Reactive Balance: Intervention Strategies
Original Editor - Selena Horner
Top Contributors - Selena Horner, Kim Jackson and Lucinda hampton
Description[edit | edit source]
The biggest goal when working with people who demonstrate gait instability or fear of falling is to help them learn how to control their center of gravity. Traditionally the framework for interventions was viewed as incorporating static or dynamic balance interventions. When determining interventions to improve balance and stability, you can now begin to become more detailed in your thought processes. You can incorporate anticipatory adjustments in your balance intervention strategy. You can include reactive balance intervention strategies. Reactive balance is different than anticipatory adjustments because the patient is not aware and cannot plan for the upcoming situation. The most recent research also highlights that the surface under the patient's feet is what is moving. The patient's body has to immediately take action and react without any planning.[1] The outwardly observed goal is for the patient to defy gravity and not fall.
Indication[edit | edit source]
Most individuals who are at risk of falling are candidates for reactive balance intervention strategies.
There is research supporting that our bodies will respond to reactive balance interventions. Both younger and older adults can respond to this type of intervention. Based on this study the improved response will last at least 24 hours.[2]
At this time, reaction balance intervention strategies may be helpful for more than one specific population or people with specific conditions. This study indicates reaction balance intervention strategies are helpful for people who have Parkinson's. [3]
Clinical Presentation[edit | edit source]
Clinical presentation includes information you receive from the patient. If you consider patient reported outcome measures, then you will appreciate learning the Activities-Specific Balance Confidence Scale.[4] Confidence in balance and fear of falling are predictive of future falls.[5][6] A score < 67% indicates an increased risk of falling.[7]
A patient who needs interventions that include reactive balance will share stories of having difficulty feeling safe walking outdoors. Will report holding onto furniture or walls while walking. Will mention feeling unsteady. Will probably mention slips, trips, near falls or falls.
The Berg Balance Scale is a performance measurement tool that can be used to determine if a patient is at risk of falls. The performance measurement tool you use to determine a patient's risk of falling seems to be dependent upon the patient's current level of function. When choosing a performance measurement tool, ensure the properties of the tool indicate that the tool is appropriate for the patient you are testing. As an example, some performance tools do not actually accurately predict a risk of falling for patients who are independent community dwellers.
As you observe your patient, you may notice that they demonstrate some gait characteristics that could be interpreted as compensating for unsteadiness. Patients will demonstrate a slower gait speed. Patients will decrease their step length. Patients will have an increased step width.[8] You may notice that your patient does not fully pick up their feet as they ambulate.
Resources[edit | edit source]
This is a study that includes a small n value for a randomized controlled trial comparing conventional balance training on a surface that is unstable but is targeted to have postural sway responses mainly involving the ankle joint (ankle strategies) to reactive balance training where the support surface is moved underneath the feet.[9]
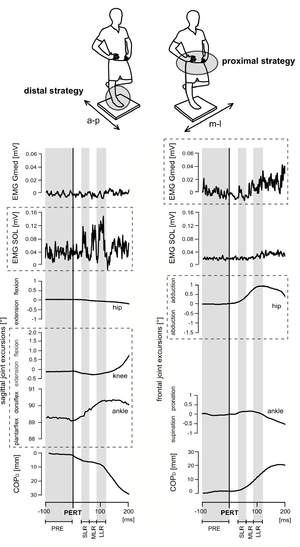
One image in the above study really connected with me to help better understand what is meant by reactive balance training. As you can see, the support surface is moved underneath the person and the person has to respond to that perturbation.
When we begin talking about reactive balance intervention strategies, these types of strategies require some equipment in order to create a situation where the ground is moving under the feet.
This next video should not be considered an endorsement. Creating reactive balance intervention strategies is fairly new in the physiotherapy industry. The best way to get ideas and to understand how to create such an intervention is to look within the market for examples. I consider this next product a reactive balance intervention because the physiotherapist determines the type of perturbation and the speed. As you could see in the above video of myself providing perturbations, I am not able to standardize or necessarily easily adjust the type or amount of perturbation I am able to provide. This particular piece of equipment allows the clinician to adjust the intervention parameters for the patient.
This next set of videos gives you another visual of the ground moving under the feet for a patient response.
| [11] | [12] |
References[edit | edit source]
- ↑ Freyler K, Gollhofer A, Colin R, Brüderlin U, Ritzmann R. Reactive Balance Control in Response to Perturbation in Unilateral Stance: Interaction Effects of Direction, Displacement and Velocity on Compensatory. Neuromuscular and Kinematic Responses. PLoS ONE 2015;12:0144529.
- ↑ Dijkstra BW, Horak FB, Kamsma Y, Peterson DS. Older adults can improve compensatory stepping with repeated postural perturbations. Frontiers in aging neuroscience. 2015 Oct 21;7:201.
- ↑ Mansfield A, Wong JS, Bryce J, Knorr S, Patterson KK. Does perturbation-based balance training prevent falls? Systematic review and meta-analysis of preliminary randomized controlled trials. Physical therapy. 2015 May 1;95(5):700-9.
- ↑ Powell LE, Myers AM. The activities-specific balance confidence (ABC) scale. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 1995;50:M28-34.
- ↑ Merrill R. Landers, Sarrie Oscar, Jessica Sasaoka, Kyle Vaughn; Balance Confidence and Fear of Falling Avoidance Behavior Are Most Predictive of Falling in Older Adults: Prospective Analysis. Physical Therapy 2016;96:433–442.
- ↑ Cleary K, Skornyakov E. Predicting falls in community dwelling older adults using the Activities-specific Balance Confidence Scale. Archives of gerontology and geriatrics 2017;72:142-5.
- ↑ Raad, J, Moore, J, Hamby J, Lainez Rivadelo, R, Straube D. A Brief Review of the Activities-Specific Balance Confidence Scale in Older Adults. Archives of Physical Medicine and Rehabilitation 2013;94:1426-1427.
- ↑ Yiou E, Caderby T, Delafontaine A, Fourcade P, Honeine JL. Balance control during gait initiation: State-of-the-art and research perspectives. World Journal of Orthopedics 2017;11:815.
- ↑ Krause A, Freyler K, Gollhofer A, Stocker T, Bruederlin U, Colin R, Toepfer H, Ritzmann R. Neuromuscular and kinematic adaptation in response to reactive balance training–a randomized controlled study regarding fall prevention. Frontiers in Physiology. 2018;9:1075.
- ↑ Perry Dynamics. Proprio Reactive Balance System Demonstration. Available from: https://www.youtube.com/watch?v=UKGCBf-9LaY
- ↑ Balance Driven. React Board 364 S proprioception and exercise training. Available from: https://www.youtube.com/watch?9=&v=j8iQclyGtIY
- ↑ Balance Driven. Reactive Balance Training on the React Board. Available from: https://www.youtube.com/watch?v=MKF6eqP33zQ