Health and wellbeing needs of the homeless, the physiotherapist's role: Difference between revisions
Sarah Rhind (talk | contribs) No edit summary |
Sarah Rhind (talk | contribs) No edit summary |
||
| Line 171: | Line 171: | ||
==== Stages of Change Model ==== | ==== Stages of Change Model ==== | ||
<br>Prochaska and DiClemente's stages of change model (1982) explains one’s readiness for behavioural change. This model consists of five stages: precontemplation, contemplation, planning, action and maintenance. Those who are in precontemplation stage have no intention to change their behaviour (Connors et al. 2012). It could be due to a lack of awareness, unwillingness as well as previous failed attempts. The people in contemplation stage are considering a change in behaviour. They could be thinking about the pros and cons of changing their behaviour. People in the contemplation stage are more likely to seek for assistance and enquire further information on possible solutions.<br>Study done by Velasquez et al. (2000) shows that majority of the homeless population with alcohol and drug abuse are in precontemplation and contemplation stage. Only 4% of alcohol abusers are in the action stage and are actively trying to quit drinking. (CBT Part)<br> | |||
?? picture of cycle | |||
INTERACTIVE ELEMENT HERE<br> | |||
== '''<font size="5">Accesibility of Health Care</font>''' == | == '''<font size="5">Accesibility of Health Care</font>''' == | ||
Revision as of 15:30, 11 January 2016
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - <img class="FCK__MWTemplate" src="http://www.physio-pedia.com/extensions/FCKeditor/fckeditor/editor/images/spacer.gif" _fckfakelement="true" _fckrealelement="2" _fck_mw_template="true">
Introduction[edit | edit source]
Throughout this Physiopedia resource we will be discussing and exploring the health and wellbeing problems associated with the homeless population in order to give you a better understanding of what they are dealing with. We will also give an introduction into the management of these issues and the impact they can have on physiotherapy. The resource should take approximately 10 hours to complete on a self-study basis. The resource is aimed at final year physiotherapy students and recently qualified physiotherapists. We will discuss five main topics which are physical health, mental health, substance abuse, accessibility of health care and the implications to physiotherapy.
Aims and Learning Outcomes[edit | edit source]
Aims:
To provide a resource for final year physiotherapy students and newly qualified physiotherapists regarding the health and wellbeing problems faced by the homeless population in the United Kingdom and consideration of the physiotherapists role in management of this population.
Learning outcomes:
By the end of this resource you will be able to:
1. Debate the issue surrounding homelessness within the United Kingdom.
2. Critically discuss the main/key health problems experienced by the homeless population in the UK.
3. Evaluate some of the challenges that the homeless population face when accessing physiotherapy.
4. Critically reflect on the physiotherapist’s role in assessing and managing the health and well-being needs of the homeless population.
Learning Styles[edit | edit source]
This resource will aim to suit everyone’s learning styles. A learning style is the way in which we learn best. Figure 1 below shows the different ways in which one learns or you can find out by taking the VARK test which is a free online resource (external link). By engaging every reader (undertaking the resource) in different activities that suits their learning style they will get more out of the resource.
Insert picture of learning styles
Homelessness in the UK [edit | edit source]
By the end of this section you should be able to debate the issues surrounding homelessness in the United Kingdom, meeting learning outcome 1. This section should take 30/40 minutes to complete.
It is widely thought that homelessness is just about those ‘sleeping rough’ and on the streets, however that is just a minority of the problem. A person can be classified as homeless if they do not have a permanent home (Crisis 2005). This can be anyone who is staying with a friend, in a B&B, a hostel or a temporary home (Shelter 2014). It is believed that the homeless population are some of the most vulnerable people in our society including those of ill health, low income, unemployment, isolation and relationship breakdown (Crisis 2005).
The 2014-2015 audit results estimated there was 28,615 homeless people in Scotland, a number which has significantly decreased since 2009-2010 when 43,371 were estimated to be homeless. Figure 2 demonstrates the time-line of homeless in Scotland over the past 23 years (Shelter Scotland 2015a). Single men make up a large proportion of the homeless population at 45% compared to single females at 21% (Shelter Scotland 2015b).
[insert graph]
Figure 2: Applications and Assessment made by the homeless population
There are several different reasons why a person can become homeless. In 2014-2015 over half of homelessness applications made were due to relationship breakdown or being asked to leave their permanent address (Shelter Scotland 2015c). Below, figure 3 expresses the reasons behind homelessness in Scotland.
[insert graph]
Figure 3: Reasons for homelessness
Crisis (2014) found that most often males who were homeless, became homeless due to relationship breakdown, substance abuse or leaving an institute for example; hospital, prison or care. More specifically they found that 18% were ex-prisoners, 8% were care leavers and 3% were ex-armed forces. Additionally, 32% of ‘rough sleepers’ in London were previously in prison.
The homeless health audit results from 2014 (Homeless link 2010) highlights the health and well-being problems faced by the homeless population. It was found that 73% of homeless people report some form of physical problem, 80% suffer from a mental health problem, 39% explained they have suffered from a drug problem and 27% from an alcohol problem. In addition, 35% had been admitted to A&E in the past, with 26% having been admitted in the last 6 months.
Below, figure 4 highlights just a few of the homeless populations problems they can be faced on a day to day basis (Health EducationAuthority 1999).
Figure 4: Factors perpetuating the homeless lifestyle
The Crisis (2011a) report ended with the chilling quote “ultimately homelessness kills” putting an emphasis on the NHS services to deliver the best patient centred, compassionate care to this very vulnerable population. Additionally, Crisis (2011b) believes new laws need to be enforced to give the homeless population emergency accommodation, written advice and real assistance for their medical needs.
In 2013 it was estimated that 70% of homeless people being discharged from hospital did not have their health or housing needs met. After that it was released that £10million funding was given to the NHS and voluntary run homeless centres to help tackle health and housing needs after discharge from hospital (Department of Health 2013a). Annually the government provides £470 million in trying to prevent homelessness, aiming to ensure the safety of those who are vulnerable (Department of Health 2013b). It is believed that a homeless person is 6 times more likely to visit A&E than someone with a permanent address and the cost of treating them is 8 times higher than due to their complex physical, social and psychological needs which costs the NHS £85 million every year.
<img class="FCK__MWTemplate" src="http://www.physio-pedia.com/extensions/FCKeditor/fckeditor/editor/images/spacer.gif" _fckfakelement="true" _fckrealelement="0" _fck_mw_template="true">
Maslow's Hierarcy of Needs[edit | edit source]
Maslow’s hierarchy of needs explains that people are motivated to achieve certain goals. In this hierarchy, there are five stages. The lower level basic needs have to be achieved before it is progressed to the next level. It was explained that self-actualisation is desired in every person. However, due to various life situations, progression from the lower level needs are often hindered.
Majority of the homeless people are still seeking to achieve their physiological needs, such as food, water, shelter, warmth and sleep. When such needs are not met, they tend to overlook health issues, thus prioritising other issues such as employment and the search for food above seeking medical attention. As such, contributing to the lack of usage of medical services in this population.
[insert picture]
Physical Health [edit | edit source]
By the end of this physical health section of the resource you should be able to discuss the physical health problems experienced by the homeless population which will contribute to completing learning outcome 2. This section should take 1hr/1hr30 to complete.
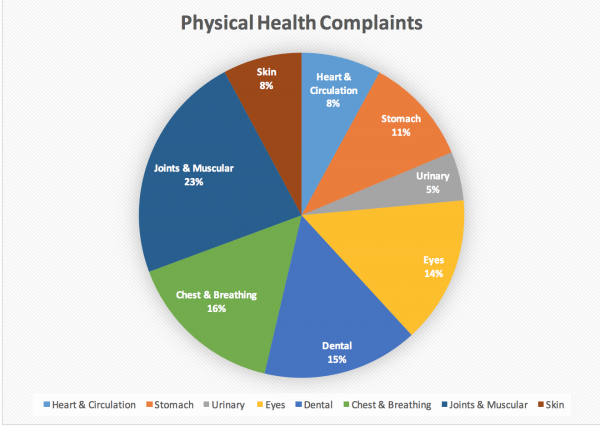
The Health Audit Findings (2014) found that long standing physical health problems were more common in the homeless population compared to the general population. There could be many reasons for this including accessibility of health care, Maslow's hierarchy of needs, fear of judgment when attending appointments and not regarding their health as important. It is perceived by the general public that to register with a GP, a permanent address is required however this is not true. The rights of a homeless person states they can register with a GP, despite living in temporary accommodation/sleeping rough (Shelter 2015). In fact the health audit findings, highlighted that 90% of homeless people in the UK are registered to a GP. Figure 1 demonstrates the physical problems faced by the homeless population on a daily basis. The graph only displays the long term health issues faced (longer than 12 months) and if the survey included short-term health problems, these percentages would be far greater. Fisher et al (2013) explained that due to the homeless population suffering a higher number of health related problems compared to the general population, their functional ability and quality of life are reduced. Ultimately this affects their life expectancy which, for a female is 43 and a male 47, 30 years younger than the national average.
Figure 5: Physical health complaints of the homeless (Health Audit Results 2014)
Musculoskeletal Problems[edit | edit source]
Within the homeless population, acute musculoskeletal pain is often brought on by trauma such as fighting, falling or being hit by vehicles (Hwang 2001). Complications of these injuries can be exacerbated by unsanitary living conditions and can lead to chronic pain, infections and abscesses. Musculoskeletal pain such as low back pain are very common, particularly among those sleeping rough. The British School of Osteopathy (BSO) (2014) run a weekly centre that sees between 130 and 220 patients a day. They estimate that 38% of the homeless population have MSK injuries. The majority being treated for acute and chronic neck and back problems. Referrals can be made for the acute injuries to eliminate fractures and muscle/ligament tears. The BSO allocate/have time to discuss social and economic problems with patients and can refer them on for help. Fisher et al (2013) undertook an observational study looking into chronic pain levels in the homeless, using questionnaires in homeless shelters in Cambridge. Most common pains were that 51.4% reported pain in the lower limbs, 36.9% in the abdomen, back and pelvis. Neuropathic pain was found in 16.9% of the population surveyed (compared with 8% of the general population). Pain is a substantial problem in homeless shelter users: 71.3% reported acute pain, and 59.3% fulfilled the criteria for chronic pain, the mean duration of which exceeded 6 years. Fisher et al (2013) concluded that due to poor sleeping levels, decreased physical activity levels and poor analgesia control, chronic pain is substantially higher among this population compared to the general public. However it was difficult to distinguish whether being homeless was the cause of the chronic pain, or whether it started before the participants became homeless. Due to such a high proportion of the homeless population suffering from some form of chronic pain it is important that physiotherapists understand the chronic pain mechanism and how to manage chronic pain effectively. Referring to chronic pain specialists may be beneficial for medication reviews.
Neuological Issues[edit | edit source]
Oddy et al (2012) found that within the homeless population in the UK, almost half (47%) of homeless participants reported having a traumatic brain injury (TBI) compared to just 21% of the general population. This can leave them in a very vulnerable place and subsequently suffer impairments including memory loss, attention, impulse control and behavioural difficulties (Brainline 2015).
Neuropathic pain associated with diabetes, HIV, hepatitis, liver cirrhosis. St Mungo's (2014) estimate that approximately 3,200 homeless people are living with diabetes in the UK, however they estimate that many more are living with it however are not receiving the correct health care or advice. Alcohol is well known to have adverse reactions with diabetes medication and can often cause worsening of nerve damage and cause medications to become less effective.
Respiratory Needs[edit | edit source]
Homeless Link estimated that 7% of the homeless population suffer from respiratory conditions. 15% complained of chest pain or breathing problems for over 12 months compared to 21% for less than 12 months. Smoking is very common within the homeless population and is one of the largest contributors to developing respiratory disorders in particular chronic obstructive pulmonary disorders (COPD) and in worse situations lung cancer. Various other conditions fall under COPD such as bronchitis and emphysema (Hough 2014) which the homeless are more susceptible for. Smoking can cause an increase in bronchial secretions and a decrease in mucociliary clearance (Bluman et al 1998) therefore results in an increased effort to clear the patient’s secretions and a longer healing time for infections. There is the added risk of developing pneumonia (Almirall et al 1999) and other chest infections, which can be hard to clear if living in unsanitary, overcrowded areas or sleeping rough in the cold weather.
Physiotherapy can play a significant role in aiding chest clearance and educating those with respiratory conditions (reference). Physiotherapy advice can help to clear the secretions and reduce the work of breathing (Hough 2014). If you suspect that a patient may be suffering from a chest infection you may need to adapt an exercise programme and provide advice as necessary.
Infections[edit | edit source]
Self-harming is very common within the population group, Pluck et al (2013) found that 68% of homeless people have self-harmed at some point. Wounds that are a result of self harming can easily become infected and pose a serious health risk due to them having less accessibility to healthcare facilities.
HIV is common as a result of needle sharing from substance abuse and unprotected sex. Physiotherapy can help with HIV through maintaining and improving their level of physical activity and functional ability (http://www.wcpt.org/node/33479). Furthermore, physiotherapy can also help with preventing complications when appropriate advice and education regarding physical function and physical activity are provided. Physical exercise among the HIV/HEP C population is proven to decrease further chronic health related problems
Soft tissue injuries such as abscess’ and cellulitis are very common infections in the homeless group, particularly if they are injecting drugs into muscular areas. This can also cause muscular injuries which can present as swelling and tenderness around the injected area (Goodman and Synder 2013). This is important to be aware of during the physical assessment, particularly if the injury is presenting as a muscle strain; infact it may just be a side effect of drug use.
Mental Health [edit | edit source]
In this section you will learn about common mental health conditions experienced by homeless people and how these affect them, helping to achieve outcome 2. This section should take 45mins-1hr to complete.
Being in affordable, stable housing has been shown to have a positive impact on general health. Therefore, living in poor housing or being homeless can increase the risks of having a mental health problem or make an existing one worse (Mind 2013). Mental health problems have been found to be a cause of long term rough sleeping and also as a result of becoming and remaining homeless (Homeless Link 2011). Those who are chronically homeless suffer more from mental illness than those who are periodically or newly homeless (Lippert and Lee 2015).
Common Pyshcological Problems[edit | edit source]
Mental health problems amongst the homeless are found to be two times higher compared to those in the general population (Crisis 2009) and that at least half of the homeless population suffer from a mental illness (QNI 2012). Anxiety, depression and mental distress are commonly experienced and these conditions are more prevalent among the homeless than the general population (QNI 2012).
- 1/3 of those living in hostels have been found to have a severe mental health problems such as personality disorders, and that as many as 8 in 10 suffer from anxiety and depression (BBC NEWS 2009).
- Amongst the street homeless, psychotic disorders are found to be 50-100 times higher compared to the general population (Crisis 2009).
- When looking at those who have had a long, uninterrupted spell of homelessness they are shown to have increased anxiety, paranoia and psychosis (Lippert and Lee 2015).
- Adolescent homeless: disruptive behaviour disorder was found to be the most common and this was more prevalent among boys than girls, with the condition decreasing as they got older.
- A third of the adolescent population would qualify for a diagnosis of attention deficit disorder and about a fifth for depression and mania (Cauce et al. 2000).
- Figures for the “hidden” homeless and the conditions commonly experienced by them have not been accounted for (Homeless Link 2011).
All these figures show that mental health is common among the homeless population. However, the prevalence of conditions is quite different amongst the different types of homeless.
Coping Strategies[edit | edit source]
- 44% of the homeless population accessing homelessness services are found to be self medicating with drugs and alcohol
- 14% have self harmed as a result of their mental health problems, compared to 4% of the general population (Homeless Link 2011).
- In the adolescent homeless population 45% admitted to attempting suicide and this was more common amongst girls in comparison to boys (Cauce et al. 2000).
Substance Abuse[edit | edit source]
This next section will complete learning outcome 2 by making you more aware of substance abuse and the problems associated with this within the homeless population. This section will take 1hr to complete.
Substance abuse refers to the intake of alcohol or illicit drugs on a regular basis that affects a person’s cognitive, behavioural and physical abilities (WHO 2015). It is believed that homelessness and substance abuse co-inside and thus should be treated together (Lowe and Gibson 2011). It is unknown whether substance abuse causes the homelessness or whether being homeless leads to substance abuse. Substance abuse can affect one's mental and physical health leading to very specific health care needs that are not necessarily met through mainstream care (Dawes et al 2003). Edens et al (2011) found that there were similar rates of drug abuse between men and women.
The homeless population often turn to substances to cope with various situations (Huntley 2015) or as a way to ‘treat’ their mental health condition (Christiani et al 2008, Bottomley 2001). A study by Healthlink (2004) found that participants from a homeless population who were referred to a methadone programme/alcohol detox programme by their GP did not always attend as accessibility was difficult.
Physiological Changes[edit | edit source]
| Low-Moderate Dose | High Dose |
|
(National Institute of Drug Abuse 2015) |
The short term effects of taking drugs can impact the assessment and treatment techniques used by various health professionals involved in the patients care. Physiotherapists should be aware of these symptoms to provide the best care possible and seek medical attention if deemed necessary. Behavioural red flags including low compliance rate, missing appointments, sudden changes in mood and either excessive fatigue/energy are also signs to be aware of that someone may be taking drugs (Goodman and Snyder 2013). Substance abuse can also cause physiological changes to the body which delays wound and soft tissue healing (Goodman and Snyder 2013). For the elderly the effects extend to memory loss, confusion, tremors and falls.
Stages of Change Model[edit | edit source]
Prochaska and DiClemente's stages of change model (1982) explains one’s readiness for behavioural change. This model consists of five stages: precontemplation, contemplation, planning, action and maintenance. Those who are in precontemplation stage have no intention to change their behaviour (Connors et al. 2012). It could be due to a lack of awareness, unwillingness as well as previous failed attempts. The people in contemplation stage are considering a change in behaviour. They could be thinking about the pros and cons of changing their behaviour. People in the contemplation stage are more likely to seek for assistance and enquire further information on possible solutions.
Study done by Velasquez et al. (2000) shows that majority of the homeless population with alcohol and drug abuse are in precontemplation and contemplation stage. Only 4% of alcohol abusers are in the action stage and are actively trying to quit drinking. (CBT Part)
?? picture of cycle
INTERACTIVE ELEMENT HERE
Accesibility of Health Care[edit | edit source]
By the end of this section you will be able to evaluate the challenges faced by the homeless population with regards to accessing healthcare. To complete this learning outcome, this section on accessibility will take 1hr.
Homeless people are predisposed to multiple health issues which are very much related to their lifestyles. Findings from a national audit Homeless Link (2014), showed that 73% of the surveyed homeless population reported having physical health problems and 90% of them were registered with a General Practitioner (GP). However, a significant amount of them reported not receiving the help for their health issues. More than 15% of the homeless people surveyed were not receiving any support even though they present with physical health problems. Of which, 17.5% of those with mental health problems and 16.5% with alcohol issues seek for support yet they are not receiving it. Of all those being surveyed, 7% of them reported that they had been refused access to a GP or dental care within the past year. With the majority of the homeless population being registered under a GP, health care services should be within reach. In reality, healthcare needs of the homeless people are not met.
Barriers to Accessing Healthcare[edit | edit source]
There are various factors that can contribute to the lack of access to healthcare services in the homeless population. Some intrinsic factors include their fear and denial of poor health, problems communicating their health needs, self-esteem issues and lack of understanding of the health care system. A study done by Geber (1997) shows that 31% of the homeless respondents thought that their medical conditions are not serious enough to see a GP, 11% of them claims that they will “tough it out” by themselves and 8% of them do not think that they are ready to handle their health issues. Some of them felt that they are neglected from the healthcare system and a group of them felt that they were “labelled” (Martin, 2008). Patients who are homeless often describe their experience to the GP as “humiliating” due to insensitive comments made by the GPs and being judged by the practice staffs and by other patients (Pfeil and Howe, 2004). It was also noted that some of the homeless people felt that they are being discharged prematurely even though their medical needs are not resolved (Martins, 2008). Therefore, the homeless population does not have a positive impression of health care services and that the quality of care for them are discriminatory and compromised. As such, many homeless people rather not seek for health care services. A study done by Nickasch and Marnocha (2009) mentioned that the great majority of homeless people have an external locus of control, which means that they attribute their experiences to external circumstances that is beyond their control, such as luck and fate. Having an external locus of control can be one of a major factor that leads to their negative perceptions of the health care services, and therefore deter them from using the services available.
There are also extrinsic factors such as rejection upon visiting the local GP and also the inability to attend consultation during daytime (Lamb & Joels, 2014. BBC, 2001). Healthlink (2004) undertook a survey within the homeless population and asked the participants to describe their experiences within the healthcare system. A number of themes arose within the group including; lack of training and understanding about homelessness, no continuity of care, experiences of stereotyping and discrimination, GP’s not having long enough to look at the patient holistically and a constant feeling of being stigmatised.
However, it is important to note that different countries have different health policies. Due to the limited number of UK research done on the topic of homelessness, some articles from other countries such as Canada and US were referenced above. There will be differences in the perceptions and experiences of the homeless population in regards to health services due to the health policies differences in each countries.
Implications for lack of access[edit | edit source]
Limited health care accessibility for the homeless population can lead to significant social and economic impact on the society. Poor access to health care often lead to delayed clinical presentation and diagnosis (Gelberg, 1990) As a result, many of the medical conditions deteriorate and requires secondary care intervention (Melvin, 2012). This figure contributes to the high estimated cost of £85 million spent on health care for the homeless people annually, which is equivalent to £2,100 per homeless person compared to £525 per person from the general population (Taylor et al., 2012).
Another pertinent issue caused by the lack of accessible health care services for the homeless population is the usage of emergency services. Firstly, people who are homeless do not have a proper housing, putting them at higher risk of being involved in violence, getting victimised on the streets and also predisposes them to contracting diseases such as Hepatitis. (Kushel et al., 2002. Watton and Gallivan, 2013). On top of that, many of the homeless people used the Emergency Department as their only source of health care (Kushel et al., 2002). Those who are not registered to a GP turn up in the Emergency Department for non-emergency complaints (BBC, 2001). One attributing factor to such tendency is that the emergency department provides services all day and it does not require an appointment. Another reason for frequent admissions to the Emergency Department is due to inadequate discharge from health care during the previous hospital visit. This lead to readmission to the hospital shortly after as patients who are homeless find managing their health needs unmanageable on the streets (Homeless Link, St Mungo’s, 2012).
Example[edit | edit source]
Accessibility of health services is a problem faced by the homeless population throughout the UK. An annual service such as <a href="http://www.crisis.org.uk/">Crisis at Christmas</a> offer services for the homeless including physiotherapy. This is a volunteer run service with includes meals, shelter, entertainment and health services over the festive period. In Edinburgh, the Salvation Army provides a weekly service called <a href="http://streetsmartphysio.org/about-us/">StreetSmart</a> that provides physiotherapy for the homeless population. As physiotherapy students and newly qualified physiotherapists this is potentially an area of practice that can be expanded on however we may be treating the homeless population in hospitals.
Key Points and Reflections[edit | edit source]
Based on what was mentioned above, discuss the role of health care professionals in improving the accessibility of health services to the homeless people (20 mins).
Taking into consideration that a great majority of homeless people have external locus of control (e.g. Extracted from Nickasch and Mamocha (2009): “I am totally a victim of my circumstances...right now I lack complete free will...life is dictating me”), recommend ways in which health care professionals can improve on to improve the comfort levels of the homeless people during treatment sessions (20 mins).
Physiotherapy Management [edit | edit source]
Communication
[edit | edit source]
Self-management[edit | edit source]
Implications of practice[edit | edit source]
Practice Techniques[edit | edit source]
Lack of evidence[edit | edit source]
More Information [edit | edit source]
Conclusion [edit | edit source]
References[edit | edit source]
References will automatically be added here, see <a href="Adding References">adding references tutorial</a>.
<span class="fck_mw_references" _fck_mw_customtag="true" _fck_mw_tagname="references" />
<a _fcknotitle="true" href="Category:Physiotherapy">Physiotherapy</a> <a _fcknotitle="true" href="Category:Homelessness">Homelessness</a> <a _fcknotitle="true" href="Category:Physical_Health">Physical_Health</a> <a _fcknotitle="true" href="Category:Mental_Health">Mental_Health</a>