs[5].
Safety Issues[edit | edit source]
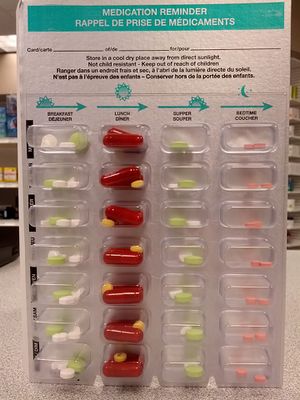
Patients with multimorbidity are at higher risk of safety issues for many reasons, including:
- Polypharmacy, which may lead to poor medication adherence and adverse drug events
- Complex management regimens
- More frequent and complex interactions with health care services leading to greater susceptibility to failures of care delivery and coordination
- Need for clear communication and patient-centred care due to complex patient needs
- Demanding self-management regimens and competing priorities
- Vulnerability to safety issues due to poor health, advanced age, cognitive impairment, limited health literacy and comorbidity of depression or anxiety[6]
Multimorbidity and Physiotherapy[edit | edit source]
Physiotherapists are well equipped to become leaders in managing multimorbidity and the complexities often associated with multimorbidity including: physical and functional decline; increased hospitalisation; reduced participation in daily roles; reduced quality of life; psychological and social impairments; barriers to physical activity.
Management can include
- Minimise disease-specific treatment plans and consider the whole individual, including interactions between conditions (eg, be aware of polypharmacy)
- Engage with clients to negotiate priorities and set meaningful goals eg use of SMART goals ie
- S Specific
- M Measurable
- A Attainable or Assignable
- R Realistic
- T Time-related
- Provide clear communication between healthcare settings to streamline the continuum (eg, write GP letters, give comprehensive handovers).
- Consider motivational and environmental factors contributing to their goal adherence (eg, access to transport, social supports, mental health resources[7])
Rehabilitation Classes
Worldwide healthcare delivery focuses on single diseases. This challenges those caring for patients with chronic disease, as multimorbidity has direct management implications.
- Rehabilitation is integral to chronic disease management but is frequently structured in single-disease disorders eg.cardiac and pulmonary rehabilitation.
- Patients attending the disease-specific rehabilitation programs are increasingly complex with more co-existing health conditions. eg In the UK, 46% of patients in cardiac rehabilitation have comorbidities.
- While patients with multimorbidity are included in cardiac, heart failure (HF), and pulmonary rehabilitation, their clinical outcomes are less optimal compared to people with single diseases.
- It is feasible to conduct multimorbidity rehabilitation programs in people with chronic diseases[8].
Guidelines for Multimorbidity[edit | edit source]
Clinical guidelines review and summarize evidence about the most effective treatments for specific conditions and provide recommendations for their use. However:
- Almost always focused on single conditions. eg guidelines for diabetes, asthma and stroke.
- Rarely take into account multimorbidity.
- Randomized trials (on which guidelines are based) exclude people with multiple conditions from taking part.
- The potential for interactions between medications and between conditions makes the application of single disease-based clinical guidelines potentially hazardous for people with multiple conditions.
- A recent Cochrane review of interventions specifically for people with multimorbidity found only 10 randomized trials published worldwide [6]
Increasing recognition of the problems attached to multimorbidity led the National Institute for Health and Care Excellence (NICE) to release guidance in 2016 for assessment and management of people with multimorbidity. The essential message from this guideline is that care can and must be individualised for each person.[9]
Conclusions[edit | edit source]
- The ageing population, less healthy lifestyles and an increasing incidence of chronic conditions mean that multimorbidity is on the rise.
- This trend is a major health care challenge facing all countries across the world. In order to safely manage people with multiple conditions, primary care teams need to be well trained, resourced and organized.
- Care needs to be proactive and anticipatory, taking a life cycle approach and including preventive care for those at risk of developing multiple conditions[6].
- Encourage prevention; Many long-term conditions which can be avoided by living a healthy lifestyle. In particular eg coronary heart disease and stroke can be avoided by not smoking, taking regular exercise and eating a healthy diet. Many cancers can be avoided by not smoking. Obesity and its many complications can be avoided by eating a healthy diet and taking regular exercise. Type 2 diabetes can often be avoided by eating a healthy diet, taking regular exercise and keeping your weight within a healthy range. Many skin cancers can be avoided by a sensible approach to sun exposure[5]
References[edit | edit source]
- ↑ Johnston MC, Crilly M, Black C, Prescott GJ, Mercer SW. Defining and measuring multimorbidity: a systematic review of systematic reviews. European Journal of Public Health. 2019 Feb 1;29(1):182-9. Available from:https://academic.oup.com/eurpub/article/29/1/182/5033670 Last accessed 28.10.2020.
- ↑ Low LL, Kwan YH, Ko MS, Yeam CT, Lee VS, Tan WB, Thumboo J. Epidemiologic characteristics of multimorbidity and sociodemographic factors associated with multimorbidity in a rapidly aging asian country. JAMA network open. 2019 Nov 1;2(11):e1915245-.Available from:https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2755312 (last accessed 28.10.2020)
- ↑ 3.0 3.1 Pearson-Stuttard J, Ezzati M, Gregg EW. Multimorbidity—a defining challenge for health systems. The Lancet Public Health. 2019 Dec 1;4(12):e599-600..Available from:https://www.thelancet.com/journals/lanpub/article/PIIS2468-2667(19)30222-1/fulltext (last accessed 27.10.2020)
- ↑ Singer L, Green M, Rowe F, Ben-Shlomo Y, Kulu H, Morrissey K. Trends in multimorbidity, complex multimorbidity and multiple functional limitations in the ageing population of England, 2002–2015. Journal of comorbidity. 2019 Aug 30;9:2235042X19872030.Available from;https://journals.sagepub.com/doi/full/10.1177/2235042X19872030 (last accessed 28.10.20200
- ↑ 5.0 5.1 Patient Frailty and Multimorbidity Available from:https://patient.info/senior-health/ageing/frailty-and-multimorbidity# (last acessed 28.10.2020)
- ↑ 6.0 6.1 6.2 Multimorbidity: Technical Series on Safer Primary Care. Geneva: World Health Organization; 2016. Licence: CC BY-NC-SA 3.0 IGO.Available from:https://apps.who.int/iris/bitstream/handle/10665/252275/9789241511650-eng.pdf;sequence=1 (last accessed 27.10.2020)
- ↑ bodyright Four Facts About Gerontological Physiotherapy Available from: https://www.bodyrighthealthcare.com.au/four-facts-about-gerontological-physiotherapy/(last accessed 28.10.2020)
- ↑ Barker K, Holland AE, Lee AL, Haines T, Ritchie K, Boote C, Saliba J, Lowe S, Pazsa F, Thomas L, Turczyniak M. Multimorbidity rehabilitation versus disease-specific rehabilitation in people with chronic diseases: a pilot randomized controlled trial. Pilot and feasibility studies. 2018 Dec 1;4(1):181.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6267787/ (last accessed 28.10.2020)
- ↑ Farmer C, Fenu E, O'Flynn N, et al; Clinical assessment and management of multimorbidity: summary of NICE guidance. BMJ. 2016 Sep 21354:i4843. doi: 10.1136/bmj.i4843.Available from:https://pubmed.ncbi.nlm.nih.gov/27655884/