Ulnar Impaction Syndrome
Original Editor Doctor of Physical Therapy Students at Texas State University - San Marcos Top Contributors - Erin Locati, Heather Hughes, Kristen Tsuei, Melissa Osti, Tori Westcott, Kim Jackson, Admin, Anas Mohamed, 127.0.0.1, Claire Knott, WikiSysop and Uchechukwu Chukwuemeka
Definition/Description[edit | edit source]
Ulnar impaction syndrome, also called ulnocarpal abutment syndrome, is a common cause of ulnar-sided wrist pain.[1][2] It is a degenerative condition in which the ulnar head abuts the triangular fibrocartilage complex (TFCC) and ulnar-sided carpals.[3][4] This abutment results in increased load bearing across the ulnar head, TFCC and ulnar carpals, and subsequent degeneration of the TFCC, chondromalacia of the osseous structures involved (ulna and carpals, especially the lunate), and disruption of the triquetrolunate ligament.[2][5]
Epidemiology/Etiology[edit | edit source]
The most common pre-disposing factor for Ulnar Impaction Syndrome (UIS) is positive ulnar variance - that is, an increased ulnar length relative to the radius. Positive ulnar variance has been found to inversely relate to TFCC thickness; thus, in the positive ulnar variance wrist, the TFCC is stretched and thin, and greater biomechanical forces, particularly rotation forces, impact the joint. This positive variance can result from[2][3][6][7]:
- a congenital positioning of the ulnar articular surface more distally than the radial articular surface
- acquired radial shortening secondary to trauma - for example, a malunion of the radius after a distal radius fracture, an Essex-Lopresti injury, proximal migration of the radius after radial head excision, or premature physeal closure of the radius
- excessive dynamic ulnar variance greater than normal distal movement of the ulna during forearm pronation and gripping
Wrists that do not have a positive ulnar variance, but are considered "ulnar neutral" or "ulnar negative" can also acquire UIS because variance can increase during functional activities, especially those that include forearm pronation and gripping.[6][8][9] When ulnar variance increases in wrists that are ulnar negative or neutral (and thus have a thicker TFCC), ulnocarpoal load also increases.[1] Therefore, although UIS is most common in those with an ulnar positive wrist, it can also occur in wrists with either negative or neutral variance.[9]
Characteristics/Clinical Presentation[edit | edit source]
Ulnar impaction syndrome is insidious and progressive, so patients can have the syndrome without symptoms or can be severely symptomatic when presenting to physical therapy. Common symptoms are: pain, occasional edema, decreased wrist range of motion, decreased forearm rotation, and tenderness to palpation dorsally just distal to the ulnar head and just volar to the ulnar styloid process. The symptoms are commonly aggravated by forceful grip, forearm pronation, and ulnar deviation.[1]
Differential Diagnosis[edit | edit source]
Ulnar wrist pathologies often present very similarly in impairment and pain pattern. Thus, diagnostic imaging is often required to confirm diagnosis in the case of ulnar-sided wrist pain, and should be considered after the history-taking and clinical exam.[1][10][11][12]
Note: TFCC Injury often occurs secondary to or in conjunction with ulnar impaction syndrome.[10]
| DISORDER | SIGNS & SYMPTOMS | TESTS |
|---|---|---|
| TFCC Injury | - Ulnar wrist pain - Snapping or clicking |
- TFCC compression test - Piano key sign - Supination lift test - Palpation |
| Lunotriquetral Interosseous Ligament (LTIL) Injury | - Joint tenderness - Decreased ROM - Decreased grip strength - Painful clunk with radial & ulnar deviation |
- Ballottement test - Shuck test - Shear test - Ulnar snuffbox test |
| Arthritis - DRUJ -Pisotriquetral |
- Pain & crepitus with loading - Decreased ROM - Decreased grip strength - Localized pain |
- Grind tests - Palpation of joint lines - Ballottement tests - ROM |
| DRUJ Instability | - Pain with forearm rotation | - Grind test - Palpation |
| ECU Pathology | - Pain specific to ECU tendon - ECU subluxation |
- Palpation of ECU tendon over ulnar head - Resisted wrist extension & ulnar deviation - Active forearm supination & ulnar deviation |
| Fracture - Ulnar styloid - Triquetrum - Hamate . |
- Tenderness & edema - Decreased ROM - Decreased wrist strength - Pain with motion |
- Palpation of bony landmarks - DRUJ stability (ulnar styloid) - Resisted 5th digit flexion (hamate) |
| Midcarpal Instability | - Midcarpal clunk with ulnar deviation & pronation - Volar sag at ulnar wrist - Often bilateral |
- Midcarpal shift test |
| Kienbock's Disease | - Chronic wrist pain without trauma - Tender dorsal lunate - Decrease ROM - Decreased grip strength - Arthritis (late stage) |
- Palpate lunate |
| Ulnar Nerve Entrapment | - Paresthesia to 4th & 5th digits - Hand intrinsic weakness |
- Tinel's to Guyon's Canal - History/pattern of symptoms |
| Ulnar Artery Thrombosis | - Night pain - Pain with repetitive activity - Cold intolerance - Exquisite tenderness at site of pathology - Dependent rubor or ulceration or 4th or 5th fingertips - Sympathetic fiber excitation of ulnar proper digital nerves |
- Allen test |
| Dorsal Ulnar Cutaneous Nerve Neuritis | - Sensory changes to 4th & 5th digits - Pain or sensory changes at elbow and/or hand weakness, indicative of more proximal ulnar nerve pathology . |
- Sensory exam - Palpation - Wartenburg sign (motor pathology) - Froment sign (motor pathology) |
Outcome Measures[edit | edit source]
Examination[edit | edit source]
To diagnose ulnar impaction syndrome,a comprehensive wrist exam must be completed. Diagnostic imaging should be performed to support the findings from the clinical exam. The physical therapist should pay specific attention to the following:
- Palpation[8][13]
- Tenderness dorsally just distal to ulnar head
- Tenderness just volar to the ulnar styloid process
- Positive ulnar variance, while static or dynamic
- Range of Motion[8][13][14]
- Painful passive ulnar deviation and forceful pronation
- Decreased flexion, extension, radial & ulnar deviation
- Ulnocarpal Stress Test[15]
- Place wrist in maximum ulnar deviation
- Apply axial load to wrist
- Passively rotate forearm through supination and pronation
- + Test = reproduction of patient’s pain NOTE- Test is sensitive for UIS but can get positive with other pathologies, such as LTIL injury, TFCC injury or isolated arthritis.
- Gripping Rotary Impaction Test (GRIT)[6]
- Place arm by side and elbow in 90 degrees of flexion
- Using a grip dynamometer, measure grip in 3 positions: neutral, full supination, full pronation
- GRIT Ratio=(supinated grip strength)/(pronated grip strength)
- GRIT ratio is greater than 1.0 indicates UIS
- GRIT ratio is greater than 1.0 indicates UIS
Examination of TFCC integrity may be necessary, especially in patients with suspected long-term ulnar impaction syndrome due to commonly seen degeneration of this structure.[7]
- Imaging – used to support physical examination findings
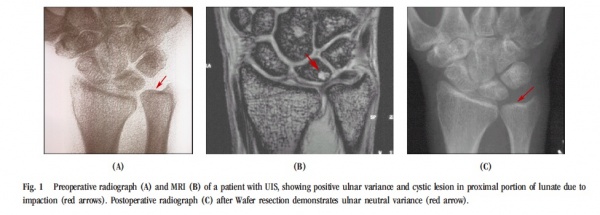
- Radiograph[1][8][14][16]
- Views:
- Neutral rotation P-A radiograph with elbow in 90° flexion
- Pronated grip P-A radiograph
- May have subchondral sclerosis, cystic changes, or osteophyte formation
- Positive ulnar variance is the hallmark of UIS
- Views:
- MRI[8][13][16]
- Detects tears to TFCC and other soft tissue injuries
- May detect decrease in vascular profusion of the lunate and ulnar head or anatomical abnormalities
- Arthrography[8][16][17]
- Currently, considered “gold standard” at detecting damage to TFCC
- Although, recent research is refuting this because of high rates of false-negatives and poor correlation between findings and patient presentation, and stating MRI is more effective
- Computed Tomography[7]
- Used to determine pathology to distal radial-ulnar joint
- Arthroscopy[7]
- Considered “gold standard” for identifying bony lesions
- Fluoroscopy[7]
- Used to assess dye leakage, due to TFCC damage
- Used to assess dye leakage, due to TFCC damage
- Radiograph[1][8][14][16]
Criteria for Ulnocarpal Abutment Syndrome[15][edit | edit source]
- Ulnar wrist pain with tenderness just distal to the ulnar head (dorsal and/or palmar)
- Ulceration or cystic lesion of the lunate ulnar base and/or ulnar head of radiography, OR low signal intensity of the lunate ulnar base on T1-weighted images of MRI, OR degenerative lesions of the TFCC on arthroscopy (Palmer’s class 2 lesion).
Medical Management[edit | edit source]
Surgery Options[edit | edit source]
Ulnar Shortening Osteotomy[3][18] [edit | edit source]
- Ulna is shortened, 2-3mm of shaft removed and fixated with a tubular or standard compression plate
- Indicated: history of ulnar wrist pain that is worse by rotation and ulnar deviation; positive ulnocarpal stress test, and positive ulnar variance with or without cystic changes
- Contraindicated if patient has advanced arthritis of distal radio-ulnar joint
- Baek et al showed significant improvements for idiopathic UIS:
- Pre-Op modified Gartland & Werley scores: 24 wrist rated poor , 7 fair
- Post-Op modified G&W scores: 24 excellent, 5 good, 1 fair, 1 poor
- Reduced subluxation of distal radio-ulnar jt and degenerative cystic changes of ulnar carpal bones resolved
- Reduced average ulnar variance from +4.6 preoperatively to -.07 postoperatively
- Chun et al showed 100% union in 6-8 wks, 72% excellent results on Gartland & Werley
Arthroscopic Wafer Procedure[19][edit | edit source]
- Indicated if no lunotriqutrial instability, minimal ulnar variance, cystic changes of carpus on radiographs and evidence of degeneration of TFCC on MRI
- Contraindicated if ulnar variance is greater than +4mm
- TFCC debridement before 2.3mm resection from distal ulna
- Good to excellent results 85-100%. Near full range of motion, but grip strength did not improve
- Those who have history of distal radius fracture had significantly more pain after surgery
Tomanino et al [9]
- Combined arthroscopic TFCC debridement and wafer resection.
- Complete pn relief in 8 of 12 patients and increase in grip strength by 36%
Feldon et al[20]
- 69% excellent and 31% good results for open wafer procedure
- Longer post-op immobilization and recovery
Bowers Procedure[21][edit | edit source]
- Resection of ulnar articular head, leaving shaft and styloid relationship intact
- Used if TFCC is intact or able to be reconstructed
Darrach Procedure[21][edit | edit source]
- Ulnar head excision if TFCC is not able to be reconstructed
Sauve-Kapandji Procedure[21][edit | edit source]
- Resection of distal ulna and fusion of ulnar head and radius via screw and/or pins
- Indicated for arthritic RU joint to help patients to maintain TFCC integrity and improve forearm rotation
Complications[edit | edit source]
- Scars, infection, dorsal sensory branch of ulnar nerve damage, numbness in fingers up to 10 hours post-op, delayed or non-union, reflex sympathetic dystrophy, tendonitis of ECU sheath [3][19][22]
Pre-op (~3 months)[3][19][edit | edit source]
- Brace/Splint
- NSAIDS
- Occupational/Physical therapy
- Cortisone injections
- Activity modifications
Post-op:[19][22][23][edit | edit source]
- Immobilization 1-2 wks in long arm splint; 10-14 days sutures are removed
- Referred to OT/PT
- Removable long arm splint 4-8 weeks
- Hand elevation to prevent swelling
- X-ray at 6wks to make sure bones are uniting
- 12-16 weeks before returning to heavy activities
- Cigarette smoking adversely influences healing time of osteotomized ulna
Physical Therapy Management[edit | edit source]
Conservative treatment should be attempted before surgery and can include immobilization for 6-12 weeks, NSAIDs, corticosteroid injection and limiting aggravating movements such as pronation, gripping and ulnar deviation. Lack of improvement with conservative management is an indication for surgery.[1][6][7]
UIS can be associated with class 2 TFCC injury and resulting instability of the distal radial-ulnar joint (DRUJ).[7][16][24][25] The therapist should use an impairment based approach to post-surgery treatment and keep in mind that post-surgery patients have had an ulnar resection or removal of a section of the ulnar shaft, deficits resulting from immobilization and may also have TFCC compromise with DRUJ instability.
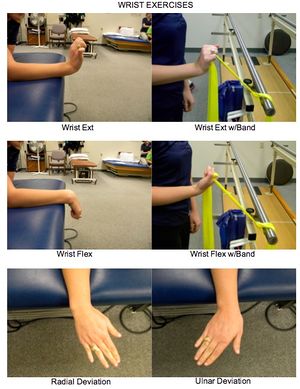
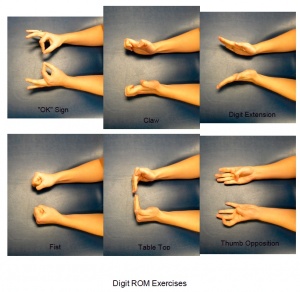
Example Post-Surgery Protocol[1][22][24][26][edit | edit source]
| Timeframe | Goals | Bracing/Splinting | Physical Agents | TherEx | Manual Techniques |
|---|---|---|---|---|---|
| 0 - 2 wks | - Control pain & swelling - Protect surgical site - Maintain ROM in unaffected jts |
- Sugar-tong splint - Long-arm cast |
- Ice - Pain medication |
- NWB - Elevation for edema - Shoulder ROM - Digit ROM |
|
| 2 - 6 wks | - Protect surgical site - Maintain ROM in unaffected jts - Increase elbow & wrist ROM - Scar management |
- Removable elbow-hinged splint or wrist cock-up brace |
- See above - as needed |
- Limited wrist & forearm ROM oustide splint - Stretching of elbow & wrist - Avoid loaded pronation & supination - Continue shoulder & digit ROM |
- Soft tissue massage |
| 6 - 8 wks |
- Increase elbow & wrist ROM |
- Removable splint worn at night |
- See above - as needed |
- Full AROM of elbow & wrist - Stretching of elbow & wrist - Isometric elbow flex/ext & supi/pronation |
- Soft tissue massage |
| 12 - 16 wks | - Address remaining ROM & strength impairments |
- Splint may still be worn at night |
- See above - as needed |
- Full AROM of elbow & wrist - UE strength training |
- Soft tissue massage - Mobilization of elbow forearm & wrist* |
*If joints to be mobilized are considered stable.
ROM exercises should be low-load and high repetition within pain limitations to faciliate cartilage repair.
Full union expected by 3 months post-ulnar shortening osteotomy.[1]
Return to full activity is expected by 6 months post-ulnar shortening osteotomy and 8-12 weeks post-wafer resection.[1]
Example Exercises
Clinical Bottom Line[edit | edit source]
Ulnar impaction syndrome is one of many possible causes of ulnar sided wrist pain, and requires multiple special tests and imaging to confirm diagnosis. If conservative treatment proves ineffective, medical management is indicated and should be followed by physical therapy to address resulting impairments in range of motion, strength, and joint mobility of the upper extremity.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Sammer DM, Rizzo M. Ulnar impaction. Hand Clin. 2010; 26: 549-557.
- ↑ 2.0 2.1 2.2 Katz DI, Seiler JG, Bond TC. The treatment of ulnar impaction syndrome: A systematic review of the literature. J of Surg Orth Adv. 2010; 19(4): 218-222.
- ↑ 3.0 3.1 3.2 3.3 3.4 Baek G, Chung M, Lee Y, Gong H, Lee S, Kim H. Ulnar shortening osteotomy in idiopathic ulnar impaction syndrome. Surgical technique. Journal Of Bone & Joint Surgery, American Volume September 2, 2006;88A:212-220.
- ↑ Harvey WW. Overview of wrist and hand injuries, pathologies, and disorders; part 2. Home Health Care Mgmt & Prac. 2011; 23(2): 146-148
- ↑ Masahiro T, Nakamura R, Horii E, Nakao E, Inagaki H. Ulnocarpal impaction syndrome restricts even midcarpal range of motion. Hand Surg Jul 2005 10(1): 23-27.
- ↑ 6.0 6.1 6.2 6.3 6.4 LaStayo P, Weiss S. The GRIT: A qualitative measure of ulnar impaction syndrome. J Hand Ther. 2001; 14(3): 173-179.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 Sachar K. Ulnar-sided wrist pain: Evaluation and treatment of triangular fibrocartilage complex tears, ulnocarpal impaction syndrome, and lunotriquetral ligament tears. J Hand Surg. 2008; 33A: 1669-1679.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 Webb B, Rettig L. Gymnastic wrist injuries. Current Sports Medicine Reports. September 2008;7(5):289-295.
- ↑ 9.0 9.1 9.2 9.3 Tomaino M, Elfar J. Ulnar impaction syndrome. Hand Clinics [serial online]. November 2005;21(4):567-575.
- ↑ 10.0 10.1 Lichtman D, Joshi A. Ulnar-sided wrist pain. Medscape Reference. Updated July 2009. Available from: http://emedicine.medscape.com/article/1245322-overview#a2. Accessed November 19, 2011.
- ↑ Forman T, Forman S, Rose N. A clinical approach to diagnosing wrist pain. American Family Physician. November 2005;72(9):1753-1758. Available from: American Academy of Family Physicians. Accessed November 20, 2011.
- ↑ Guardia III C, Berman S, Azevedo, C. Ulnar neuropathy clinical presentation. Medscape Reference. Updated May 2011. Available from: http://emedicine/medscape.com/article/1141515-clinical. Accessed November 20, 2011.
- ↑ 13.0 13.1 13.2 13.3 Vezeridis PS, Yoshioka H, Han R, Blazar P. Ulnar-sided wrist pain. Part 1: anatomy and physical examination. Skeletal Radiol. 2010; 39:733-745.
- ↑ 14.0 14.1 Tatebe M, Nakamura R, Horii E, Nakao E, Inagaki H. Ulnocarpal impaction syndrome restricts even midcarpal range of motion. J Hand Surgery. July 2005;10(1):23-27.
- ↑ 15.0 15.1 Nakamura R, Horii E, Imaeda T, Nakao E, Kato H, Watanabe K, The ulnocarpal stress test in the diagnosis of ulnar-sided wrist pain, J Hand Surg. 1997; 22B:719–723.
- ↑ 16.0 16.1 16.2 16.3 Watanabe A, Souza F, Vezeridis PS, Blazar P, Yoshioka H. Ulnar-sided wrist pn II. Clinical imaging and treatment. Skeletal Radiol. 2010; 39: 837-857.
- ↑ Shin AY, Deitch MA, Sachar D, Boyer MI. Ulnar-Sided Wrist Pain: Diagnosis and Treatment. J Bone Joint Surg. July 2004;86A(7):1560-1574.
- ↑ Chun S, Palmer AK. The ulnar impaction syndrome: follow-up of ulnar shortening osteotomy. J Hand Surg. 1993; 24: 316-20.
- ↑ 19.0 19.1 19.2 19.3 Meftah M, Keefer EP, Panagopoulos G, Yang SS. Arthroscopic wafer resection for ulnar impaction syndrome: Prediction of outcomes. J Hand Surg. 2010; 15(2): 89-93.
- ↑ Feldon P, Terrono AL, Belsky MR, The “wafer” procedure, partial distal ulnar resection, Clin Orthop 275: 124-129, 1992.
- ↑ 21.0 21.1 21.2 Duke Orthopaedics: Wheeless’ Textbook of Orthopaedics Website. Avaliable at: http://www.whellessonline.com/ortho/. Accessed November 5, 2011.
- ↑ 22.0 22.1 22.2 Belcher HJ. Ulnar Osteotomy. Available at: http://www.pncl.co.uk/~belcher/information/Ulnar%20osteotomy.pdf. Accessed November 18, 2011.
- ↑ Chen F, Osterman AL, Mahony K. Smoking and bony union after ulna-shortening osteotomy. Am J Orthop. 2001; 30:486-9/
- ↑ 24.0 24.1 Ulnocarpal Impaction Syndrome. Available at: http://eorif.com/WristHand/UlnocarpalImpaction.html. Accessed November 18, 2011.
- ↑ Ozer K, Scheker LR. Distal radioulnar joint and treatment options. Orthopedics. 2006; 29(1): 38-49.
- ↑ Marti RK, van Heerwaarden RJ. Osteotomies for posttraumatic deformities. Thieme; 2008: 221-22.