Valsalva Test
Introduction[edit | edit source]
Valsalva maneuver VM non-invasive test was described for the first time by Antonio Maria Valsalva an Italian anatomist, physician, and surgeon in 1704. It was first used in otolaryngology, in 1851 was used for the cardiovascular purpose for the first time by Edward Weber so it sometimes named Valsalva- Edward maneuver.
Valsalva maneuver is a forced expiration against a closed glottis, associated with an increase in the intrathoracic and intra-abdominal pressure. It is simple but associated with complex cardiovascular changes, controlling the arterial blood pressure was one of the first aims as it is affected by signals of the baroreceptor[1].
The maneuver/ test may be associated with signs during applications most are visible for example; blushing, headache, dizziness, jugular vein distension. special care should be taken when dealing with a patient having a history of coronary artery disease, congenital heart disease, intraocular lens implantation as there is an increase in intra-ocular and intra-abdominal pressure.
Purpose[edit | edit source]
Valsalva test is used widely with different specialties and has different instruments and different applications according to the field and the target it is used for.
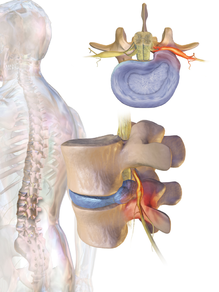
- Neurological cases, lumbar and cervical radiculopathy, the test is associated with an increase in intrathoracic pressure, and a slight increase in the intraspinal pressure cause radicular pain exacerbation, which may indicate the nerve is compressed by an intervertebral disc or nearby anatomy[3].
- Women health is used as a urodynamic test for assessment of pelvic organ prolapse, and urinary incontinence to assess sphincter function by using valsalva leak pressure point, that indicates the pressure at which urine leakage occurs.
- As a diagnostic and treatment maneuver for cardiovascular disease, diagnosis of heart abnormalities specifically with using ECG. heart murmurs, a marker to heart failure, and treatment for supraventricular tachycardia carried at clinical labs with precautions and emergency equipment[4].
- Normalize middle ear pressure, during the hyperbaric oxygen therapy to protect middle ear trauma[5].
Technique[edit | edit source]
There are various descriptions for this test to carry depending on the target and the condition it is used for, the patient can perform it from sitting, supine, or semi-recumbent position, but sitting is the preferred position.
First take a normal, deep breath, hold the breath, close your glottis, then exhale against your closed glottis (close your nose and mouth) or as bearing down.
It is done for 10-15 seconds followed by normal breathing.
The test is positive if there is radicular pain exacerbate in the upper or the lower limb in neurological conditions.
A manometer with pressure 40mmHg is used during autonomic dysfunction evaluation when continuous heart rate and blood pressure monitoring is important.
When it is carried to assess the pelvic prolapse it is done during imaging, at this situation valsalvometer[7], or sphygmomanometer is used to better understand the maneuver, the patient blowing into a restricted flow tube starts with pressure 30–40 cm H2O, the prolapse depends on the duration the test is last and the repitition[8]
Evidence[edit | edit source]
With radiculopathy diagnosis. the test shows low sensitivity 22 %, and high specificity 94 %[10], negative likelihood ratios -LR .83, positive likelihood ratios +LR 3.5[11].
To diagnosis heart failure the Valsalva test has 86% sensitivity, 54% specificity, and a positive likelihood ratio 1.86 when compared with electrocardiography. In addition, 100% sensitivity, 64% specificity, and a positive likelihood ratio 2.8 when compared with NT-proBNP ( a blood test for a protein produced in large amounts by heart)[12]
References[edit | edit source]
- ↑ Pstras L, Thomaseth K, Waniewski J, Balzani I, Bellavere F. The Valsalva manoeuvre: physiology and clinical examples. Acta physiologica. 2016 Jun;217(2):103-19.
- ↑ Air to air. Valsalva maneuver. Available from: http://www.youtube.com/watch?v=fifcKrM9SBg[last accessed 13/2/2020]
- ↑ Iyer S, Kim HJ. Cervical radiculopathy. Current reviews in musculoskeletal medicine. 2016 Sep;9(3):272-80.
- ↑ Junqueira Jr LF. Teaching cardiac autonomic function dynamics employing the Valsalva (Valsalva-Weber) maneuver. Advances in Physiology Education. 2008 Mar;32(1):100-6.
- ↑ Lima MA, Farage L, Cury MC, Bahmad Jr F. Middle ear barotrauma after hyperbaric oxygen therapy-the role of insuflation maneuvers. Int Tinnitus J. 2012 Jun 1;17(2):180-5.
- ↑ JClinical Examination Videos. Valsalva manoeuvre. Available from: http://www.youtube.com/watch?v=mViHwWXNyj0[last accessed 13/2/2020]
- ↑ Greenland HP, Hosker GL, Smith AR. A valsalvometer can be effective in standardising the Valsalva manoeuvre. International Urogynecology Journal. 2007 May;18(5):499-502.
- ↑ Mulder FE, Shek KL, Dietz HP. What's a proper push? T he V alsalva manoeuvre revisited. Australian and New Zealand Journal of Obstetrics and Gynaecology. 2012 Jun;52(3):282-5
- ↑ SparkBio. Valsalva Maneuver. Available from: http://www.youtube.com/watch?v=Wfka6tTad64[last accessed 15/2/2020]
- ↑ Rubinstein SM, Pool JJ, Van Tulder MW, Riphagen II, De Vet HC. A systematic review of the diagnostic accuracy of provocative tests of the neck for diagnosing cervical radiculopathy. European spine journal. 2007 Mar;16(3):307-19.
- ↑ Wainner RS, Fritz JM, Irrgang JJ, Boninger ML, Delitto A, Allison S. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine. 2003 Jan 1;28(1):52-62.
- ↑ Liniado GE, Beck MA, Gimeno GM, González AL, Cianciulli TF, Castiello GG, Gagliardi JA. Clinical examination and the Valsalva maneuver in heart failure. Medicina. 2018 Jan 1;78(3):163-70.