Whiplash Associated Disorders: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editor '''- Your name will be added here if you created the original content for this page. | |||
Original Editor - Your name will be added here if you created the original content for this page. | |||
Lead Editors - Your name will be added here if you are a lead editor on this page. [[Physiopedia:Editors|Read more.]] | '''Lead Editors''' - Your name will be added here if you are a lead editor on this page. [[Physiopedia:Editors|Read more.]] | ||
</div> | |||
== Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | |||
<div class="researchbox"> | |||
<rss>Feed goes here!!|charset=UTF-8|short|max=10</rss> | |||
</div> | |||
== References == | |||
| | References will automatically be added here, see [[Adding References|adding references tutorial]]. | ||
< | <references /> | ||
== Clinically Relevant Anatomy<br> == | == Clinically Relevant Anatomy<br> == | ||
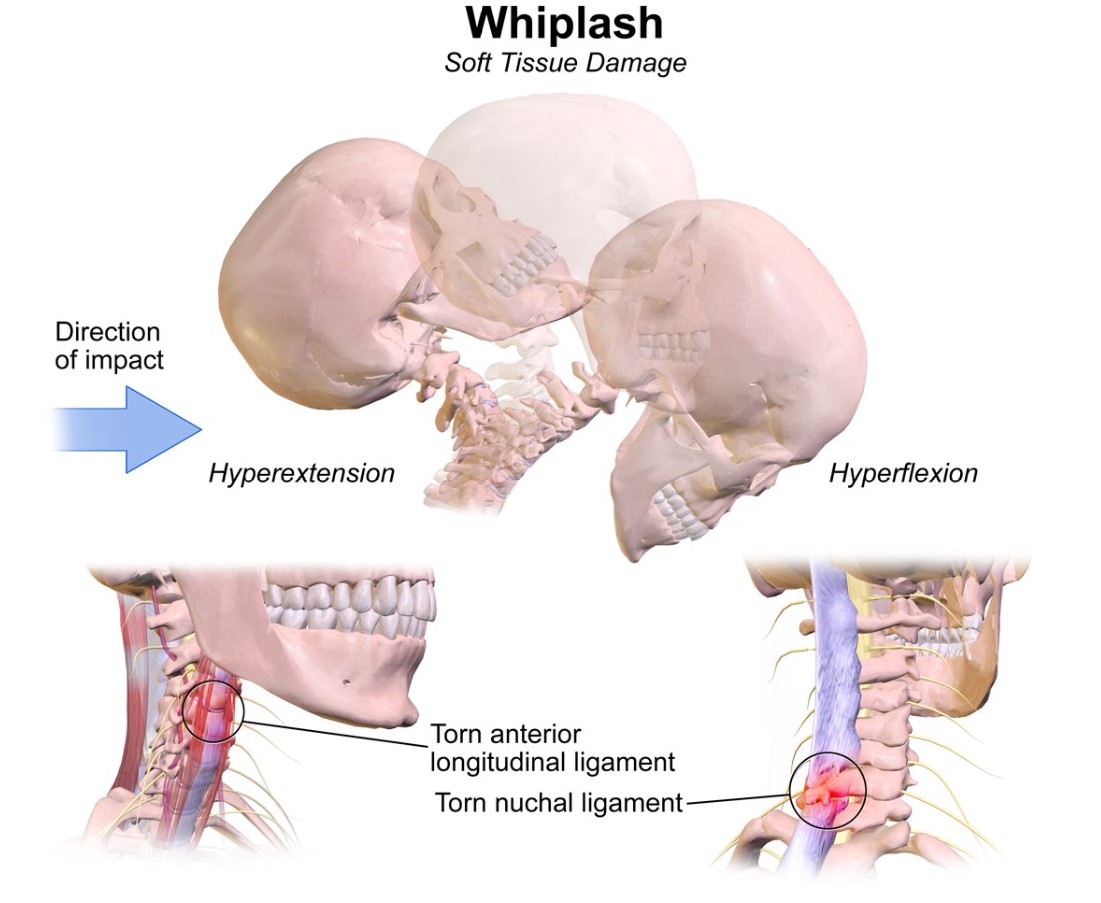
Whiplash and whiplash associated disorders (WAD) affects variable areas of the cervical spine, depending on the force and direction of impact as well as many other factors. In a whiplash injury, bony structures, ligamentous structures, muscles, neurological structures, and other connective tissue may be affected. Anatomic causes of pain can be any of these structures, with the strain injury resulting in secondary edema, hemorrhage, and inflammation. | Whiplash and whiplash associated disorders (WAD) affects variable areas of the cervical spine, depending on the force and direction of impact as well as many other factors. In a whiplash injury, bony structures, ligamentous structures, muscles, neurological structures, and other connective tissue may be affected. Anatomic causes of pain can be any of these structures, with the strain injury resulting in secondary edema, hemorrhage, and inflammation. | ||
== Mechanism of Injury / Pathological Process<br> == | == Mechanism of Injury / Pathological Process<br> == | ||
The mechanism of injury is variable, usually involving a motor vehicle accident but also including causes such as sports injury, child abuse, blows to the head from a falling object, or similar accelleration-decceleration event. | The mechanism of injury is variable, usually involving a motor vehicle accident but also including causes such as sports injury, child abuse, blows to the head from a falling object, or similar accelleration-decceleration event. | ||
[[Image: | [[Image:Whiplash Injuries.jpg|border|center]] | ||
== Clinical Presentation == | == Clinical Presentation == | ||
The most common presentation will be sub-occipital headaches and/or neck pain that is constant or motion-induced. There may be up to 48 hrs delay of symptom onset from the initial injury. Other signs include neurologic signs, dizziness, tinnitus, visual disturbances, UE radicular pain, difficulty sleeping due to pain, and difficulty concentrating/poor memory. ([http://emedicine.medscape.com/article/306176-overview eMedicine]) It is important to provide a thorough spinal exam and neurologic exam in patient with WAD to screen for delayed-onset of cervical spine instability or myelopathy. <ref name="Delfini et al">Delfini R, Dorizzi A, Facchinetti G, Faccioli F, Galzio R, Vangelista T. Delayed post-traumatic cervical instability. Surg Neurol. 1999;51:588-95.</ref><br> | The most common presentation will be sub-occipital headaches and/or neck pain that is constant or motion-induced. There may be up to 48 hrs delay of symptom onset from the initial injury. Other signs include neurologic signs, dizziness, tinnitus, visual disturbances, UE radicular pain, difficulty sleeping due to pain, and difficulty concentrating/poor memory. ([http://emedicine.medscape.com/article/306176-overview eMedicine]) It is important to provide a thorough spinal exam and neurologic exam in patient with WAD to screen for delayed-onset of cervical spine instability or myelopathy. <ref name="Delfini et al">Delfini R, Dorizzi A, Facchinetti G, Faccioli F, Galzio R, Vangelista T. Delayed post-traumatic cervical instability. Surg Neurol. 1999;51:588-95.</ref><br> | ||
===== QTFC (Quebec Task Force Classification)<br> ===== | ===== QTFC (Quebec Task Force Classification)<br> ===== | ||
The Quebec Task Force was a task force sponsored by a public insurer in Canada. They submitted recommendations regarding classification and treatment of WAD, which was used to develop a guide for managing whiplash in 1995. An updated report was published in 2001. Each of the grades corresponds to a specific treatment recommendation.<br> | The Quebec Task Force was a task force sponsored by a public insurer in Canada. They submitted recommendations regarding classification and treatment of WAD, which was used to develop a guide for managing whiplash in 1995. An updated report was published in 2001. Each of the grades corresponds to a specific treatment recommendation.<br> | ||
{| cellspacing="1" cellpadding="1" | {| width="404" cellspacing="1" cellpadding="1" border="2" align="center" | ||
|- | |- | ||
| '''QTFC Grade'''<br> | | '''QTFC Grade'''<br> | ||
| '''Clinical presentation'''<br> | | '''Clinical presentation'''<br> | ||
|- | |- | ||
| 0'''<br>''' | | 0'''<br>''' | ||
| | | | ||
No complaint about neck pain | No complaint about neck pain | ||
No physical signs<br> | No physical signs<br> | ||
|- | |- | ||
| I<br> | | I<br> | ||
| | | | ||
Nec complaints of pain, stiffness or tenderness only | Nec complaints of pain, stiffness or tenderness only | ||
No physical signs<br> | No physical signs<br> | ||
|- | |- | ||
| II<br> | | II<br> | ||
| | | | ||
Neck complaint | Neck complaint | ||
Musculoskeletal signs including<br> | Musculoskeletal signs including<br> | ||
*decreased ROM<br> | *decreased ROM<br> | ||
*point tenderness<br> | *point tenderness<br> | ||
|- | |- | ||
| <span style="font-weight: bold">III</span><br> | | <span style="font-weight: bold;">III</span><br> | ||
| | | | ||
Neck complaint | Neck complaint | ||
| Line 70: | Line 74: | ||
|- | |- | ||
| IV<br> | | IV<br> | ||
| Neck complaint and fracture or dislocation<br> | | Neck complaint and fracture or dislocation<br> | ||
|} | |} | ||
<br> | <br> | ||
<br> | <br> | ||
'''MQTFC (Modified Quebec Task Force Classification) '''<ref name="PMID: 15040964 [PubMed - indexed for MEDLINE]">Sterling M., Man Ther. 2004 May;9(2):60-70. A proposed new classification system for whiplash associated disorders--implications for assessment and management.</ref><br> | '''MQTFC (Modified Quebec Task Force Classification) '''<ref name="PMID: 15040964 [PubMed - indexed for MEDLINE]">Sterling M., Man Ther. 2004 May;9(2):60-70. A proposed new classification system for whiplash associated disorders--implications for assessment and management.</ref><br> | ||
<br> | <br> | ||
<br> | <br> | ||
{| | {| cellspacing="1" cellpadding="1" border="1" align="center" style="width: 596px; height: 1318px;" | ||
|- | |- | ||
| | | | ||
Proposed<br> | Proposed<br> | ||
classification grade | classification grade | ||
| Physical and psychological impairments present<br> | | Physical and psychological impairments present<br> | ||
|- | |- | ||
| WAD 0<br> | | WAD 0<br> | ||
| | | | ||
No complaints about neck pain | No complaints about neck pain | ||
No physical signs<br> | No physical signs<br> | ||
|- | |- | ||
| WAD I<br> | | WAD I<br> | ||
| | | | ||
'''No complaints of pain, stiffness or tenderness only''' | '''No complaints of pain, stiffness or tenderness only''' | ||
No physical signs<br> | No physical signs<br> | ||
|- | |- | ||
| WAD IIA<br> | | WAD IIA<br> | ||
| | | | ||
Neck complaint | Neck complaint | ||
'''Motor impairment'''<br> | '''Motor impairment'''<br> | ||
*decreased ROM<br> | *decreased ROM<br> | ||
*altered muscle recruitment patterns (CCFT)<br> | *altered muscle recruitment patterns (CCFT)<br> | ||
| Line 121: | Line 125: | ||
|- | |- | ||
| WAD IIB<br> | | WAD IIB<br> | ||
| | | | ||
Neck complaint | Neck complaint | ||
| Line 130: | Line 134: | ||
*altered muscle recruitment patterns (CCFT) | *altered muscle recruitment patterns (CCFT) | ||
Sensory Impairment<br> | Sensory Impairment<br> | ||
*local cervical mechanical hyperalgesia<br> | *local cervical mechanical hyperalgesia<br> | ||
| Line 139: | Line 143: | ||
|- | |- | ||
| WAD IIC<br> | | WAD IIC<br> | ||
| Neck complaint | | Neck complaint | ||
Motor impairment | Motor impairment | ||
| Line 150: | Line 154: | ||
*local cervical mechanical hyperalgesia | *local cervical mechanical hyperalgesia | ||
*'''generalized sensory hypersensitivity (mechanical, thermal, ULNT)<br>''' | *'''generalized sensory hypersensitivity (mechanical, thermal, ULNT)<br>''' | ||
*'''Some may show SNS disturbances'''<br> | *'''Some may show SNS disturbances'''<br> | ||
Psychological impairment | Psychological impairment | ||
*elevated psychological distress (GHQ, TAMPA)<br> | *elevated psychological distress (GHQ, TAMPA)<br> | ||
*'''elevated levels of acute posttraumatic stress (IES)'''<br> | *'''elevated levels of acute posttraumatic stress (IES)'''<br> | ||
|- | |- | ||
| WAD III<br> | | WAD III<br> | ||
| | | | ||
Neck complaint | Neck complaint | ||
| Line 175: | Line 179: | ||
*Some may show SNS disturbances | *Some may show SNS disturbances | ||
'''Neurological signs of conduction loss including:'''<br> | '''Neurological signs of conduction loss including:'''<br> | ||
*decrease or absent deep tendon reflexes<br> | *decrease or absent deep tendon reflexes<br> | ||
*muscle weakness<br> | *muscle weakness<br> | ||
*sensory deficits<br> | *sensory deficits<br> | ||
| Line 187: | Line 191: | ||
|- | |- | ||
| WAD IV<br> | | WAD IV<br> | ||
| '''Fracture or dislocation'''<br> | | '''Fracture or dislocation'''<br> | ||
|} | |} | ||
<br> | <br> | ||
<br> | <br> | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
Canadian C-Spine Rule (CCR): algorithm to determine the necessity for cervical spine radiography in alert and stable patients presenting with trauma and cervical spine injury. <ref name="Stiell et al">Stiell IG, Clement CM, McKnight RD, Brison R, Schull MJ, Rowe BH, Worthington JR, Eisenhauer MA, Cass D, Greenberg G, MacPhail I, Dreyer J, Lee JS, Bandiera G, Reardon M, Holoroyd B, Lesiuk H, Wells GA. The Canadian c-spine rule versus the NEXUS low-risk criteria in patients with trauma. N Engl J Med. 2003;349(26): 2510-2518.</ref> | Canadian C-Spine Rule (CCR): algorithm to determine the necessity for cervical spine radiography in alert and stable patients presenting with trauma and cervical spine injury. <ref name="Stiell et al">Stiell IG, Clement CM, McKnight RD, Brison R, Schull MJ, Rowe BH, Worthington JR, Eisenhauer MA, Cass D, Greenberg G, MacPhail I, Dreyer J, Lee JS, Bandiera G, Reardon M, Holoroyd B, Lesiuk H, Wells GA. The Canadian c-spine rule versus the NEXUS low-risk criteria in patients with trauma. N Engl J Med. 2003;349(26): 2510-2518.</ref> | ||
[[Image:CCR.jpg|border|center|Canadian C-Spine Rule]]<br><br> | [[Image:CCR.jpg|border|center|Canadian C-Spine Rule]]<br><br> | ||
== Management / Interventions<br> == | == Management / Interventions<br> == | ||
Management approaches for patients with WAD are poorly researched. These patients often do not fit into treatment categories as defined for other cervical pain problems due to multiple factors, and even within the WAD group there are multiple variances which warrant individualized treatment approaches. The most recent evidence supports the use of [http://academic.regis.edu/clinicaleducation/pdf%27s/M_Sterling_Long_term_whiplash.pdf Sterling's] classification system for WAD. <ref name="Sterling et al">Sterling M, Jull G, Kenardy J. Physical and psychological factors maintain long-term predictive capacity post-whiplash injury. Pain. 2006;122:102-108.</ref> | Management approaches for patients with WAD are poorly researched. These patients often do not fit into treatment categories as defined for other cervical pain problems due to multiple factors, and even within the WAD group there are multiple variances which warrant individualized treatment approaches. The most recent evidence supports the use of [http://academic.regis.edu/clinicaleducation/pdf%27s/M_Sterling_Long_term_whiplash.pdf Sterling's] classification system for WAD. <ref name="Sterling et al">Sterling M, Jull G, Kenardy J. Physical and psychological factors maintain long-term predictive capacity post-whiplash injury. Pain. 2006;122:102-108.</ref> | ||
== Differential Diagnosis<br> == | == Differential Diagnosis<br> == | ||
Cervical radiculopathy<br>Facticious disorder<br>Polymyalgia Rheumatica<br>Traumatic Brain Injury<br>Cervical herniated disk<br>Cervical myelopathy<br>Cervical osteoarthritis<br>Infection or osteomyelitis<br>Inflammatory rheumatologic disease<br>Malingering<br>Psychogenic pain disorder<br>Referred pain from cardiothoracic structures<br>Tumor or malignancy of cervical spine | Cervical radiculopathy<br>Facticious disorder<br>Polymyalgia Rheumatica<br>Traumatic Brain Injury<br>Cervical herniated disk<br>Cervical myelopathy<br>Cervical osteoarthritis<br>Infection or osteomyelitis<br>Inflammatory rheumatologic disease<br>Malingering<br>Psychogenic pain disorder<br>Referred pain from cardiothoracic structures<br>Tumor or malignancy of cervical spine | ||
Vascular abnormality of cervical structures | Vascular abnormality of cervical structures | ||
== Key Evidence == | == Key Evidence == | ||
[http://whiplashinfo.se/artiklar_debatt_forskning_asikter/redefining_whiplash.pdf "Whiplash associated disorders- redefining whiplash and its management" by the Quebec Task Force: a critical evaluation.] | [http://whiplashinfo.se/artiklar_debatt_forskning_asikter/redefining_whiplash.pdf "Whiplash associated disorders- redefining whiplash and its management" by the Quebec Task Force: a critical evaluation.] | ||
== Resources <br> == | == Resources <br> == | ||
www.som.uq.edu.au/whiplash | www.som.uq.edu.au/whiplash | ||
[http://www.slsportstherapy.com/content/documents/PIER/SLST/Whiplash-PIER-SLST.pdf Evidence-based summary] | [http://www.slsportstherapy.com/content/documents/PIER/SLST/Whiplash-PIER-SLST.pdf Evidence-based summary] | ||
== Case Studies == | == Case Studies == | ||
add links to case studies here (case studies should be added on new pages using the [[Template:Case Study|case study template]])<br> | add links to case studies here (case studies should be added on new pages using the [[Template:Case Study|case study template]])<br> | ||
== References == | == References == | ||
References will automatically be added here, see [[Adding References|adding references tutorial]]. <references /> | References will automatically be added here, see [[Adding References|adding references tutorial]]. <references /> | ||
Revision as of 14:45, 5 December 2009
Original Editor - Your name will be added here if you created the original content for this page.
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
Clinically Relevant Anatomy
[edit | edit source]
Whiplash and whiplash associated disorders (WAD) affects variable areas of the cervical spine, depending on the force and direction of impact as well as many other factors. In a whiplash injury, bony structures, ligamentous structures, muscles, neurological structures, and other connective tissue may be affected. Anatomic causes of pain can be any of these structures, with the strain injury resulting in secondary edema, hemorrhage, and inflammation.
Mechanism of Injury / Pathological Process
[edit | edit source]
The mechanism of injury is variable, usually involving a motor vehicle accident but also including causes such as sports injury, child abuse, blows to the head from a falling object, or similar accelleration-decceleration event.
Clinical Presentation[edit | edit source]
The most common presentation will be sub-occipital headaches and/or neck pain that is constant or motion-induced. There may be up to 48 hrs delay of symptom onset from the initial injury. Other signs include neurologic signs, dizziness, tinnitus, visual disturbances, UE radicular pain, difficulty sleeping due to pain, and difficulty concentrating/poor memory. (eMedicine) It is important to provide a thorough spinal exam and neurologic exam in patient with WAD to screen for delayed-onset of cervical spine instability or myelopathy. [1]
QTFC (Quebec Task Force Classification)
[edit | edit source]
The Quebec Task Force was a task force sponsored by a public insurer in Canada. They submitted recommendations regarding classification and treatment of WAD, which was used to develop a guide for managing whiplash in 1995. An updated report was published in 2001. Each of the grades corresponds to a specific treatment recommendation.
| QTFC Grade |
Clinical presentation |
| 0 |
No complaint about neck pain No physical signs |
| I |
Nec complaints of pain, stiffness or tenderness only No physical signs |
| II |
Neck complaint Musculoskeletal signs including
|
| III |
Neck complaint Musculosceletal signs Neurological signs including:
|
| IV |
Neck complaint and fracture or dislocation |
MQTFC (Modified Quebec Task Force Classification) [2]
|
Proposed classification grade |
Physical and psychological impairments present |
| WAD 0 |
No complaints about neck pain No physical signs |
| WAD I |
No complaints of pain, stiffness or tenderness only No physical signs |
| WAD IIA |
Neck complaint Motor impairment
Sensory Impairment
|
| WAD IIB |
Neck complaint Motor impairment
Sensory Impairment
Psychological impairment
|
| WAD IIC |
Neck complaint
Motor impairment
Sensory Impairment
Psychological impairment
|
| WAD III |
Neck complaint Motor impairment
Sensory Impairment
Neurological signs of conduction loss including:
Psychological impairment
|
| WAD IV |
Fracture or dislocation |
Diagnostic Procedures[edit | edit source]
Canadian C-Spine Rule (CCR): algorithm to determine the necessity for cervical spine radiography in alert and stable patients presenting with trauma and cervical spine injury. [3]
Management / Interventions
[edit | edit source]
Management approaches for patients with WAD are poorly researched. These patients often do not fit into treatment categories as defined for other cervical pain problems due to multiple factors, and even within the WAD group there are multiple variances which warrant individualized treatment approaches. The most recent evidence supports the use of Sterling's classification system for WAD. [4]
Differential Diagnosis
[edit | edit source]
Cervical radiculopathy
Facticious disorder
Polymyalgia Rheumatica
Traumatic Brain Injury
Cervical herniated disk
Cervical myelopathy
Cervical osteoarthritis
Infection or osteomyelitis
Inflammatory rheumatologic disease
Malingering
Psychogenic pain disorder
Referred pain from cardiothoracic structures
Tumor or malignancy of cervical spine
Vascular abnormality of cervical structures
Key Evidence[edit | edit source]
Resources
[edit | edit source]
www.som.uq.edu.au/whiplash
Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ Delfini R, Dorizzi A, Facchinetti G, Faccioli F, Galzio R, Vangelista T. Delayed post-traumatic cervical instability. Surg Neurol. 1999;51:588-95.
- ↑ Sterling M., Man Ther. 2004 May;9(2):60-70. A proposed new classification system for whiplash associated disorders--implications for assessment and management.
- ↑ Stiell IG, Clement CM, McKnight RD, Brison R, Schull MJ, Rowe BH, Worthington JR, Eisenhauer MA, Cass D, Greenberg G, MacPhail I, Dreyer J, Lee JS, Bandiera G, Reardon M, Holoroyd B, Lesiuk H, Wells GA. The Canadian c-spine rule versus the NEXUS low-risk criteria in patients with trauma. N Engl J Med. 2003;349(26): 2510-2518.
- ↑ Sterling M, Jull G, Kenardy J. Physical and psychological factors maintain long-term predictive capacity post-whiplash injury. Pain. 2006;122:102-108.