Dyspareunia: Difference between revisions
Kim Jackson (talk | contribs) m (corrected categories) |
Nicole Hills (talk | contribs) mNo edit summary |
||
| Line 14: | Line 14: | ||
'''Dyspareunia could be a symptom stemming from one or more of the following:''' | '''Dyspareunia could be a symptom stemming from one or more of the following:''' | ||
* skin irritation ( | * skin irritation (i.e. eczema or other skin problems in the genital region)<ref name=":0" /> | ||
* [[endometriosis]]<ref name=":3">The American College of Obstetricians and Gynecologists. When sex is painful. Available from:https://www.acog.org/Patients/FAQs/When-Sex-Is-Painful (accessed 21 Feb 2019).</ref> | * [[endometriosis]]<ref name=":3">The American College of Obstetricians and Gynecologists. When sex is painful. Available from:https://www.acog.org/Patients/FAQs/When-Sex-Is-Painful (accessed 21 Feb 2019).</ref> | ||
* [[Pelvic Floor and Other Pelvic Disorders|vestibulodynia]] | * [[Pelvic Floor and Other Pelvic Disorders|vestibulodynia]] | ||
| Line 31: | Line 31: | ||
'''Objective Assessment''' | '''Objective Assessment''' | ||
The gold standard to assess the pelvic floor muscles is through an internal exam, performed by a trained medical professional with the informed consent of the patient. This exam allows for the assessment of the health of the tissue, the tonicity of the pelvic floor muscles, the ability to contract and relax these muscles | The gold standard to assess the pelvic floor muscles is through an internal exam, performed by a trained medical professional with the informed consent of the patient. This exam allows for the assessment of the health of the tissue, the tonicity of the pelvic floor muscles, the ability to contract and relax these muscles and to assess for vulvodynia and/or vestibulodynia. | ||
'''Outcome Measures''' | '''Outcome Measures''' | ||
| Line 56: | Line 56: | ||
|- | |- | ||
|Pain centralization | |Pain centralization | ||
|If this has been a chronic issue, addressing principles of centralized pain and explaining this to the patient can be helpful and informative. Additionally, pain | |If this has been a chronic issue, addressing principles of centralized pain and explaining this to the patient can be helpful and informative. Additionally, pain at the entrance or through the vaginal canal can elicit a spasm or hypertonic response by the pelvic floor muscles. | ||
|} | |} | ||
'''Additional Considerations''' | '''Additional Considerations''' | ||
* The use of a multidisciplinary approach with the inclusion of a physician and a counselling therapist could be beneficial, depending on the reason for experiencing dyspareunia. | * The use of a multidisciplinary approach with the inclusion of a physician and a counselling therapist could be beneficial, depending on the reason for experiencing dyspareunia. | ||
* Issues such as fatigue, depression/anxiety, stress or history of abuse can contribute to the tension of the pelvic floor muscles and this may be addressed through counselling. | * Issues such as fatigue, depression/anxiety, stress or history of abuse can contribute to the tension of the pelvic floor muscles, and this may be addressed through counselling. | ||
'''Medical management''' | '''Medical management''' | ||
Revision as of 15:49, 7 May 2019
Definition[edit | edit source]
Dyspareunia is defined as persistent genital pain that occurs during sexual intercourse.[1]
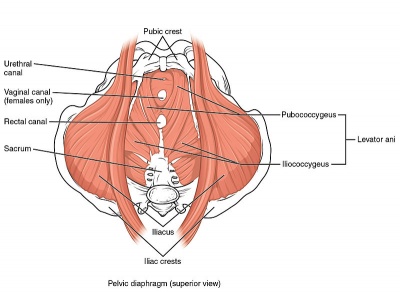
Clinically Relevant Anatomy[edit | edit source]
Please see the page "Pelvic Floor Anatomy," for further details regarding anatomy.
Clinical Exam[edit | edit source]
Subjective History
Individuals may present with pain that occurs at entry during penetration, with deep penetration or pain post-penetration. The patient may also describe pain associated with the insertion of a tampon or during a Pap exam. Words used to describe pain may be (but are not limited to): "throbbing" "burning" or "aching."
Dyspareunia could be a symptom stemming from one or more of the following:
- skin irritation (i.e. eczema or other skin problems in the genital region)[1]
- endometriosis[2]
- vestibulodynia
- vulvodynia[3]
- vaginismus[2]
- interstitial cystitis[3]
- fibromyalgia[3]
- irritable bowel syndrome[3]
- pelvic inflammatory disease[4]
- depression and/or anxiety[4]
- post-menopause[4]
Objective Assessment
The gold standard to assess the pelvic floor muscles is through an internal exam, performed by a trained medical professional with the informed consent of the patient. This exam allows for the assessment of the health of the tissue, the tonicity of the pelvic floor muscles, the ability to contract and relax these muscles and to assess for vulvodynia and/or vestibulodynia.
Outcome Measures
The Female Sexual Destress Scale-Revised (FSDS-R): a single item from this scale may be a useful tool in quickly screening for sexual distress in middle-aged women.[5]
Level of dyspareunia pain (0-10)
Management / Interventions[edit | edit source]
Physiotherapy
Physiotherapists can address factors contributing to dyspareunia with the following tools and techniques.
| Contributing factor | Tool/Technique |
|---|---|
| Lack of awareness of pelvic floor muscles | Assess the patient's ability to connect with their pelvic floor muscles through their ability to correctly contract and relax their pelvic floor muscles. If the patient is unable to correctly recruit these muscles, whether it be due to lack of strength or neuromotor connection, this should be addressed. |
| Hypertonic pelvic floor muscles | Teaching relaxation techniques for the pelvic floor muscles:
The use of inserts can be beneficial along with these techniques. Teach the patient to move the dilator or insert past the entrance of the vaginal canal in conjunction with relaxing the pelvic floor muscles. |
| Pain centralization | If this has been a chronic issue, addressing principles of centralized pain and explaining this to the patient can be helpful and informative. Additionally, pain at the entrance or through the vaginal canal can elicit a spasm or hypertonic response by the pelvic floor muscles. |
Additional Considerations
- The use of a multidisciplinary approach with the inclusion of a physician and a counselling therapist could be beneficial, depending on the reason for experiencing dyspareunia.
- Issues such as fatigue, depression/anxiety, stress or history of abuse can contribute to the tension of the pelvic floor muscles, and this may be addressed through counselling.
Medical management
Ensure that the patient has been screened by a physician to rule out any differential diagnoses or address co-existing diagnoses that are out of the physiotherapy scope of practice.
Resources[edit | edit source]
Webinar: Dyspareunia - The Physiotherapist's Perspective
Pelvic Physiotherapy - to Kegel or Not?
This presentation was created by Carolyn Vandyken, a physiotherapist who specializes in the treatment of male and female pelvic dysfunction. She also provides education and mentorship to physiotherapists who are similarly interested in treating these dysfunctions. In the presentation, Carolyn reviews pelvic anatomy, the history of Kegel exercises and what the evidence tells us about when Kegels are and aren't appropriate for our patients.
References[edit | edit source]
- ↑ 1.0 1.1 Mayo Clinic. Painful intercourse. Available from:https://www.mayoclinic.org/diseases-conditions/painful-intercourse/symptoms-causes/syc-20375967 (accessed 13 Feb 2019).
- ↑ 2.0 2.1 The American College of Obstetricians and Gynecologists. When sex is painful. Available from:https://www.acog.org/Patients/FAQs/When-Sex-Is-Painful (accessed 21 Feb 2019).
- ↑ 3.0 3.1 3.2 3.3 Reed BD, Harlow SD, Sen A, Edwards RM, Chen D, Haefner HK. Relationship between vulvodynia and chronic comorbid pain conditions. Obstetrics and gynecology. 2012;120(1):145.
- ↑ 4.0 4.1 4.2 Latthe P, Mignini L, Gray R, et al. Factors predisposing women to chronic pelvic pain: systematic review. BMJ. 2006;332:749. Latthe P, Mignini L, Gray R, Hills R, Khan K. Factors predisposing women to chronic pelvic pain: systematic review. BMJ. 2006;332(7544):749-55.
- ↑ Carpenter JS, Reed SD, Guthrie KA, Larson JC, Newton KM, Lau RJ, Learman LA, Shifren JL. Using an FSDS‐R Item to Screen for Sexually Related Distress: A MsFLASH Analysis. Sexual medicine. 2015 Mar;3(1):7-13.