Proprioceptive Neuromuscular Facilitation
Introduction[edit | edit source]
Proprioceptive Neuromuscular Facilitation (PNF) is a therapeutic approach defined as promoting the response of the nerve impulses to recruit muscles through stimulation of the proprioceptors (e.g. Muscle spindle and Golgi Tendon Organs) in addition to other sensory stimuli (tactile, visual or verbal) in the beginning (i.e. at cognitive phase of motor learning) that decrease overtime as learning progresses.[1]
The approach aims to reach the highest level of function and follows the ICF model where it begins with the findings of clinical assessment to stand on the major impairment of body structure or function (e.g. weakness) that may limit an activity (e.g. sit to stand or walking) and restrict life participation (e.g. using transportation or employment) considering the account of environmental barriers (e.g. high floor residence without lifts or narrow spaces, stressful conditions, etc.) and personal factors (e.g. age, fitness level, etc.). Then, the therapist sets treatment goals to treat certain impairment and improve activity or participation.[2].
PNF uses nerve impulses that can excite ,inhibit, relax or strengthen muscles on neurophysiological basis such as spatial summation, temporal summation[3] and reciprocal inhibition[4]. In order to recruit these basis PNF consists of certain principles, procedures and techniques will be illustrated in this page.
Practice[edit | edit source]
First: PNF basic principles[edit | edit source]
Principles [2] are stimuli used in practice that can be exteroceptive (e.g. tactile, verbal/auditory or visual) or proprioceptive stimuli (e.g. resistance, traction, approximation and stretching), all of which are incorporated in all PNF practice with small variations according to patients' condition and treatment goals.
- Tactile stimulus: represented by the correct manual contact and grip for both therapist's hands on the target body part.
- Verbal or auditory stimulus: this is represented by a therapist's command or order to guide the patient for movement and its timing. it can be preparatory or action or feedback.
- Visual stimulus: which is persons can see and follow the movement with their eyes as much as they can. This promotes feedback, influence body and head motions and gives reflexive reinforcement or facilitation to certain muscles.
- Resistance: optimal resistance is performed by the therapist to suit the treatment goal and the patient's ability. Different degrees or intensities of resistance results in different types of muscle contractions.
- Isometric contractions occur when therapist's resistance equals the patient's ability to overcome or the patient stabilizes the position of the extremity with no resistance from the therapist.
- Concentric and eccentric (Isotonic) contractions occur when therapist's resistance is less or higher than patient's ability respectively
- Traction: is the elongation of the extremity or the trunk by the therapist, it is performed all of the movement except on reaching the possible end of pattern.
- Approximation: is the compression of the extremity or trunk and it is mostly done near or by the end of pattern.
- Stretching: stretch stimulus is putting the target muscle in the optimal lengthening position for facilitating muscle contractions, this explains the reason for starting with the pattern that opposes the target pattern and move towards the target pattern.
Second: PNF procedures[edit | edit source]
- irradiation: spreading of response of nerve impulses of stimulus.
- reinforcement: increased stimuli intensity and types will increase the amount of muscle response, making it stronger.
- Body positions and mechanics for both the therapist and the patient, therapist’s shoulders and pelvis face the direction of the motion, position of the patient according to patient's abilities and treatment goals.
- timing: every pattern has fixed sequence of motion (timing) that can be changed to enhance particular muscle response (Timing for emphasis).
- patterns: 3D multiple joint movements result from muscle synergies contractions and assemble normal functional movements. Every pattern has an opposite pattern in each individual joint movement, the two together constitutes a diagonal.
Patterns are named according to the proximal joint movement while the pattern movement starts with the most distal joints. This sequence occurs in every patterns and represents normal timing any change in this sequence is performed as timing for emphasis.
Patterns of extremities[edit | edit source]
First: Unilateral patterns[2]
Patterns are named according to the proximal joint movement while the pattern movement starts with the most distal joints. This sequence occurs in every patterns and represents normal timing any change in this sequence is performed as timing for emphasis.
For upper extremities:
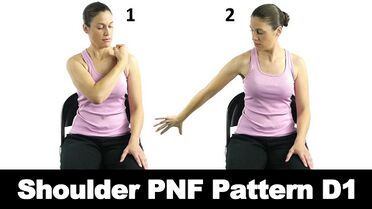
- The first diagonal (D1): Flexion-adduction-external rotation pattern of the gleno-humeral joint and Extension-abduction-internal rotation pattern of the gleno-humeral joint.
- The second diagonal (D2): Flexion-abduction- external rotation pattern of the gleno-humeral joint and Extension-adduction- internal rotation pattern of the gleno-humeral joint.

For lower extremities:
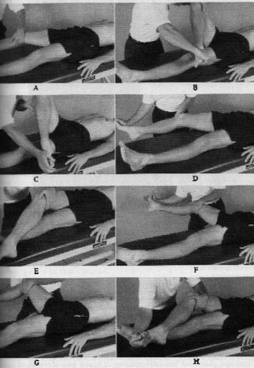
- The first diagonal (D1): Flexion-adduction-external rotation pattern and extension-abduction-internal rotation.
- The second diagonal (D2): Flexion-abduction-internal rotation pattern and extension-adduction-external rotation.
Please note that every flexion pattern is accompanied by ankle dorsiflexion + toes extension and extension pattern is accompanied by ankle planterflexion + toes flexion. Also, subtalar movements depends on the desired pattern contains hip adduction or abduction. Subtalar eversion is associated hip abduction and subtalar inversion is associated with hip abduction.
Patterns of scapula and pelvis[2]
Girdles in the human body are the proximal articulations of the extremities with the trunk. Pelvic girdles are the links between lower extremities and the trunk while scapulae link upper extremities with the trunk. Girdle patterns can be performed independently or in conjunction with the upper extremity or trunk patterns.
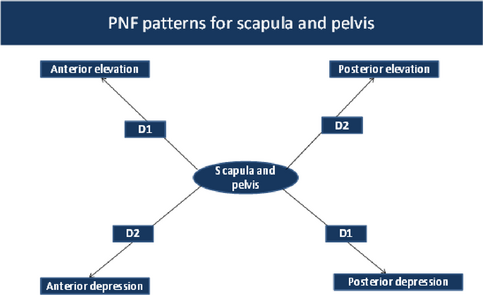
Scapula
Scapula D1 consists of the anterior elevation pattern -in which scapula moves up towards one's ear and front (mix of upward rotation, abduction and protraction)- and posterior depression pattern in which scapula moves down and back (mix of downward rotation, adduction and retraction).
The anterior elevation occurs with Flexion-adduction-external rotation gleno-humeral pattern while posterior depression occurs with extension-abduction-internal rotation gleno-humeral pattern.
Scapula D2 constitutes the posterior elevation pattern -in which scapula moves up towards one's ear and back (mix of upward rotation, adduction and retraction)- and anterior depression pattern -in which scapula moves down and front (mix of downward rotation, abduction and protraction).
The posterior elevation occurs with Flexion-abduction-external rotation gleno-humeral pattern while anterior depression occurs with extension-adduction-internal rotation gleno-humeral pattern.
Scapula articulates with the humerus and thoracic cage, scapula muscles are attached to humerus and spine. That's why scapula movements can occur with upper trunk or upper extremities movements.
Pelvis
Pelvis D1 consists of the anterior elevation pattern in which one side of pelvis moves up and front towards trunk and posterior depression pattern in which pelvis side moves down and back.
Pelvis D2 consists of the posterior elevation pattern in which one side of pelvis moves up and front towards trunk and anterior depression pattern in which pelvis side moves down and back.
In contrast to Scapular diagonals, pelvis patterns don't correspond directly with lower extremities patterns because their motions depend on trunk muscle actions primarily not lower extremities muscles.
Second: Bilateral patterns[2]
Four main combinations can be used if we want to engage both upper extremities or both lower extremities[2]:
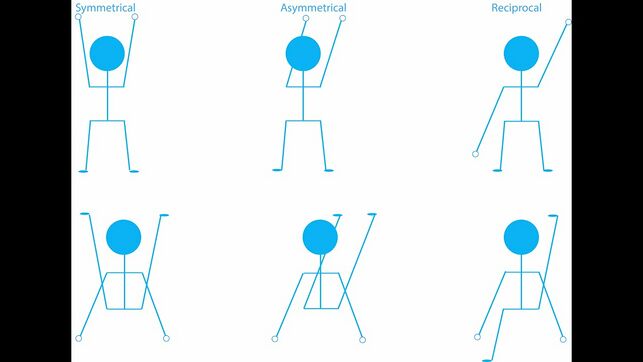
Symmetrical: We instruct the individual to perform same pattern on both limbs e.g. flexion-adduction-external rotation for both upper extremities.
Asymmetrical: We inform the trainee to perform a certain pattern of a diagonal at one limb and perform another pattern on the other limb in the same direction of the first from the other diagonal e.g. flexion adduction external rotation and flexion abduction external rotation.
Reciprocal symmetrical: We teach the person to do a pattern in one limb from a diagonal by one limb and do the opposite pattern of the same diagonal by the other limb e.g. flexion-adduction-internal rotation and extension-abduction-internal rotation.
Reciprocal asymmetrical: The patient do a pattern in one limb and opposes the pattern that is in the same direction of the first but from the other direction e.g. flexion -adduction-external rotation and extension-adduction-internal rotation.
Patterns of the trunk[edit | edit source]
For trunk movements, bilateral extremities patterns are performed in asymmetrical maneuvers "Check previous section - bilateral patterns" to engage the spinal rotation. Patterns of trunk movements are exclusive into:
- flexion with right rotation
- extension with left rotation
- flexion with left rotation
- extension with right rotation
When both upper extremities move into flexion, this encourages upper trunk extension and the reverse is true while in case of movements of lower extremities into flexion, the lower trunk moves into flexion and vice versa.
Third: PNF techniques[edit | edit source]
1. Agonistic techniques:
- Rhythmic initiation.
- Repeated contractions (from the beginning or throughout the range).
- Combinations of isotonics.
- Replication.
2. Antagonistic techniques:
- Rhythmic stabilization.
3. Relax techniques:
Intended goals for using techniques:[2]
Facilitating motion initiation
- Rhythmic initiation
- Repeated stretch from the beginning of the range.
Learning a motion
- Rhythmic initiation
- Combination of isotonics
- Repeated contractions
- Replication
Changing rate of motion
- Rhythmic initiation
- Reversals
- Repeated contractions
Increasing strength
- Combination of isotonics
- Reversals
- Rhythmic stabilization
- Repeated contractions
Increasing stability
- Combination of isotonics
- Reversals
- Rhythmic stabilization
Increase coordination and control
- Combination of isotonics
- Rhythmic initiation
- Reversals
- Rhythmic stabilization
- Repeated contractions
- Replication
Increase endurance
- Reversals
- Rhythmic stabilization
- Repeated contractions
Increase ROM
- Reversals
- Rhythmic stabilization
- Repeated contractions
- Contract–relax
- Hold–relax
Relaxation
- Rhythmic initiation
- Rhythmic stabilization
- Hold–relax
Decrease pain
- Rhythmic stabilization
- Reversals
- Hold–relax
Research Evidence[edit | edit source]
- Hip-flexion ROM[16]: Level 2 evidence Both of PNF stretching and static stretching are effective in increasing muscle extensibility and increasing hip flexion ROM.
- Adhesive-capsulitis[17]: PNF is superior than conventional physical therapy in decreasing pain and reducing disability, increasing ROM, improving function.
- Parkinson's disease[1]: PNF is similar or superior to other therapies related to gait speed.
- Stroke: PNF is an effective treatment for the improvement of gait parameters in patients with stroke.
- Low Back pain (LBP)[18] [19]: Low to moderate evidence for PNF for decreasing pain and improving disability in patients with LBP whether in the short term (4 to 8 weeks of intervention) or at 12-week follow-up.
- Other conditions.[20]
References[edit | edit source]
- ↑ 1.0 1.1 Alexandre de Assis IS, Luvizutto GJ, Bruno ACM, Sande de Souza LAP. The Proprioceptive Neuromuscular Facilitation Concept in Parkinson Disease: A Systematic Review and Meta-Analysis. Journal of Chiropractic Medicine [Internet]. 2020 Sep;19(3):181–7. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7750824/
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Adler SS, Beckers D, Buck M. PNF in practice : an illustrated guide. Heidelberg: Springer Medizin Verlag; 2014.
- ↑ Byrne JH. Chapter 16 - Postsynaptic Potentials and Synaptic Integration [Internet]. Byrne JH, Heidelberger R, Waxham MN, editors. From molecules to networks: an introduction to cellular and molecular neuroscience. ScienceDirect. Boston: Academic Press; 2014 [cited 2023 May 9]. p. 489–507. Available from: https://www.sciencedirect.com/science/article/abs/pii/B9780123971791000166
- ↑ Heckman CJ, Hyngstrom AS, Johnson MD. Active properties of motoneurone dendrites: diffuse descending neuromodulation, focused local inhibition. The Journal of Physiology. 2008 Feb 29;586(5):1225–31.
- ↑ Jo D. Shoulder PNF Pattern D1 - Ask Doctor Jo [Internet]. www.youtube.com. 2016 [cited 2023 Nov 25]. Available from: https://www.youtube.com/watch?app=desktop&v=ALbNYfjKWUg
- ↑ Moreira R, Lial L, Teles Monteiro MG, Aragão A, Santos David L, Coertjens M, et al. Diagonal movement of the upper limb produces greater adaptive plasticity than sagittal plane flexion in the shoulder. Neuroscience Letters. 2017 Mar;643:8–15.
- ↑ PNF (Proprioceptive Neuromuscular Facilitation) for the Upper Extremity [Internet]. www.youtube.com. [cited 2023 Dec 1]. Available from: [https://www.youtube.com/watch?v=lDwG4zFBWr4&t=13s https://www.youtube.com/watch?v=lDwG4zFBWr4 ]
- ↑ Stephanie. Proprioception [Internet]. Post-Stroke Impairments and Interventions. Available from: https://stroketherapyreference.weebly.com/proprioception.html
- ↑ PNF (Proprioceptive Neuromuscular Facilitation) for the Lower Extremity [Internet]. www.youtube.com. [cited 2023 Dec 1]. Available from: https://www.youtube.com/watch?v=RvhJR9NJhks
- ↑ Chaturvedi P. PNF in acute stroke. MOJ Anatomy & Physiology [Internet]. 2018 Nov 27;5(6). Available from: https://medcraveonline.com/MOJAP/MOJAP-05-00232.pdf
- ↑ PNF (Proprioceptive Neuromuscular Facilitation) for the Pelvis [Internet]. www.youtube.com. [cited 2023 Dec 1]. Available from: https://www.youtube.com/watch?v=Rm8fsOYQ_1c
- ↑ PNF (Proprioceptive Neuromuscular Facilitation) for the Scapula [Internet]. www.youtube.com. [cited 2023 Dec 1]. Available from: https://www.youtube.com/watch?v=GDqbuj_q6wE&t=8s
- ↑ PNF Patterns [Internet]. www.youtube.com. 2021 [cited 2023 Nov 26]. Available from: https://www.youtube.com/watch?v=6qmINzUhW8A
- ↑ Trunk PNF Pattern | Upper and Lower Trunk PNF [Internet]. www.youtube.com. [cited 2023 Dec 1]. Available from: https://www.youtube.com/watch?v=oJl5jaQn0p0
- ↑ PNF lower trunk [Internet]. www.youtube.com. [cited 2023 Dec 1]. Available from: https://www.youtube.com/watch?app=desktop&v=yuWb9oEdeZk
- ↑ Lempke L, Wilkinson R, Murray C, Stanek J. The Effectiveness of PNF Versus Static Stretching on Increasing Hip-Flexion Range of Motion. Journal of Sport Rehabilitation. 2018 May;27(3):289–94.
- ↑ Tedla JS, Sangadala DR. Proprioceptive neuromuscular facilitation techniques in adhesive capsulitis: a systematic review and meta-analysis. Journal of Musculoskeletal & Neuronal Interactions [Internet]. 2019;19(4):482–91. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6944810/
- ↑ Arcanjo FL, Martins JVP, Moté P, Leporace G, Oliveira DA de, Sousa CS de, et al. Proprioceptive neuromuscular facilitation training reduces pain and disability in individuals with chronic low back pain: A systematic review and meta-analysis. Complementary Therapies in Clinical Practice. 2022 Feb;46(101505):101505.
- ↑ Gao P, Tang F, Liu W, Mo Y. The effects of proprioceptive neuromuscular facilitation in treating chronic low back pain: A systematic review and meta-analysis. Journal of Back and Musculoskeletal Rehabilitation. 2021 Jul 1;35(1):1–13.
- ↑ Smedes F, Heidmann M, Schäfer C, Fischer N, Stępień A. The proprioceptive neuromuscular facilitation-concept; the state of the evidence, a narrative review. Physical Therapy Reviews. 2016 Jan 2;21(1):17–31.






