ICF in Relation to Wheelchair Users
Original Editor - Laura Ritchie
Top Contributors - Naomi O'Reilly, Laura Ritchie, Kim Jackson, Rucha Gadgil and Jess Bell
Introduction[edit | edit source]
The International Classification of Functioning, Disability and Health (ICF) is a framework for describing functioning and disability in relation to a health condition. It provides a common language and framework for describing the level of function of a person within their unique environment.[1][2] More information on the ICF can be found at International Classification of Functioning, Disability and Health (ICF).
Currently individuals who use a wheelchair encounter many barriers to participation including accessibility problems, low rates of employment, social isolation and stigma. Given these issues it is critical to develop better ways to measure and to understand barriers and facilitators to participation in this population. Using the ICF provides a scientific basis for understanding health and health-related states. It supports looking at and analyzing factors that influence how wheelchair users function and participate in their society/community and enables people to look beyond impairments and activity limitations such as; social, environmental, personal and cultural issues. [3]
ICF in Relation to Wheelchair Users[edit | edit source]
The following table suggests some factors that should be considered when evaluating a patient and their wheelchair using the ICF. [4][5]
| Body Structures and Functions | Activities | Participation | Environmental Factors | Personal Factors |
|---|---|---|---|---|
| Global & mental function | Mobility in the home | Quality of Life | Assistive equipment | Age |
| Sensory function & pain | Mobility in the community | Community participation | Seating system | Understanding & performance of WC skills |
| Voice & speech function | ADLs | Social engagement | Environmental control | BMI |
| Seating position | Physical activity & exercise | Self-care | Wheelchair design & seating configuration | Duration of impairment |
| Wheelchair & seating assessment | Self-esteem | Home, community & work barriers | Marital & socio-economic status | |
| Neuromusculoskeletal and movement-related functions | Work / employment | Transportation | Gender | |
| Severity of condition | Ethnicity | |||
| Cognition | ||||
| Fitness level | ||||
| Upper extremities & trunk |
Uses of the ICF in Research and Clinical Practice with Users of Wheelchairs[edit | edit source]
The ICF has been used in various ways in relation to research and clinical practice involving users of wheelchairs.
For example, Morgan et al (2017) recommended the ICF as a useful tool for identifying key wheelchair skills that needed to be taught during initial rehabilitation versus those that can be addressed once a patient has returned to community life.[6] Using the ICF, the authors identified three areas in which there was a disconnect between what was actually being taught during initial wheelchair rehabilitation and what should ideally be taught;[6]
- Use of the environment for training
- Addressing and accommodating for a psychological adjustment period
- Teaching how to care for and maintain the wheelchair
Similarly, Requejo et al (2015) noted that limitations and restrictions imposed by possible pain and dysfunction in wheelchair users can be defined using the ICF. The authors stated that the ICF can be used both to identify key elements that must be addressed during rehabilitation and also for guiding the provision and classification of assistive technology.[4] Thus, using the ICF can reduce the risk of a mismatch between the needs and capacities of the patient versus the type of wheelchair he is provided, which can in turn decrease the risk of pain, fatigue, pressure ulcers and increase quality of life, confidence and community participation.[4]
Mortenson et al (2008) used the ICF to evaluate wheelchair-specific outcome measures in relation to wheelchair activity and participation. They found two issues when using the ICF for this purpose. First, the majority of items in the outcome measures were coded as d465 (Moving around with equipment) on the ICF, thus the authors suggested that without a subsequent level to break this category down further, this code provides insufficient detail.[7] For example, there is no way to specify the type of equipment being used, the surface in question or whether the patient has to negotiate kerbs, inclines or thresholds. Second, the ICF does not include any subjective elements related to activity and participation.[7]
McDonald et al (2016) suggested that the ICF in itself would be a useful outcome measure in relation to wheelchair seating, positioning and mobility. [8] The authors note that wheelchairs have two main purposes; 1) compensating for or improving body functions and structure and 2) enhancing performance in seating, function and wheeled mobility. Thus, determining the overall success of wheelchair prescription can be a complicated task when reconciling these two purposes. In addition, these two purposes do not include social or environmental factors.[8] By using the ICF as an outcome measure for wheelchair prescription, all contextual factors would be considered and, importantly, given equal weight when determining the suitability of a given wheelchair for a given patient.[8]
Case Example of the ICF in Use[edit | edit source]
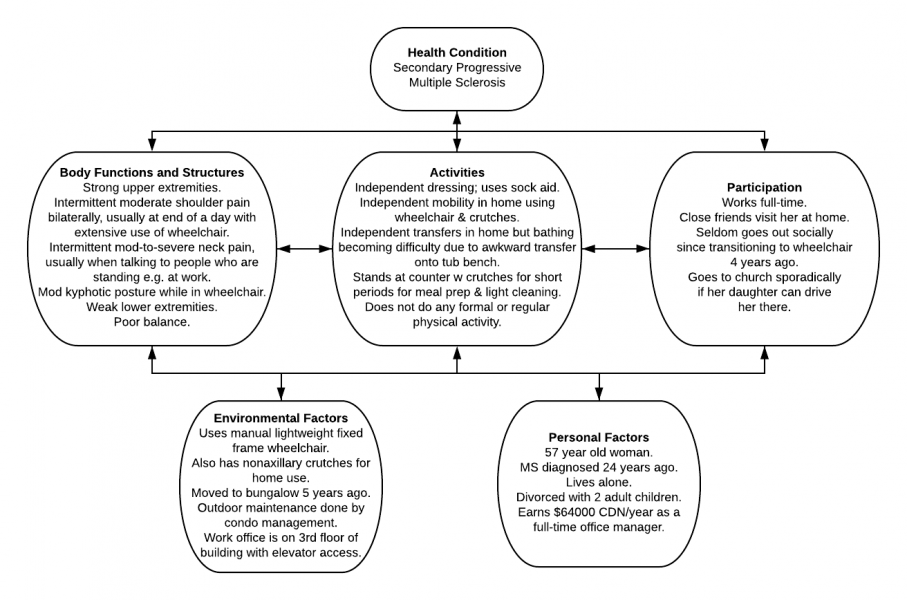
Mrs T is a 57 year old woman who was diagnosed with relapsing remitting multiple sclerosis 24 years ago. Seven years ago, her diagnosis was adjusted to Secondary Progressive MS as the condition progressed according to its natural history. In response to progressive lower extremity weakness and disequilibrium, she was provided with a manual fixed frame wheelchair four years ago. Using the ICF, Mrs T’s situation could be summarized by the following schematic.
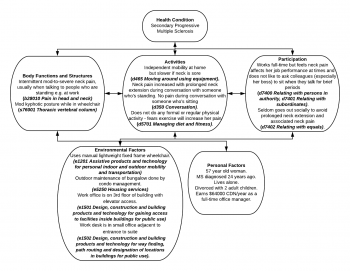
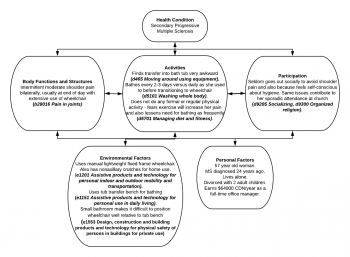
Alternatively, a health care professional could use the ICF to focus on certain related aspects of Mrs T’s situation in order to plan an intervention. For example;
Resources[edit | edit source]
- An introduction to the International Classification of Functioning, Disability and Health (ICF) from the WCPT
- Using the ICF in Clinical Practice from the WCPT
- World Health Organization ICF Resources, a summary from the WCPT
- ICF Core Sets
- ICF Checklist Version 2.1a Clinician Form
References[edit | edit source]
- ↑ Sykes C. Health classifications 1 - An introduction to the ICF. WCPT Keynotes. World Confederation for Physical Therapy. 2006.
- ↑ https://www.wcpt.org/sites/wcpt.org/files/files/GH-ICF_overview_FINAL_for_WHO.pdf The ICF: An Overview. Available at: https://www.wcpt.org/sites/wcpt.org/files/files/GH-ICF_overview_FINAL_for_WHO.pdf
- ↑ Mortenson WB, Miller WC, Auger C. Issues for the selection of wheelchair-specific activity and participation outcome measures: a review. Archives of Physical Medicine and Rehabilitation. 2008 Jun 1;89(6):1177-86.
- ↑ 4.0 4.1 4.2 Requejo PS, Furumasu J, Mulroy SJ. Evidence-Based Strategies for Preserving Mobility for Elderly and Aging Manual Wheelchair Users. Top Geriatr Rehabil. 2015 Jan-Mar;31(1):26-41.
- ↑ Mausen S. Why wheelchair and seating assessment by ICF? Is it necessary or a waste of time? Lecture presented at 2015 International Seating Symposium; University of Pittsburgh.
- ↑ 6.0 6.1 Morgan KA, Engsberg JR, Gray DB. Important wheelchair skills for new manual wheelchair users: health care professional and wheelchair user perspectives. Disabil Rehabil Assist Technol. 2017 Jan;12(1):28-38.
- ↑ 7.0 7.1 Mortenson WB, Miller WC, Auger C. Issues for the selection of wheelchair-specific activity and participation outcome measures: a review. Arch Phys Med Rehabil. 2008 Jun;89(6):1177-86.
- ↑ 8.0 8.1 8.2 McDonald R, Rushton P, Giesbrecht E, Kirby RL, Viswanathan P, Casey J.Outcome measurement in wheelchair seating, positioning and mobility. European Seating Symposium, Dublin, Ireland. European Seating Symposium. 2016. 4 pp. [Conference contribution]