Peripheral Sensitisation
Original Editor - Michelle Lee
Top Contributors - Michelle Lee, Shaimaa Eldib, Melissa Coetsee, Admin, Jo Etherton, Bruno Serra, Khloud Shreif and Mathius Kassagga
Introduction[edit | edit source]
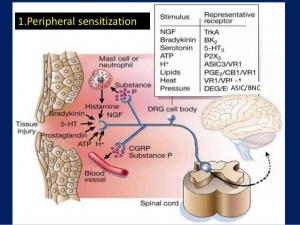
Peripheral sensitisation refers to sensitisation of the nociceptive system in the periphery. It is characterised by an increased responsiveness and reduced threshold of nociceptive neurons to stimulation of their receptive fields.[1]
Physiological Mechanisms of Peripheral Sensitisation[edit | edit source]
Following an injury or tissue damage, sensitisation of the affected area occurs to help with healing by initiating behaviours that would prevent further injury (eg. guarding). The mechanisms that sensitise the nociceptive system operate both in the periphery (leading to primary hyperalgesia) and the central nervous system (leading to secondary hyperalgesia and allodynia).[1]
| Primary hyperalgesia | Secondary hyperalgesia | |
|---|---|---|
| Area affected | Localised to the area of tissue damage or nerve distribution | Occurs in healthy skin next to or further away from the injury site |
| Description | Heightened sensitivity to heat and mechanical stimulation in the area of damage | Heightened sensitivity to mechanical stimuli |
| Mechanism | Peripheral sensitisation | Central sensitisation |
Peripheral sensitisation is an increased sensitivity to an afferent nerve stimulus. This occurs after there has been an injury or cell damage to the area, and produces a flare response due to nociceptors producing lots of neuropeptides, which results in an increased sensitivity to heat and touch stimuli. If noxious stimuli are more painful than before, primary hyperalgesia is present. [4][5] The mechanisms responsible for this response are explained below:
Up-regulation of existing receptors:[edit | edit source]
This can occur as a result of inflammation. Chemical mediators of inflammation (such as histamine, bradykinin, prostaglandins) and neuropeptide (Substance P) are released following tissue damage and can stimulate the nociceptive receptors, making them depolarize, and sensitize them (bringing the membrane potential closer to the depolarization threshold). Receptors are sensitised by up-regulation of the ion-channels (influenced by the protein enzyme cascade), which makes them more sensitive to chemical mediators. This results in a lowered activation threshold (more sensitive to the same quantity of chemical mediators) and results in peripheral sensitisation.[4][6][7]The accumulation of 'inflammatory soup' of chemicals at the site of injury produces the characteristic signs of inflammation (redness, swelling and pain).[1]
In summary, the nociceptor terminals become more sensitive to the same quantity of the chemical mediators.
Up-regulation of new receptors:[edit | edit source]
Activation of silent nociceptors increases the nociceptive receptor field.
The cell body which is located in the dorsal root ganglia sensory nerves produces protein channels and transmits signals to the nociceptive terminals. When there is inflammation present as described above, the Nerve Growth Factor is produced which transmits up to the cell body in the dorsal root ganglia. This then also stimulates the production of ions, which as described above, stimulates the receptors on the nociceptive terminals. Now the nociceptive terminals have a greater quantity of the 'chemical mediators' stimulating the sensation of pain more frequently.
Comparison with Central Sensitisation[edit | edit source]
The difference between central and peripheral sensitisation can be identified quite easily, as peripheral sensitisation becomes heat-sensitive whereas central sensitisation does not. Lorimer Moseley explains this in more detail in the video below.[4][8]The table below also summarises some of the differences between central and peripheral sensitisation. Bear in mind that is possible for both to co-exist.
| Peripheral Sensitisation | Central Sensitisation | |
|---|---|---|
| Pathophysiology | Increased responsiveness and lowered firing thresholds of peripheral nociceptors; activation of silent nociceptors | Sensitisation occurs at the spinal cord level, resulting in increased receptor field size and increased responsiveness/lowered threshold to noxious and non-noxious stimuli |
| Clinical features | Primary hyperaglesia
Redness and swelling Heat hyperalgesia |
Secondary hyperalgesia
Allodynia Diffuse, widespread pain (non dermatomal) Temporal summation |
| Treatment | Responsive to NSAIDs | More responsive to anti-epileptic or anti-depressant medications |
Pathological Peripheral Sensitisation[edit | edit source]
Hypersensitivity following an injury is an important self-preservation mechanism, which allows the injured tissue to heal and to continuously warn/remind the brain to avoid further injury to this area. Peripheral sensitisation is therefore a normal, protective process, and should resolve as damaged tissue heals. When this hypersensitivity becomes prolonged, it provides the body with no benefit. Sustained peripheral sensitisation can be influenced by[11]:
- Prolonged nociceptive input and or continued peripheral pathology
- Central mechanisms maintaining peripheral nociceptive mechanisms (eg impaired inhibition of pain)
- Neurogenic inflammation which can result in continued activation of nociceptors
- Neuropathic pain mechanisms resulting in spontaneous firing in nerves
- Continued inflammatory processes
It is important to identify peripheral sensitisation in patients as it will have an impact on treatment and their experience of pain. For example, assessment through touch or movement may stimulate an unexpected level of pain. [12]
Clinical findings[edit | edit source]
The following signs indicate that peripheral sensitisation is likely present[11]:
- Distribution of symptoms is within a discreet area of tissue damage
- Hyperalgesia at or close to the site of tissue damage
- Pain described as burning or deep and achy
- Pain worsens with heat
- Pain often present at night
- Quantitative sensory testing will reveal increased sensitivity to heat and reduced pain pressure threshold at the injury site
Management[edit | edit source]
In order to prevent the nociceptive processes of peripheral sensitisation from becoming chronic, pain needs to be addresses early. Ice and NSAIDs can help to reduce inflammatory mediators (especially if excessive). Immobilisation and the use of assistive devices can be very useful in the acute stages of injury to 'calm' the peripheral nociceptive processes. When peripheral sensitisation is present long after tissue healing has occurred, a multidisciplinary approach to pain management will be required. Refer to the following pages for more guidance: Central sensitisation, Neuropathic pain, Pain mechanisms, Quantitative Sensory Testing.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Johnson MI. The physiology of the sensory dimensions of clinical pain. Physiotherapy. 1997 Oct 1;83(10):526-36.
- ↑ Hsieh MT, Donaldson LF, Lumb BM. Differential contributions of A- and C-nociceptors to primary and secondary inflammatory hypersensitivity in the rat. Pain. 2015 Jun;156(6):1074-1083. doi: 10.1097/j.pain.0000000000000151. PMID: 25760474; PMCID: PMC4535358.
- ↑ Pezet S, McMahon SB. Neurotrophins: mediators and modulators of pain. Annu. Rev. Neurosci.. 2006 Jul 21;29:507-38..
- ↑ 4.0 4.1 4.2 Bolay H, Moskowitz MA. Mechanisms of pain modulation in chronic syndromes. Neurology. 2002 Sep 10;59(5 suppl 2):S2-7.
- ↑ Graven-Nielsen T, Arendt-Nielsen L. Peripheral and central sensitization in musculoskeletal pain disorders: an experimental approach. Current rheumatology reports. 2002 Aug 1;4(4):313-21.
- ↑ Staud R, Smitherman ML. Peripheral and central sensitization in fibromyalgia: pathogenetic role. Current pain and headache reports. 2002 Aug 1;6(4):259-66.
- ↑ Van Griensven H, Strong J, Unruh A. Pain: a textbook for health professionals. Churchill Livingstone; 2013 Nov 1.
- ↑ Mizumura KA. Peripheral mechanism of hyperalgesia-sensitization of nociceptors. Nagoya journal of medical science. 1997 Nov 1;60:69-88.
- ↑ Laree Draper. Lorimer Moseley Pain DVD Sensitivity to Heat, Peripheral Sensitization. Available from: http://www.youtube.com/watch?v=VmQT5NgsUdc[last accessed 20/8/2021]
- ↑ Dr Matt & Dr Mike. Chronic Pain and Sensitisation. Available from: http://www.youtube.com/watch?v=rxl6c8UwmKs[last accessed 20/8/2021]
- ↑ 11.0 11.1 Parker,R & Bolton, B. Principles of Pain (Module 1) (unpublished lecture notes). Train Pain Academy, South Africa; lecture given 2017 July.
- ↑ Van Griensven H, Strong J, Unruh A. Pain: a textbook for health professionals. Churchill Livingstone; 2013 Nov 1.