Wrist Replacement: Difference between revisions
(anatomy) |
(post operative rehabilitation) |
||
| Line 24: | Line 24: | ||
* Wrist osteoarthritis | * Wrist osteoarthritis | ||
* Rheumatoid | * Rheumatoid arthritis | ||
* Post-traumatic arthritis | * Post-traumatic arthritis | ||
| Line 46: | Line 46: | ||
* Lack of active wrist extension | * Lack of active wrist extension | ||
== Complication of Wrist Arthroplasty == | |||
* Instability of the wrist | |||
* Infection at the wrist | |||
* Fracture of the wrist bone, | |||
* Dislocation of the wrist, | |||
* Damage to the nerves or blood vessels, | |||
* Deep vein thrombosis | |||
== Clinical Presentation == | == Clinical Presentation == | ||
Typical symptoms of arthritis at the wrist include: | |||
* Pain | |||
* Stiffness | |||
* Swelling | |||
* Reduced range of motion | |||
* Clicking, cracking or grinding sounds on movement | |||
== Diagnostic Tests == | == Diagnostic Tests == | ||
<br> | |||
== Pre-Op == | == Pre-Op == | ||
| Line 63: | Line 84: | ||
Radiographic assessment of bone quality, erosions, carpal collapse, carpal ulnar translations, volar subluxation and distal radioulnar joint. In PA view, the radial component should not should not extend beyond the edge of the styloid while the carpal component should not extend > 2mm over the margins of the carpus at osteotomy. | Radiographic assessment of bone quality, erosions, carpal collapse, carpal ulnar translations, volar subluxation and distal radioulnar joint. In PA view, the radial component should not should not extend beyond the edge of the styloid while the carpal component should not extend > 2mm over the margins of the carpus at osteotomy. | ||
Pre-op rehabilitation includes exercises to maintain strength and function of non-affected extremity and other joints of affected extremity and education on post-operative exercises. | |||
== Post-Op Rehabilitation == | |||
0-2 weeks | |||
* post-operative dressing | |||
* wrist is immobilized in neutral alignment | |||
* elevation of the limb to control swelling | |||
* mobilization of adjacent joints- shoulder and elbow joints | |||
3-5 weeks | |||
* removal of post-operative dressing | |||
* static splinting at 15<sup>0</sup> of flexion(worn during exercise and at night) | |||
* gentle passive and active range of motion exercises for the wrist and fingers | |||
* scar massage | |||
6-12 weeks | |||
* full PROM at the wrist minimizing radial and ulnar deviation of the wrist | |||
* dynamic splint | |||
* gentle progressive strengthening of the wrist and hand | |||
* gradual return to normal activities | |||
== Key Evidence == | == Key Evidence == | ||
| Line 73: | Line 119: | ||
== Resources <br> == | == Resources <br> == | ||
add appropriate resources here | add appropriate resources here | ||
== References == | == References == | ||
Revision as of 13:41, 25 October 2017
Description[edit | edit source]
Wrist replacement, also referred to as wrist arthroplasty is a surgical procedure in which the diseased or damaged joint is replaced with an artificial joint- an implant. It aims to create a stable, pain-free joint with a functional range of movement when conservative treatments have failed.
Total wrist arthroplasty (TWA) is a motion preserving alternative to arthrodesis of the wrist and usually lasts for about 10 to 15 years. Implant survival of 90-100% at five years are mostly reported using newer second generation and third generation implants, but declines from five to eight years.[1]
Total wrist replacements are non weight bearing joints; heavy household or occupational activity, use of a walking aid or repetitive movements e.g. hammering will increase the speed and incidence of loosening of the implants stems and the ultimate failure of the implant. The ideal patient for a TWA should have a low demand lifestyle, should not need the upper extremity for regular ambulation and transfers. Young active patients and individuals with high physical demands are not considered good candidates for TWA.[2][3]
Clinically Relevant Anatomy[edit | edit source]
The wrist/radiocarpal joint is a ellipsoid type of synovial joint. The wrist consists of two rows of carpal bones which forms the proximal segment of the hand and articulates proximally with the forearm via the wrist joint and distally with the five metacarpals. The ends of the bones are covered with articular cartilage. Cartilage is an elastic connective tissue whose purpose is to allow for a smooth, gliding motion between joints.[1] Movements occurring in the wrist include flexion, extension adduction and abduction. Diseases such as osteoarthritis and rheumatoid arthritis, injury and infection can damage or wear out the articular cartilage. This may cause the wrist bones to rub against each other producing pain, stiffness and swelling of the wrist.
The Artificial Wrist[edit | edit source]
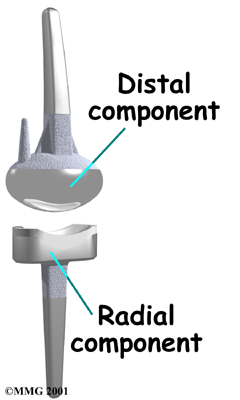
Earlier designs of wrist implants had high complications and failure rates, however, advances in prosthetic design have contributed to improved clinical outcomes and greater implant longevity.[4] The implant is made from metal and plastic and has 2 components- radial and distal component.
The radial component: is the part that fits against the end of the radius bone. It is made up of two pieces- a flat metal piece with a stem that attaches down into the canal of the bone and a plastic cup that fits onto the metal piece, forming a socket for the artificial wrist joint.
The distal component: is the part that replaces the small wrist bones. This piece is made completely of metal. It is globe shaped to fit into the plastic socket on the end of the radius. It is attached by two metal stems that fit into the hollow bone marrow cavities of the carpal and metacarpal bones of the hand.
The prosthesis typically is stable and should demonstrate approximately 350 of flexion and 350 of extension with modest tightness at full extensions.
Indications[edit | edit source]
- Wrist osteoarthritis
- Rheumatoid arthritis
- Post-traumatic arthritis
- Failed wrist fusion
- Advanced avascular necrosis of the carpal bones
- Kienbock disease
Contra-indications[edit | edit source]
- Severe ligamentous laxity in form of severe volar subluxation
- Highly active synovitis in patients with RA
- Systemic lupus erythematosus
- Patients with minimally functional hand
- Recent infection
- Lack of active wrist extension
Complication of Wrist Arthroplasty[edit | edit source]
- Instability of the wrist
- Infection at the wrist
- Fracture of the wrist bone,
- Dislocation of the wrist,
- Damage to the nerves or blood vessels,
- Deep vein thrombosis
Clinical Presentation[edit | edit source]
Typical symptoms of arthritis at the wrist include:
- Pain
- Stiffness
- Swelling
- Reduced range of motion
- Clicking, cracking or grinding sounds on movement
Diagnostic Tests[edit | edit source]
Pre-Op[edit | edit source]
In patients with rheumatoid arthritis, a comprehensive pre-operative evaluation should be carried out. Prior to wrist arthroplasty, a hip or knee replacement surgery should be carried out to prevent weight bearing on the wrist prosthesis, improve hand balance and optimize rehabilitation of the digits.
Patients for wrist arthroplasty should temporarily discontinue medications such as methotrexate (anti rheumatic) and immune-modulating drugs after consulting with their rheumatologist to reduce the risk of infections and delayed wound healing. NSAIDs should also be reduced at least 10 days pre-operatively and 5 days post-operatively to reduce the risk of bleeding complications.
Radiographic assessment of bone quality, erosions, carpal collapse, carpal ulnar translations, volar subluxation and distal radioulnar joint. In PA view, the radial component should not should not extend beyond the edge of the styloid while the carpal component should not extend > 2mm over the margins of the carpus at osteotomy.
Pre-op rehabilitation includes exercises to maintain strength and function of non-affected extremity and other joints of affected extremity and education on post-operative exercises.
Post-Op Rehabilitation[edit | edit source]
0-2 weeks
- post-operative dressing
- wrist is immobilized in neutral alignment
- elevation of the limb to control swelling
- mobilization of adjacent joints- shoulder and elbow joints
3-5 weeks
- removal of post-operative dressing
- static splinting at 150 of flexion(worn during exercise and at night)
- gentle passive and active range of motion exercises for the wrist and fingers
- scar massage
6-12 weeks
- full PROM at the wrist minimizing radial and ulnar deviation of the wrist
- dynamic splint
- gentle progressive strengthening of the wrist and hand
- gradual return to normal activities
Key Evidence[edit | edit source]
add text here relating to key evidence with regards to any of the above headings
Resources
[edit | edit source]
add appropriate resources here
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ Boeckstyns ME Dan Med J 2014 May;61(5):A4834.
- ↑ Adams BD. Total wrist arthroplasty. Journal of the American Society for Surgery of the Hand. 2001;1:236-248
- ↑ Adams BD, Khoury JG. Total wrist arthroplasty. In : Weiss APC, Hastings H, eds. Surgery of the Arthritic Hand Wrist. Philadephia, Pa: Lippincott Williams& Wikins; 2002:166-176
- ↑ Kennedy CD, Huang JI Orthop Clin North Am. 2016