Goniometry
Original Editor - The Open Physio project.
Top Contributors - Rachael Lowe, Innocent Abugu, Admin, Naomi O'Reilly, Uchechukwu Chukwuemeka, Chrysolite Jyothi Kommu, Lucinda hampton, Sonal Joshi, WikiSysop, Claire Knott and Redisha Jakibanjar
Introduction[edit | edit source]
Goniometry is the art and science of measuring the joint ranges in each plane of the joint.[1] The term 'goniometry' is derived from the greek words 'gonia' meaning angle and 'metron' meaning measure, therefore goniometry refers to the measurement of angles, which in rehabilitation settings refers to the measurement of angles in each plane at the joints of the body.
A goniometer is the most common instrument used to measure range of motion.[1] If a patient has altered range of motion in a particular joint, the therapist can use a goniometer to assess what the range of motion is at the initial assessment, and then make sure the intervention is working by using the goniometer in subsequent sessions to assess the effectiveness of the intervention.
Types of Goniometers[edit | edit source]
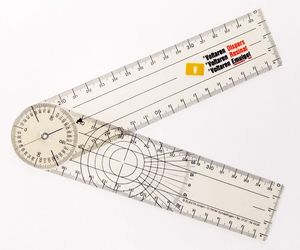
Of all the types, a universal goniometer is most widely used.
- Universal Goniometer (Figure.1)
- Comes in two forms: short arm and long arm.
- The short arm goniometer is used for smaller joints like the wrist, elbow, or ankle,
- The long arm goniometers are more accurate for joints with long levers like the knee and hip joints.
- Gravity Goniometer/Inclinometer (Figure.2)
- One arm has a weighted pointer that remains vertical under the influence of gravity. (Figure.2)
- Software/Smartphone-based Goniometer:
- A smartphone as a digital goniometer has several benefits like availability, ease of measurement, application-based tracking of measurements, and one-hand use. These applications use the accelerometers in phones to calculate the joint angles.
- Arthrodial Goniometer:
- Ideal for measuring cervical rotation, anteroposterior flexion, and lateral flexion of the cervical spine.
- Twin Axis Electrogoniometer:
- The inter-rater and intra-rater reliability of the electrogoniometer is higher than the universal goniometer but challenging to apply in patients' clinical evaluation, hence used more often for research purposes[1]
Validity and Reliability[edit | edit source]
There is some question as to whether or not a goniometer is a sufficiently valid and reliable instrument to determine whether an intervention has been effective.[2]
There are limited validity studies on goniometry, but they have found high criterion validity in measurements of knee joint angles when compared to x-ray joint angles.[3] [4] Reliability depends on the joint and motion being assessed but generally the universal goniometer has been shown to have good to excellent reliability, and is more reliable than visual estimation especially with inexperienced examiners. Some research argues that the reliability of the measurement from a goniometer depends on the type used[5][6] while some did not see any significant difference between some instruments.[7][8] Overall, research shows high intra- and inter-rater reliability of the universal goniometer, with reliability in non-expert examiners improved with clear instructions on goniometric alignment, therefore where possible he same therapist should perform all measures to improve accuracy. Evidence is mixed on on the number of measures to take, or whether taking an average of repeated measures improves assessment. Sources of error when using goniometry can come from our expectations of what the ROM is, reading the wrong side of the scale on the goniometer, a change in the patient’s motivation to perform, or taking successive measurements at different times of the day.[9]
So overall greater reliability is obtained when measures are taken by the same therapist, using a standardised method with the same measurement tool assessed at the same time of day.[1][9][10][11][12] [13][14]
Goniometry Technique[edit | edit source]
It is necessary that a single notation system is used in goniometry. The neutral zero method (0 to 180- degree system) is the most widely used method. The same goniometer should always be used to reduce the chances of instrumental error.
- Position and stabilise the joint correctly.
- Move a body part through its appropriate range of motion (ROM).
- Determine the joint's end of the range of motion and end-feel.
- Palpate the appropriate bony landmarks.
- Align the goniometer with the landmarks.
- Read the measuring instrument properly
- Record measurements correctly (both active and passive range of motion should be measured and recorded respectively).[1]
- The range of motion of each joint should be measured in isolation, to avoid trick movement (simultaneous movement of another joint) and muscle insufficiency which may alter the reading.
Procedures[edit | edit source]
- Ankle (Subtalar) Eversion
- Ankle (Subtalar) Inversion
- Ankle (Talocrural) Dorsiflexion
- Ankle (Talocrural) Plantarflexion
- Elbow Extension
- Elbow Flexion
- Forearm Pronation
- Forearm Supination
- Hip Abduction
- Hip Adduction
- Hip Extension
- Hip Flexion
- Hip External Rotation
- Hip Internal Rotation
- Knee Extension
- Knee Flexion
- Shoulder Abduction
- Shoulder Flexion
- Shoulder Horizontal Abduction
- Shoulder Internal and External Rotation
- Wrist Extension
- Wrist Flexion
- Wrist Radial Deviation
- Wrist Ulnar Deviation
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Goniometer.Viraj N. Gandbhir, Bruno Cunha,In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2020 Jan.2020 Jun 12.Pubmed.gov. National Library of Medicine.National Centre for Biotechnology Information.
- ↑ Goniometer. (2008, August 30). In Wikipedia, The Free Encyclopedia. Retrieved 11:12, September 14, 2008, from http://en.wikipedia.org/wiki/Goniometer.
- ↑ Jordan K. Assessment of published reliability studies for cer- vical range-of-motion measurement tools. J Manip Physiol Ther. 2000;23:180–195.
- ↑ de Koning CHP, van den Heuvel SP, Staal JB, Smits-Engelsman BCM, Hendriks EJM. Clinimetric evaluation of active range of motion measures in patients with non-specific neck pain: a systematic review. Eur Spine J. 2008;17:905-921.
- ↑ Milanese S et al. Reliability and concurrent validity of knee angle measurement: Smart phone app versus universal goniometer used by experienced and novice clinicians. Manual Therapy, 2014; 5: 1–6.
- ↑ Jones A, Sealey R, Crowe M, Gordon S. Concurrent validity and reliability of the simple goniometer iPhone app compared with the universal goniometer. Physiotherapy Theory and Practice. 2014;30 (7): 512–516.
- ↑ Mourcou Q, Fleury A, Diot B, Franco C, Vuillerme N. Mobile Phone-Based Joint Angle Measurement for Functional Assessment and Rehabilitation of Proprioception.Biomed Res Int. 2015; doi: 10.1155/2015/328142
- ↑ Ockendon M, Gilbert RE. Validation of a Novel Smartphone Accelerometer-Based Knee Goniometer. Journal of Knee Surg. 2012;25:341–346.
- ↑ 9.0 9.1 Magee D. Orthopaedic Physical Assessment WB Saunders. pg. 2002;478:483-631.
- ↑ Gajdosik RL, Bohannon RW. Clinical measurement of range of motion: review of goniometry emphasizing reliability and validity. Physical therapy. 1987 Dec 1;67(12):1867-72.
- ↑ Norkin CC, White DJ. Measurement of joint motion: a guide to goniometry. FA Davis; 2016 Nov 18.
- ↑ Blonna, D., Zarkadas, P. C., Fitzsimmons, J. S., & O'Driscoll, S.W. (2012). Accuracy and inter-observer reliability of visual estimation compared to clinical goniometry of the elbow. Knee Surgery, Sports Traumatology, Arthroscopy, 20(7), 1378-85.
- ↑ Boone, D. C., Azen, S. P., Lin, C., Spence, C., Baron, C., & Lee, L. (1978). Reliability of goniometric measurements. Physical Therapy, 58(11), 1355-1360.
- ↑ Blonna, D., Zarkadas, P. C., Fitzsimmons, J. S., & O'Driscoll, S.W. (2012). Accuracy and inter-observer reliability of visual estimation compared to clinical goniometry of the elbow. Knee Surgery, Sports Traumatology, Arthroscopy, 20(7), 1378-85.