Risk Factors and Injury Mechanisms in Sports Injuries
Original Editor - Wanda van Niekerk based on the course by Ian Gatt
Top Contributors - Wanda van Niekerk, Jess Bell, Kim Jackson and Lucinda hampton
Introduction[edit | edit source]
Musculoskeletal injuries are common in athletes of all levels. The nature of these injuries varies between sports, but the majority of injuries are caused by a combination of factors, and it can be difficult to establish the specific mechanism that leads to injury.[1] Epidemiological studies in sports show that the rate of injury in athletes varies from 10%-65%.[2][3] Because of this, one of the main goals of sports physiotherapists and other professionals in sports is to prevent injury.[4] A key step in evidence-based injury prevention is to identify possible risk factors for injury.[5] Risk factors such as strength, balance, joint mobility and biomechanics are often of interest as these are modifiable, whereas risk factors such as age and previous injury are non-modifiable.[6] Understanding modifiable risk factors is necessary for the design of effective, targeted risk mitigation strategies.[5] This may lead to the development of accurate and reliable tests to investigate risk factors, which are necessary for athlete screening, monitoring over time and to determine the efficacy of injury prevention programmes.[7]
Risk Factors[edit | edit source]
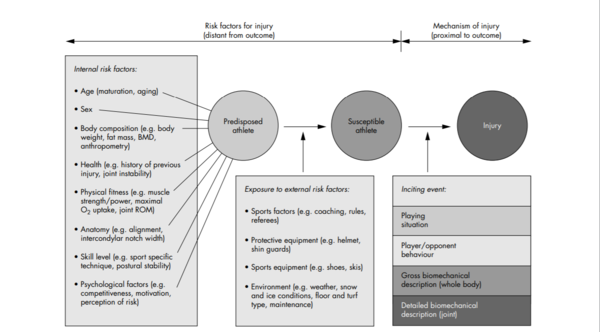
In 2005, Bahr and Krosshaug[8] described risk factors for injury and mechanisms of injury. Internal risk factors that may predispose an athlete can include:
- Age
- Biological sex
- Body composition
- Health
- Physical fitness
- Anatomy
- Skill level
- Psychological factors
When an athlete is exposed to external risk factors, they become susceptible to injury. External risk factors include:
- Sports factors
- Protective equipment
- Environment
When an inciting event (ie injury mechanism) occurs, the athlete is injured. Examples of inciting events are:
- Playing situation
- Player/opponent behaviour
- Gross biomechanical description (whole body)
- Detailed biomechanical description (joint)
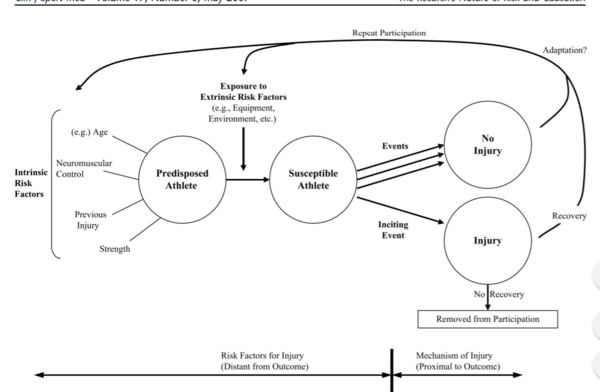
Meeuwisse et al.[1] focused on the intrinsic and extrinsic risk factors for injury and developed a dynamic, recursive model of aetiology in sports injury. This injury prevention model highlights the fact that “adaptations occur within the context of sport (both in the presence and absence of injury) that alter risk and affect aetiology in a dynamic, recursive fashion.”[1] It is suggested that one should look further than the initial risk factors preceding an injury and consider how these risk factors may have changed during various cycles of training or participation.
It is evident that there are multiple factors involved in the risk of injury occurrence and the interaction between these factors may increase the risk. Herrington et al.[9] provides a detailed list of these factors[9]:
- Training-related factors
- Training volume, load, intensity
- Type of training
- Training and competition schedule
- Rest
- Motor control factors
- Posture
- Movement patterns
- Muscle tone
- Technique
- Sport-specific movements
- Psychological factors
- Beliefs
- Fears
- Coping strategies
- Self-efficacy
- Catastrophising
- Emotional status (stress, depression, anxiety)
- Health-related factors
- Diet
- Medication
- General health
- Fatigue
- Sleep patterns
- Non-modifiable factors
- Gender
- Age
- Maturation stage
- Body type
- Genetics
- Previous injuries
- Environmental factors
- Training/competition surface
- Equipment
- Clothing
- Weather
- Coaching
- Conditioning factors
- Strength
- Endurance
- Muscle length
- Joint range of motion
- Chronic capacity
- Additional demands
- Home
- Work
- Family
- Social
- Leadership
- Media
- Sponsors
- Other factors
- Sport-specific skill level
- Ranking and status
- Goals of the athlete
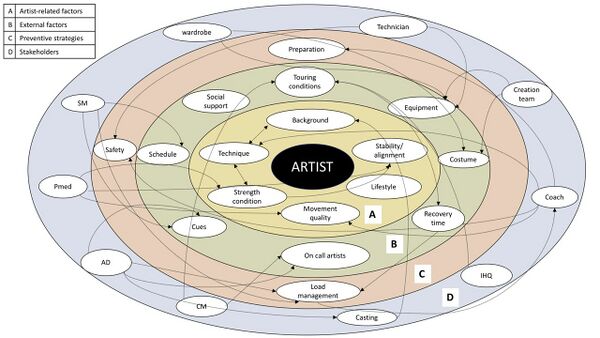
Bolling et al.[10] illustrates the complexity and multiple levels of the factors associated with injury occurrence.
Injury Mechanisms[edit | edit source]
Injury mechanism can also be referred to as the “inciting event.” From a biomechanical perspective, considering tissue properties and load characteristics, an injury occurs when the transfer of energy to the tissue and the mechanical load is in excess of the tissue's load tolerance. The International Olympic Committee Injury and Illness Epidemiology Consensus group[11] define injury as:
“Injury is tissue damage or other derangement of normal physical function due to participation in sports, resulting from rapid or repetitive transfer of kinetic energy.”[11]
This is different for each type of tissue and is dependent on the type of load, the rate of load, the frequency of load and the magnitude of the load. Key points to remember when considering the biomechanical perspective: biomechanics must explain how the injury is caused by mechanical load in excess of the tissue's loadbearing tolerance; or how the mechanical load has reduced the tissue's tolerance level to a point where normal mechanical loads cannot be tolerated.[8]
When considering an epidemiological model, load and load tolerance are influenced by the main elements of the model - the intrinsic risk factors, the extrinsic risk factors and the inciting event.
It is important to have a precise description of the injury mechanism or "inciting event". This information may be used to develop injury prevention measures for specific types of injuries and even for specific sports. According to Bahr and Krosshaug,[8] the description of the injury mechanism should include information on different levels. These levels can be separated into four categories[8]:
- Sports situation
- Team action
- Skills performed before and at point of injury
- Player position
- Court position
- Athlete behaviour
- Player performance
- Opponent interaction
- Whole body biomechanics
- Description of whole-body kinematics and kinetics
- Joint/tissue biomechanics
- Description of joint/tissue kinematics
The following table, adapted from Bahr and Krosshaug,[8] shows how these categories can be implemented:
| Category | Elements | Example of factors describing the injury mechanism:
Knock-out in boxing |
|---|---|---|
| Playing/Sports Situation | Team action | Uppercut, hook |
| Skill performed before and at the point of injury | Counterattack | |
| Court position | Foot work | |
| Player position | Forced into the corner/to the ropes
Ring-side referee decision Inter-boxer distance | |
| Athlete/opponent behaviour | Player performance | Awareness |
| Opponent interaction | Aggressiveness | |
| Player attention | Punching power
Punching speed Balance | |
| Whole-body biomechanics | Coarse description, often static of whole body kinematics and kinetics | Centre of mass velocity
Punching force Punching direction Weight distribution of the legs |
| Joint/tissue biomechanics | Detailed description of joint/tissue kinematics and kinetics | Energy transfer
Head acceleration Pressure distribution and localisation |
There are more examples in Table 1 of this article: Understanding injury mechanisms: a key component of preventing injuries in sport[8]
Sports physiotherapists and sports professionals should know that each injury type has its typical patterns and the same is true of sports. Staying informed by keeping up with evidence-based literature is important for professionals working with athletes in all sports.
Read more on Injury Type and Classification in Sport
Sports Injury Prevention Models[edit | edit source]
Van Mechelen Injury Prevention Model[12]
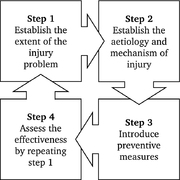
Van Mechelen et al.[12] developed the fundamental, conceptual model for the prevention of sports injuries. This model has since been developed and further adapted for many sports and specific types of injuries. The four steps of action in this model are:
- Identification of the magnitude of the problem (prevalence and incidence of injuries)
- Identification of the cause and mechanism of injury
- Development and implementation of an injury prevention strategy
- Evaluation of the effectiveness of the intervention
Dynamic Model of Aetiology in Sports Injury[1]
Meeuwisse et al.[1] focused on the intrinsic and extrinsic risk factors for injury and developed a dynamic, recursive model of aetiology in sports injury. With this model, the authors suggest it is necessary to look further than just a snapshot of the initial predisposing factors to an injury and consider how these factors change and adapt within the context of the sport.
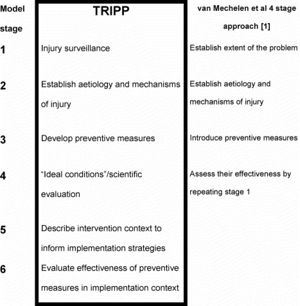
Translating Research Into Injury Prevention Practice (TRIPP) Model[13]
The TRIPP model by Finch[13] considered the context of interventions and the behavioural features of athletes and sports professionals. The TRIPP framework is an extension of the Van Mechelen model and includes two additional steps that are necessary to translate injury prevention strategies into real-life practice. These are: understanding the real world for which the specific intervention is being developed; and the evaluation of this intervention in a real-world setting.[13]
Team-Sport Injury Prevention Cycle
Recently a new model has been proposed for injury prevention in team sports: the Team-sport Injury Prevention (TIP) cycle.[14] The three key phases in this model are[14]:
- (Re)evaluate
- Identify
- Intervene
This model incorporates key aspects of previous models, but also adds insight into implementation aspects. Read more about this here: A new model for injury prevention in team sports: the Team-sport Injury Prevention (TIP) cycle.[14]
See also: Injury Prevention in Sport
Screening and the Element of Causality[edit | edit source]
Musculoskeletal screening is commonly practised in several sports. For many years, the aim of screening was to identify the athletes at risk of injury and to implement injury prevention programmes for these athletes. Screening cannot predict if an athlete will get injured,[15] but screening can help find predisposed athletes. Having a predisposition to a certain injury does not mean that the athlete will get injured. Furthermore, if an athlete does not have a predisposition to an injury, this is not a guarantee that the athlete will not be injured. Athletes become vulnerable to injury when they are exposed to load and inciting events.
Read more about Musculoskeletal Injury Risk Screening
Examples where a specific condition/finding is seen as a causality that then creates an effect:[16]
- Glenohumeral internal rotation deficit (GIRD) in overhead athletes
- Wilk et al.[17] reported that a loss of 20 degrees internal rotation and a loss of 5% of TROM (total range of motion) increases the risk of injury twofold (x2) in professional baseball pitchers
- Shanley et al.[18] showed that a loss of more than 25 degrees into internal rotation is predictive for arm injury in professional baseball players
- More recently, Rose and Noonan suggested that "GIRD in isolation is not a pathologic process, throwers with GIRD often present to the clinic due to the development of shoulder pathology."[19]
So, GIRD in isolation may not be an issue, but just something that is present when an athlete comes for treatment of their injury. What came first? The injury and then the loss of internal rotation or the loss of internal rotation and then the injury?[16]
- Scapular dyskinesis
- Hogan et al.[20] showed that the presence of scapular dyskinesis may increase the risk of shoulder injury, but their findings were not statistically significant. It may very well be that scapular dyskinesis is only a significant risk for shoulder injury when other factors associated with sports injury risk are present (i.e., training load, etc)
Complex System and Risk Identification[edit | edit source]
Sport injuries are multifactorial. Bittencourt et al.[21] proposed the complex systems approach for sports injuries, where the focus is on injury pattern recognition rather than on risk factor identification.[21] The authors argue that a reductionist view is taken in sports injury aetiology investigations where “a phenomenon is simplified into units and analysed as the sum of its basic parts.”[21] With this approach, correlation and regression analyses are undertaken. However, despite the effort, it is still difficult to identify or isolate predictive factors to injury.[21]
Bittencourt et al.,[21] therefore, argue that a complex systems approach should instead be considered. In this approach, athletes are seen as complex (much like the majority of human health conditions) and the injury occurs as a result of complex interactions between a web of determinants (biomechanical, behavioural, physiological, psychological).[21] To prevent sports injuries, risk profiles need to be identified. This requires sports professionals to move away from simply identifying risk factors, and instead adopt a more complex approach of risk pattern recognition. Clinicians should be well informed about the interaction between risk factors, so that they can plan an effective preventative intervention.[21]
Read the full article here: Complex systems approach for sports injuries: moving from risk factor identification to injury pattern recognition—narrative review and new concept[21]
Screening and Preventative Measures[edit | edit source]
There are different views on screening and its use in athletes. Screening cannot predict which athlete will sustain an injury, but there are many benefits of athlete screening.
Read more on:
An editorial by Verhagen et al.[7] summarises how screening can be important for an athlete:
- Positive predictive values
- One of the main injury risk factors is previous injury. Using the example of ACL injuries, the authors used different mathematical approaches to look at risk ratio. When applying the traditional predictive diagnostic test on the data to determine if a previous ACL injury is a predictor of a new ACL injury, a positive predictive value of 29% was reported (i.e., 29% of the participants with a new injury had a previous injury). Using the risk ratio approach, it was reported that the risk of sustaining an ACL injury when having had a previous ACL injury is 3.6 times higher when compared to having had no previous ACL injury.[7]
- Predicting injury versus estimating risk of injury
- In medicine, screening is a strategy to identify an unrecognised disease in individuals with or without symptoms.[7] When applying this to sport, the idea would be to determine if an athlete is injured. However, the aim of injury prevention is to intervene before an injury occurs. This, therefore, changes the context of screening in sports to finding the elements (risk factors) that can lead to injury. In injury risk factor screening, one is looking for an athlete with certain traits that may predispose the athlete to injury. However, there are limitations to paradigms commonly used in screening that professionals involved in sports do not always consider. These are: Complexity and Temporality.[7]
- Complexity
- Injury occurs when different extrinsic and intrinsic risk factors interact with a timely injury mechanism.[21] These occurrences are complex, multifactorial, and unpredictable. When screening athletes, this complex and unpredictable reality needs to be considered - otherwise the screening process may appear meaningless.
- Temporality
- Risk factors do not stand still. Instead, they vary over time. Often screening is performed at a set point in time (i.e., pre-season screening, baseline screening) and injury rates are investigated over the following season or period. However, if the screening tests were performed regularly, the results will change over time as training and match demands will have an effect. Furthermore, risk factors identified in athletes at a pre-season screening will most likely be addressed, thus influencing / reducing injury risk. Therefore, a temporal approach to screening is beneficial (i.e. taking repeated measures rather than just one snapshot in time).[7]
Watch this video where Nicol van Dyk, the second author of this paper discusses their rationale.
Workload: Mediators and Moderators[edit | edit source]
Spikes in training and competition workload are also an injury risk.[24] According to Windt et al.,[24] this workload-injury relationship can be further analysed through mediators and moderators. Mediators can be seen as the steps that explain the association between a variable and an outcome. ("Why changes in workloads might cause injuries?") For example: Rugby league players with spikes in running workload (as determined by the acute:chronic workload ratio) are at an increased risk for a non-contact injury. The mediator in this scenario can be neuromuscular fatigue as increased workloads cause higher levels of fatigue and this may predispose the athlete to an injury.[24]
The moderators are seen to modify the effect of a variable on an outcome. ("What characteristics make certain athletes more robust or susceptible to injury at given workloads?")[24] For example, high aerobic fitness protects against spikes in workload. Thus, aerobic fitness moderates the workload effect by reducing the risk of rapid workload increases.[24]
See Figure 1 in this article: Why do workload spikes cause injuries, and which athletes are at higher risk? Mediators and moderators in workload–injury investigations.
Again, this may seem a simplified approach, but the complexity of injuries needs to be considered as well as the temporality of risk factors.
General Guidelines on Risk Factors and Injury Mechanisms[edit | edit source]
- The effectiveness of screening has been questioned by clinicians and researchers
- Individual risk factors are important; however, it is their summation within a complex individual, over a period of time, which should be considered (complexity and temporality)
- Consider both mediators and moderators
- Understand the sport you are working with and recognise injury risk patterns
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Meeuwisse WH, Tyreman H, Hagel B, Emery C. A dynamic model of etiology in sport injury: the recursive nature of risk and causation. Clin J Sport Med. 2007;17(3):215–219.
- ↑ Alonso JM, Junge A, Renstrom P, Engebretsen L, Mountjoy M, Dvorak J. Sports injuries surveillance during the 2007 IAAF World Athletics Championships. Clin J Sport Med. 2009;19(1):26–32.
- ↑ Junge A, Engebretsen L, Mountjoy ML, Alonso JM, Renstrom PA, Aubry MJ, et al. Sports injuries during the Summer Olympic Games 2008. Am J Sports Med. 2009;37(11):2165–2172.
- ↑ Saragiotto BT, Di Pierro C, Lopes AD. Risk factors and injury prevention in elite athletes: a descriptive study of the opinions of physical therapists, doctors and trainers. Braz J Phys Ther. 2014;18(2):137–143.
- ↑ 5.0 5.1 Collings TJ, Bourne MN, Barrett RS, du Moulin W, Hickey JT, Diamond LE. Risk factors for lower limb injury in female team field and court sports: a systematic review, meta-analysis, and best evidence synthesis. Sports Medicine. 2021 Apr;51(4):759-76.
- ↑ Fulton J, Wright K, Kelly M, Zebrosky B, Zanis M, Drvol C, Butler R. Injury risk is altered by previous injury: a systematic review of the literature and presentation of causative neuromuscular factors. International journal of sports physical therapy. 2014 Oct;9(5):583.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 Verhagen E, van Dyk N, Clark N, Shrier I. Do not throw the baby out with the bathwater; screening can identify meaningful risk factors for sports injuries. British journal of sports medicine. 2018 Oct 1;52(19):1223-4.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 Bahr R, Krosshaug T. Understanding injury mechanisms: a key component of preventing injuries in sport. Br J Sports Med 2005: 39: 324-329.
- ↑ 9.0 9.1 Herrington LC, Munro AG, Jones PA. Assessment of factors associated with injury risk. In: Performance Assessment in Strength and Conditioning 2018 Oct 9 (pp. 53-95). Routledge.
- ↑ 10.0 10.1 Bolling C, Mellette J, Pasman HR, Van Mechelen W, Verhagen E. From the safety net to the injury prevention web: applying systems thinking to unravel injury prevention challenges and opportunities in Cirque du Soleil. BMJ open sport & exercise medicine. 2019 Feb 1;5(1):e000492.
- ↑ 11.0 11.1 International Olympic Committee Injury and Illness Epidemiology Consensus Group, Bahr R, Clarsen B, Derman W, Dvorak J, Emery CA, Finch CF, Hägglund M, Junge A, Kemp S, Khan KM. International Olympic Committee consensus statement: methods for recording and reporting of epidemiological data on injury and illness in sports 2020 (including the STROBE extension for sports injury and illness surveillance (STROBE-SIIS)). Orthopaedic journal of sports medicine. 2020 Feb 14;8(2):2325967120902908
- ↑ 12.0 12.1 Van Mechelen W, Hlobil H, Kemper HC. Incidence, severity, aetiology and prevention of sports injuries. A review of concepts. Sports Med. 1992;14(2):82–99
- ↑ 13.0 13.1 13.2 Finch C. A new framework for research leading to sports injury prevention. J Sci Med Sport. 2006;9(1-2):3–9.
- ↑ 14.0 14.1 14.2 O’Brien J, Finch CF, Pruna R, McCall A. A new model for injury prevention in team sports: the Team-sport Injury Prevention (TIP) cycle. Science and Medicine in Football. 2019 Jan 2;3(1):77-80.
- ↑ Bahr R. Why screening tests to predict injury do not work—and probably never will…: a critical review. British journal of sports medicine. 2016 Jul 1;50(13):776-80.
- ↑ 16.0 16.1 Gatt, Ian. Risk Factors and Injury Mechanisms in Sports. Plus. Course. 2022.
- ↑ Wilk KE, Macrina LC, Fleisig GS, Porterfield R, Simpson CD, Harker P, Paparesta N, Andrews JR. Correlation of glenohumeral internal rotation deficit and total rotational motion to shoulder injuries in professional baseball pitchers. The American journal of sports medicine. 2011 Feb;39(2):329-35.
- ↑ Shanley E, Rauh MJ, Michener LA, Ellenbecker TS, Garrison JC, Thigpen CA. Shoulder range of motion measures as risk factors for shoulder and elbow injuries in high school softball and baseball players. The American journal of sports medicine. 2011 Sep;39(9):1997-2006.
- ↑ Rose MB, Noonan T. Glenohumeral internal rotation deficit in throwing athletes: current perspectives. Open access journal of sports medicine. 2018;9:69.
- ↑ Hogan C, Corbett JA, Ashton S, Perraton L, Frame R, Dakic J. Scapular dyskinesis is not an isolated risk factor for shoulder injury in athletes: A systematic review and meta-analysis. The American Journal of Sports Medicine. 2021 Aug;49(10):2843-53.
- ↑ 21.0 21.1 21.2 21.3 21.4 21.5 21.6 21.7 21.8 Bittencourt NF, Meeuwisse WH, Mendonça LD, Nettel-Aguirre A, Ocarino JM, Fonseca ST. Complex systems approach for sports injuries: moving from risk factor identification to injury pattern recognition—narrative review and new concept. British journal of sports medicine. 2016 Nov 1;50(21):1309-14.
- ↑ Sports Map. Natalia Bittencourt: Complex System and Risk Identification. Available from: https://www.youtube.com/watch?v=IaC0vNeQ1c0[last accessed 06/04/2022]
- ↑ Clinical Athlete. Injury Risk & Screening. Available from: https://www.youtube.com/watch?v=lvP_KtQf3Xc [last accessed 06/04/2022]
- ↑ 24.0 24.1 24.2 24.3 24.4 Windt J, Zumbo BD, Sporer B, MacDonald K, Gabbett TJ. Why do workload spikes cause injuries, and which athletes are at higher risk? Mediators and moderators in workload–injury investigations. British journal of sports medicine. 2017 Jul 1;51(13):993-4.