Dysphagia Rehabilitation Management: Difference between revisions
No edit summary |
No edit summary |
||
| (One intermediate revision by the same user not shown) | |||
| Line 137: | Line 137: | ||
== Diet == | == Diet == | ||
The International Dysphagia Diet Standardisation Initiative Functional Diet Scale (IDDSI) is a reliable scale for clinicians to "capture diet texture restriction and progression in people with dysphagia."<ref>Steele CM, Namasivayam-MacDonald AM, Guida BT, Cichero JA, Duivestein J, Hanson B, Lam P, Riquelme LF. [https://pdf.sciencedirectassets.com/272381/1-s2.0-S0003999317X00063/1-s2.0-S0003999318300856/main.pdf?X-Amz-Security-Token=IQoJb3JpZ2luX2VjEAIaCXVzLWVhc3QtMSJGMEQCIFS06Z25JFz6kurfEcFjiUM5AuiDtIEavNkLLCq%2Bt2yMAiAP%2FA2MRpKYmyNN9fB6RIfRKUhJS9NXtykhk9Oy7dRHVCq8BQi6%2F%2F%2F%2F%2F%2F%2F%2F%2F%2F8BEAUaDDA1OTAwMzU0Njg2NSIMSq4pHeWmCoiJ%2BGMCKpAFPPnsJ63cVRYqI3l5ZDOir1aFYJ%2F7jVGtp6O3VGYtOJ8SQV8i51K2TVVphnc2wja2LHNjQjrKtLC%2Bu0plmgqwlLsS3OUEg4HWN7qnR3Xb1xh86i%2FbjVWkPuiM3nkZ7%2FBPk7wRk5uKOcRjs1BujCEbwFkwNvFOXSEb9h37S2BvNgCEH6e%2BKpSfGXRcUzt1NI%2FOEueRAqWu49Zi7Jh7JBc2ZVZPAL4DhOmj1sNLx1yfu5kBoFGLXcLYR6t0wxbwKzUNLhruaBIgQxUof0ivPIis1y5SerCG71RyBUkewY0j4xa9I1M%2BP6w%2B2ypJK1FThNg%2BsxB96OrYgOg%2FZCvwq%2BfpaoAat3SMK9mNYVk9WvIZo3YtD%2FqvFcAgfuN91yY4PFgXJYSC27PmMYO2%2BHAg%2B1tMoOMUm3MB0mHW%2FMcxJzXDeDvbGnOHZIU7Un7eIxWSEYHWcO2H3aXB3TvBXIvOS2nphXdu1KQ8r%2F1w6jAGZBrtQO0zFoBr2o%2Bb0cmVk6b%2FZeHnHxtVI3EfSe0Egjtdm%2FcEuOd8I%2Ff5VS6hiuz9awrn8zLTKGuR4g%2Fthniz0JQxQ0Il5vVYk5bIKGDkW9lZKtrtDKtysvzT9Xe2DUieoMsKQSJuqxBhkc39fomomNf5jb7cgelm259tncZtDeAszlKbP4LJsnNN4LvPs6vkjlLOWHo7InI8BKGiEjtra%2BKPT0ZO4lSBLf4VQ10LBXdDWT%2BDKBE3BA0CrASz8Rc6vmJGbR5cKuvdtM7qjkBxxHWZcLhLV3DSPTccj8k1Iy63gZqI2pCTmdZlpKBGAeuycQ%2FsDhlEN2quwKf1crfNVgHuVRdOjv1%2FoNZmpFIetAM4OvyJHzAtSFkyT89RkpSOBnEC2gYw1u6etAY6sgF%2BqsgOyxmrnHEgkeZQ7oivYW7Fl%2FCDrWBzJlSnh6P1eUf9BogWmcEtsxKGZ139s9v19eWX1wlD4TVOrl8w%2FoJMIOSHxYgZFyMz7c%2Bvs9EOkA%2Fq13islcuhqSM9TdmLufewThhN0C5lYfRp5095tfGE4J980566e3a3%2BspG2UTnxEuCW4IBmdcA6P4vZkXJPqSN4r4FjJ9xngg%2B8gUx9LY4PNAdgCwZhDZ4MIW%2FouD2jPD1&X-Amz-Algorithm=AWS4-HMAC-SHA256&X-Amz-Date=20240705T095503Z&X-Amz-SignedHeaders=host&X-Amz-Expires=300&X-Amz-Credential=ASIAQ3PHCVTYWBG3X7MF%2F20240705%2Fus-east-1%2Fs3%2Faws4_request&X-Amz-Signature=77cd257804ebc4ca1997664b6a731261856509f94fc33c91aa1c3ec835926b05&hash=2a8dee0e7544e57f8ccd705b46fce1a7915281a3f2917d87086b482d5fb0329a&host=68042c943591013ac2b2430a89b270f6af2c76d8dfd086a07176afe7c76c2c61&pii=S0003999318300856&tid=spdf-439ac6e2-e880-4eaf-a39c-ae506fbc7653&sid=b645a1f57e8a2346cd184c0846d63b1d05f1gxrqb&type=client&tsoh=d3d3LnNjaWVuY2VkaXJlY3QuY29t&ua=0a025f5b0055510e5d02&rr=89e67a2a59cec3ce&cc=pl Creation and initial validation of the international dysphagia diet standardisation initiative functional diet scale.] Archives of physical medicine and rehabilitation. 2018 May 1;99(5):934-44.</ref> IDDSI describes and categorises foods and drinks according to their texture or flow characteristics. The degree of diet texture restriction must be recommended for a patient based on assessment by a '''qualified clinician.''' | <blockquote>"Dietary modification—altering the consistency of foods and liquids—is a fundamental aspect of dysphagia management."<ref name=":7" /></blockquote>The International Dysphagia Diet Standardisation Initiative Functional Diet Scale (IDDSI) is a reliable scale for clinicians to "capture diet texture restriction and progression in people with dysphagia."<ref name=":7">Steele CM, Namasivayam-MacDonald AM, Guida BT, Cichero JA, Duivestein J, Hanson B, Lam P, Riquelme LF. [https://pdf.sciencedirectassets.com/272381/1-s2.0-S0003999317X00063/1-s2.0-S0003999318300856/main.pdf?X-Amz-Security-Token=IQoJb3JpZ2luX2VjEAIaCXVzLWVhc3QtMSJGMEQCIFS06Z25JFz6kurfEcFjiUM5AuiDtIEavNkLLCq%2Bt2yMAiAP%2FA2MRpKYmyNN9fB6RIfRKUhJS9NXtykhk9Oy7dRHVCq8BQi6%2F%2F%2F%2F%2F%2F%2F%2F%2F%2F8BEAUaDDA1OTAwMzU0Njg2NSIMSq4pHeWmCoiJ%2BGMCKpAFPPnsJ63cVRYqI3l5ZDOir1aFYJ%2F7jVGtp6O3VGYtOJ8SQV8i51K2TVVphnc2wja2LHNjQjrKtLC%2Bu0plmgqwlLsS3OUEg4HWN7qnR3Xb1xh86i%2FbjVWkPuiM3nkZ7%2FBPk7wRk5uKOcRjs1BujCEbwFkwNvFOXSEb9h37S2BvNgCEH6e%2BKpSfGXRcUzt1NI%2FOEueRAqWu49Zi7Jh7JBc2ZVZPAL4DhOmj1sNLx1yfu5kBoFGLXcLYR6t0wxbwKzUNLhruaBIgQxUof0ivPIis1y5SerCG71RyBUkewY0j4xa9I1M%2BP6w%2B2ypJK1FThNg%2BsxB96OrYgOg%2FZCvwq%2BfpaoAat3SMK9mNYVk9WvIZo3YtD%2FqvFcAgfuN91yY4PFgXJYSC27PmMYO2%2BHAg%2B1tMoOMUm3MB0mHW%2FMcxJzXDeDvbGnOHZIU7Un7eIxWSEYHWcO2H3aXB3TvBXIvOS2nphXdu1KQ8r%2F1w6jAGZBrtQO0zFoBr2o%2Bb0cmVk6b%2FZeHnHxtVI3EfSe0Egjtdm%2FcEuOd8I%2Ff5VS6hiuz9awrn8zLTKGuR4g%2Fthniz0JQxQ0Il5vVYk5bIKGDkW9lZKtrtDKtysvzT9Xe2DUieoMsKQSJuqxBhkc39fomomNf5jb7cgelm259tncZtDeAszlKbP4LJsnNN4LvPs6vkjlLOWHo7InI8BKGiEjtra%2BKPT0ZO4lSBLf4VQ10LBXdDWT%2BDKBE3BA0CrASz8Rc6vmJGbR5cKuvdtM7qjkBxxHWZcLhLV3DSPTccj8k1Iy63gZqI2pCTmdZlpKBGAeuycQ%2FsDhlEN2quwKf1crfNVgHuVRdOjv1%2FoNZmpFIetAM4OvyJHzAtSFkyT89RkpSOBnEC2gYw1u6etAY6sgF%2BqsgOyxmrnHEgkeZQ7oivYW7Fl%2FCDrWBzJlSnh6P1eUf9BogWmcEtsxKGZ139s9v19eWX1wlD4TVOrl8w%2FoJMIOSHxYgZFyMz7c%2Bvs9EOkA%2Fq13islcuhqSM9TdmLufewThhN0C5lYfRp5095tfGE4J980566e3a3%2BspG2UTnxEuCW4IBmdcA6P4vZkXJPqSN4r4FjJ9xngg%2B8gUx9LY4PNAdgCwZhDZ4MIW%2FouD2jPD1&X-Amz-Algorithm=AWS4-HMAC-SHA256&X-Amz-Date=20240705T095503Z&X-Amz-SignedHeaders=host&X-Amz-Expires=300&X-Amz-Credential=ASIAQ3PHCVTYWBG3X7MF%2F20240705%2Fus-east-1%2Fs3%2Faws4_request&X-Amz-Signature=77cd257804ebc4ca1997664b6a731261856509f94fc33c91aa1c3ec835926b05&hash=2a8dee0e7544e57f8ccd705b46fce1a7915281a3f2917d87086b482d5fb0329a&host=68042c943591013ac2b2430a89b270f6af2c76d8dfd086a07176afe7c76c2c61&pii=S0003999318300856&tid=spdf-439ac6e2-e880-4eaf-a39c-ae506fbc7653&sid=b645a1f57e8a2346cd184c0846d63b1d05f1gxrqb&type=client&tsoh=d3d3LnNjaWVuY2VkaXJlY3QuY29t&ua=0a025f5b0055510e5d02&rr=89e67a2a59cec3ce&cc=pl Creation and initial validation of the international dysphagia diet standardisation initiative functional diet scale.] Archives of physical medicine and rehabilitation. 2018 May 1;99(5):934-44.</ref> IDDSI describes and categorises foods and drinks according to their texture or flow characteristics. The degree of diet texture restriction must be recommended for a patient based on assessment by a '''qualified clinician.''' The IDDSI framework consists of 8 levels, represented by 2 intersecting pyramids. The 0 and 7 levels constitute of unmodified drinks and foods: levels 0-4 correspond to drinks and levels 3-7 measure foods. The middle levels represent progressively greater degrees of texture modification'''.''' | ||
[[File:IDDSI Framework.jpeg|center|thumb|500x500px|The IDDSI framework. © The International Dysphagia Diet Standardisation Initiative 2019 @ [[/iddsi.org/framework/|https://iddsi.org/framework]]. Licensed under the [[/creativecommons.org/licenses/by-sa/4.0/legalcode|CreativeCommons Attribution Sharealike 4.0 License]]. Derivative works extending beyond language translation are NOT PERMITTED.]] | |||
Refer to the [https://iddsi.org/IDDSI/media/images/Complete_IDDSI_Framework_Final_31July2019.pdf IDDSI website] for a detailed descriptions of food textures and drink thickness and their testing methods. | |||
[http://www.rehab.go.jp/english/pdf/E30.pdf Dysphagia rehabilitation manual] published a dysphagia diet pyramid, based on the work by Kanaya et al.<ref>Fujishima, I. Rehabilitation for Swallowing Disorders Associated with Stroke; Ishiyaku Publishers, Inc.: Tokyo, Japan, 1993; pp. 81–86.</ref><ref>Matsuo K, Fujishima I. [https://www.mdpi.com/2072-6643/12/6/1613 Textural Changes by Mastication and Proper Food Texture for Patients with Oropharyngeal Dysphagia.] Nutrients. 2020; 12(6):1613.</ref> The 5-stage Seirei Dysphagia Diets consist of the following categories: | |||
* L0 is gelatin jelly (tea or fruit juice, etc.) | |||
* L1 is gelatin jelly (miso soup, milk, etc., containing protein) | |||
* L2 is gelatin jelly (mixer meal with gelatin) | |||
* L3 is a puréed or mixer meal | |||
* L4 is a softened diet | |||
The Dysphagia Diet Pyramid is known and used in Japan vs The International Dysphagia Diet Standardisation Initiative Functional Diet Scale (IDDSI) provides a common terminology to describe food textures and drink thickness. | |||
== Resources == | == Resources == | ||
* | *[http://www.ebrsr.com/sites/default/files/chapter%2015_v19.pdf Dysphagia rehabilitation] | ||
* | *[http://www.rehab.go.jp/english/pdf/E30.pdf Dysphagia rehabilitation manual] | ||
== References == | == References == | ||
<references />. | <references />. | ||
Latest revision as of 18:09, 5 July 2024
Original Editor - User Name
Top Contributors - Ewa Jaraczewska
Introduction[edit | edit source]
Positioning[edit | edit source]
Posture can affect swallowing and, in turn, can be affected by swallowing. A good understanding of the relationship between swallowing and posture is essential when managing patients with dysphagia.
Position during eating and drinking[edit | edit source]
Body position:
- 30 degrees reclining position:[1]
- raises the front of the oral cavity and lowers the back
- facilitates bringing a food bolus from the oral cavity to the throat for patients with difficulties sending a food bolus into the pharynx
- raises the respiratory tract and lowers the oesophagus making its easier to slide the bolus down the posterior wall of the pharynx, thus minimising aspiration.
- 60 degrees or higher position is needed for independent feeding[1]
- maintaining a seated position from 30 minutes[2] to 2 hours[3] after eating may prevent gastroesophageal reflux and reduce risk for aspiration
Chin tuck (chin down):[1]
- the chin down position may involve head flexion, neck flexion, or a combination of both
- the head flexion involving the upper cervical spine is effective when food residue is stuck in the epiglottic vallecula
- the neck flexion involving the middle and lower cervical spine is effective the initiation of swallowing reflex is poor.
- the effectiveness of each position should be verified by a Videofluoroscopic Swallowing Study or by a video-endoscopic examinations
Chin-up:[4]
- the chin-up posture involves the head and neck extension and lifting of the chin before initiation of the swallow.
- the head and neck extension facilitates posterior bolus transit using the force of gravity
- patient with reduction in base of tongue movements due to oral pain, mucositis, fibrosis caused by radiation, and chemoradiation and patients with prolonged oral transit time and reduced tongue strength may benefit from this posture [2]
- chin-up position is recommended only in patients with intact laryngeal and pharyngeal function
- chin-up position should be used with caution. Study by Lazarus et al.[5] has found that even in healthy subject, the chin-up posture presents a challenge as it alters the normal sequence of swallowing events and it is "necessary to further investigate how the chin-up posture affects the sequence of events of impaired swallows."[5]
Head rotation:
- the effect of head rotation on swallowing involves narrowing of the piriform on the side that was turned and expanding on the opposite side. This manoeuvre makes the food bolus to travel down the non-rotated side much easier [1]
- head rotation technique can benefit patients with the paralysis of the pharynx (bulbar paralysis as an example). It helps guiding a food bolus to the healthy side or less paralysed side.[1]
Head tilt:
- head tilt towards the stronger side is going to promote the diversion of the bolus to the stronger side. The force of gravity will help to bring a food bolus downward and pass through the non-paralysed side. [2][1]
Exercises[edit | edit source]
Dysphagia can be managed by improving oro-motor function which includes the function created by the movements of the mouth, tongue, jaw, and lips, oral motor skills such as swallowing, sucking, biting, chewing, and speaking functions, and the respiratory muscles strength training. [6][7]
The aim of exercises in dysphagia is to impact swallowing mechanics and impact bolus flow via compensatory strategies and rehabilitative exercise ( effortful swallow, supraglottic swallow, super-supraglottic swallow, and the Mendelsohn manoeuvre, or by improving swallowing physiology ( Shaker exercise). [8]
Guidelines for Exercises in Dysphagia[edit | edit source]
Determinants of dose for exercise prescriptions dysphagia should include: (1) duration or length of the programme, (2)intensity (% of max), (3)repetitions (number of actions per set), and (4) frequency (number of sets/day, number of days/week).[7]
Factors Affecting Outcomes[edit | edit source]
- poor compliance with swallow exercises reported with patients treated for head and neck cancer
- pre-treatment depression correlates with poor compliance with exercises
- timing and type of exercises. Lazarus et al.[5] found that one month post-radiotherapy for patients treated for head and neck cancer may be too soon to initiate a swallow therapy programme.
Outcome Measures[edit | edit source]
Outcome measures for each type of exercises are highly variable. When combination exercises are used the following outcome measures are recommended:[7]
- Functional Oral Intake Scale (FOIS)
- Penetration Aspiration Scale (PAS - measures changes on videofluoroscopy)
- Percutaneous endoscopic gastrostomy (PEG) tube dependence [9]
- Lingual pressure measurements [10]
- MD Anderson Dysphagia Inventory
Oro-Motor Exercises[edit | edit source]
- Mandible Exercises:[7]
- include jaw opening, jaw closing, and chin tuck against resistance (CTAR)[7]
- a systematic review of CTAR exercises by Park JS et al.[11] indicated, that CTAR exercise can selectively activate the suprahyoid muscle. Authors suggested that CTAR exercises are effective in improving swallowing function in patients with dysphagia [11]
- outcome measures consist of chin tuck strength, jaw opening strength, tongue strength, muscle volume, changes in videofluoroscopy parameters, body weight gain, Penetration Aspiration Scale (PAS) ratings laryngeal elevation and epiglottic closure
- recommended frequency: 3 times per day, 7 days per week [12]
- Lip muscle training:[2]
- protruding the lips while biting an ice cream stick to prevent jaw and teeth from moving
- lip rounding, such as if you are blowing a whistle or blowing on something hot
- treatment duration may range from 4 weeks to 6 months[7]
- Cheeks exercises:[2]
- puffing the cheeks
- Tongue exercises:[5]
- lingual range of motion, protrusion, lateralisation, elevation, and retraction towards the posterior pharyngeal wall
- isometric tongue exercises against resistance. Individuals press against a tongue depressor with their tongue in four directions: left, right, on protrusion, and on elevation, while resisting with the tongue depressor. Each press should be hold for 2 seconds
- a protocol by Lazarus et al.[5]sets the rules for the isometric tongue exercises to be performed 5 days a week for 6 weeks, and practiced five times per day with 10 repetitions per practice session
Oral-Motor Skills[edit | edit source]
- Vocalisation exercises
- voice training or vocal exercises focused on improving voice function were found to have a positive impact upon swallowing function[13]
- vocalisation exercises involving pronouncing letters of the alphabet can activate labial consonants (letters P and B), alveolar consonants (letters T and D), and palatal consonants (letters K and G) [2]
- outcome measures include Videofluoroscopic Dysphagia Scale (VDS), Speech Handicap Index-15 (SHI-15), Eating Assessment Tool-10 (EAT-10), Functional Oral Intake Scale (FOIS), and Quality of Life in Swallowing Disorders Questionnaire (SWAL-QOL) [13]
- A systematic review by Liu et al.[13]found a positive short term effect of voice training on swallowing in patients with neurological dysphagia (stroke) and non-neurological dysphagia (head and neck cancer), but the long term effects are unknown.
- Voice training can improve tongue strength leading to better control of the bolus and decrease bolus loss prematurely[14]
- Mendelsohn manoeuvre [2]
- The patient swallows the air which raises the larynx to the highest position. Next the patient holds this position for several seconds
- The goal is to enlarge the entrance of the oesophagus through a prolonged elevation of the larynx.
- Vocal fold adduction exercises:[2]
- the goal is to improve swallowing and reduce the risk of aspiration
- the patient is asked to clasp the palms together and press them against each other. While pressing the palms, the patient clears the voice by saying "ee" five times
- next, the patient is asked to repeat " ah", "ah", "ah" five times while maintaining the pressure
- the recommended frequency is five to ten times in one session repeated five times a day
- Shaker exercise:
- the goal of this exercise is to enlarge the entrance of the esophagus and strengthen the suprahyoid muscles[1]
- the patient is lying supine. Next, the patient is asked to lift the head up and holds it up for 1 minute, followed by a 1 minute rest. This sequence is repeated 3 times [1]
- the head up and down sequence is repeated 30 times[2]
- recommended frequency is 3 times a day for 6 weeks[1]
- Supraglottic swallow:[1]
- this training method can benefit patients who aspirate during swallowing
- the patient takes a deep breath, holds it, swallows a food bolus, and immediately clears the throat
- the effect of this exercise is based on the mechanism of holding one’s breath closes the glottis which prevents aspiration. Additionally coughing after swallowing removes any food from the respiratory tract.
- Super-supraglottic swallow:
- patient is instructed to “take a breath and hold it tightly while bearing down, continue to hold your breath and bear down as you swallow, immediately after your swallow (before you inhale) cough then immediately swallow hard again (before you inhale).”[15]
- Effortful swallow[2]
- the aim is to improve the posterior movement of the tongue
- the patient is asked to swallow by squeezing the neck and the throat muscles as hard as possible
Modalities and Devices[edit | edit source]
- Ice massage with a cold cotton bud targeting trigger point of swallowing reflexes, such as your soft palate, dorsum of the tongue. [2]
- Thermal tactile stimulation using a cold laryngeal mirror applied to the base of the arches. The mirror is rubbed up and down five times. Special training to perform this stimulation is required.[2]
- Passy Muir® Valve improves cough, decrease secretions, and reduce aspiration. [16] It can be used by clinicians other than speech therapists after passing a competency training.
Respiratory Training[edit | edit source]
Respiratory Muscle Strength Training
- The goal is to increase respiratory muscle strength as respiration and swallowing actions are highly coordinated. [7]
- The choice between inspiratory vs expiratory muscle strength training depends on the outcome desired.[17] Example: A patient with Parkinson's disease presenting with difficulty with breathing, swallowing, and cough production will benefit from increasing expiratory muscle force generation. [17]
- Outcome measures include the Penetration Aspiration Scale (PAS), Modified Barium Swallow Impairment Profile, Swallowing Quality of Life questionnaire (SWAL-QOL). [7]
- The recommended exercise frequency is 5 time a day for 5 days per week. [7]
The Respiratory Muscle Training article discusses different methods of respiratory muscle training.
Sputum discharge maneuver [1]
- The most common technique to assist with removing secretions trapped in the central respiratory tract
- The technique is based on exhaling very quickly and with strength while the glottis is open (huffing), then huffing once or twice after breathing in (forced expiratory maneuver ), and finished by coughing
Diet[edit | edit source]
"Dietary modification—altering the consistency of foods and liquids—is a fundamental aspect of dysphagia management."[18]
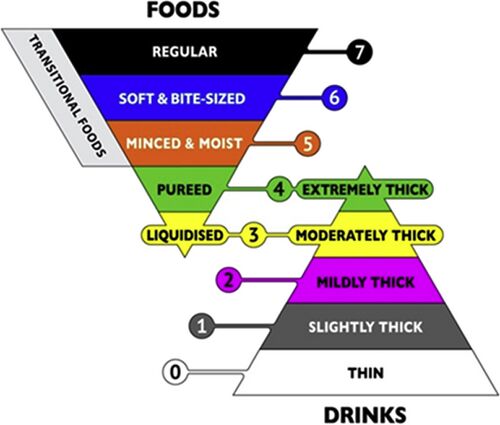
The International Dysphagia Diet Standardisation Initiative Functional Diet Scale (IDDSI) is a reliable scale for clinicians to "capture diet texture restriction and progression in people with dysphagia."[18] IDDSI describes and categorises foods and drinks according to their texture or flow characteristics. The degree of diet texture restriction must be recommended for a patient based on assessment by a qualified clinician. The IDDSI framework consists of 8 levels, represented by 2 intersecting pyramids. The 0 and 7 levels constitute of unmodified drinks and foods: levels 0-4 correspond to drinks and levels 3-7 measure foods. The middle levels represent progressively greater degrees of texture modification.
Refer to the IDDSI website for a detailed descriptions of food textures and drink thickness and their testing methods.
Dysphagia rehabilitation manual published a dysphagia diet pyramid, based on the work by Kanaya et al.[19][20] The 5-stage Seirei Dysphagia Diets consist of the following categories:
- L0 is gelatin jelly (tea or fruit juice, etc.)
- L1 is gelatin jelly (miso soup, milk, etc., containing protein)
- L2 is gelatin jelly (mixer meal with gelatin)
- L3 is a puréed or mixer meal
- L4 is a softened diet
The Dysphagia Diet Pyramid is known and used in Japan vs The International Dysphagia Diet Standardisation Initiative Functional Diet Scale (IDDSI) provides a common terminology to describe food textures and drink thickness.
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 Kagaya H, Inamoto Y, Okada S, Saitoh E. Body Positions and Functional Training to Reduce Aspiration in Patients with Dysphagia. JMAJ 2011; 54(1): 35–38.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 Banerjee S. Dysphagia Rehabilitation Management. Plus Course 2024
- ↑ Matsui T, Yamaya M, Ohrui T, Arai H, Sasaki H. Sitting position to prevent aspiration in bed-bound patients. Gerontology. 2002 May-Jun;48(3):194-5.
- ↑ Calvo I, Sunday KL, Macrae P, Humbert IA. Effects of chin-up posture on the sequence of swallowing events. Head & neck 2017: 39(5):947.
- ↑ 5.0 5.1 5.2 5.3 5.4 Lazarus CL, Husaini H, Falciglia D, DeLacure M, Branski RC, Kraus D, Lee N, Ho M, Ganz C, Smith B, Sanfilippo N. Effects of exercise on swallowing and tongue strength in patients with oral and oropharyngeal cancer treated with primary radiotherapy with or without chemotherapy. Int J Oral Maxillofac Surg. 2014 May;43(5):523-30.
- ↑ Sampallo-Pedroza RM, Cardona-López LF, Ramírez-Gómez KE. Description of oral-motor development from birth to six years of age. Rev. Fac. Med. 2014; 62 (4): 593-604.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 7.8 Krekeler BN, Rowe LM, Connor NP. Dose in Exercise-Based Dysphagia Therapies: A Scoping Review. Dysphagia 2021; 36(1): 1.
- ↑ Vose A, Nonnenmacher J, Singer ML, González-Fernández M. Dysphagia Management in Acute and Sub-acute Stroke. Curr Phys Med Rehabil Rep. 2014 Dec 1;2(4):197-206.
- ↑ Pohar S, Demarcantonio M, Whiting P, Crandley E, Wadsworth J, Karakla D. Percutaneous endoscopic gastrostomy tube dependence following chemoradiation in head and neck cancer patients. Laryngoscope. 2015 Jun;125(6):1366-71.
- ↑ Shieh WY, Wang CM, Cheng HK, Imbang TI. Noninvasive Measurement of Tongue Pressure and Its Correlation with Swallowing and Respiration. Sensors (Basel). 2021 Apr 7;21(8):2603.
- ↑ 11.0 11.1 Park JS, Hwang NK. Chin tuck against resistance exercise for dysphagia rehabilitation: A systematic review. J Oral Rehabil. 2021 Aug;48(8):968-977.
- ↑ Kraaijenga SA, van der Molen L, Stuiver MM, Teertstra HJ, Hilgers FJ, van den Brekel MW. Effects of Strengthening Exercises on Swallowing Musculature and Function in Senior Healthy Subjects: a Prospective Effectiveness and Feasibility Study. Dysphagia. 2015 Aug;30(4):392-403.
- ↑ 13.0 13.1 13.2 Niu C, Zhou W, Wang H, Zhang Y, Cai J, Lu N, Wang Y. The effect of voice training interventions on patients with oropharyngeal dysphagia: a systematic review. Eur Arch Otorhinolaryngol. 2023 Mar;280(3):973-984.
- ↑ Park A, Jang SJ, Kim NE, Kim TH, Sohn YH, Kim H, Cho SR. Swallowing outcomes following voice therapy in multiple system atrophy with dysphagia: comparison of treatment efficacy with Parkinson's disease. Dysphagia. 2022;37(1):198–206.
- ↑ Martin BJ, Logemann JA, Shaker R, Dodds WJ. Normal laryngeal valving patterns during three breath-hold maneuvers: A pilot investigation. 1993; 8(1):11–20.
- ↑ Han X, Ye Q, Meng Z, Pan D, Wei X, Wen H, Dou Z. Biomechanical mechanism of reduced aspiration by the Passy-Muir valve in tracheostomized patients following acquired brain injury: Evidences from subglottic pressure. Front Neurosci. 2022 Oct 31;16:1004013.
- ↑ 17.0 17.1 Sapienza C, Troche M, Pitts T, Davenport P. Respiratory strength training: concept and intervention outcomes. Semin Speech Lang. 2011 Feb;32(1):21-30.
- ↑ 18.0 18.1 Steele CM, Namasivayam-MacDonald AM, Guida BT, Cichero JA, Duivestein J, Hanson B, Lam P, Riquelme LF. Creation and initial validation of the international dysphagia diet standardisation initiative functional diet scale. Archives of physical medicine and rehabilitation. 2018 May 1;99(5):934-44.
- ↑ Fujishima, I. Rehabilitation for Swallowing Disorders Associated with Stroke; Ishiyaku Publishers, Inc.: Tokyo, Japan, 1993; pp. 81–86.
- ↑ Matsuo K, Fujishima I. Textural Changes by Mastication and Proper Food Texture for Patients with Oropharyngeal Dysphagia. Nutrients. 2020; 12(6):1613.
.






