Hip Dysplasia: Difference between revisions
(Undo revision 50462 by Ruben Van Laere (talk)) |
No edit summary |
||
| Line 1: | Line 1: | ||
Definition | Definition | ||
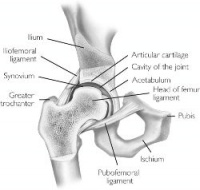
[[Image:Hip.jpg|thumb|right|200px|Hip Joint]] | |||
<br>Developmental dysplasia of the hip is better known as a congenital hip dislocation. It is a collective term for a spectrum of anatomical abnormalities of the hip joint like dislocatability, dislocation or inadequate joint development nearly always diagnosed within the first two years of life. In the joint the articulating bones are displaced which leads to separation of the joint surfaces. There are two types of dislocation: typical and teratological. DDH occurs in approximately 1 in 1000 live births. The dislocation is more common in girls and the left hip is more affected than the right. There is also a chance that the dislocation is bilateral. A hip is unstable when the femoral head is able to move within (subluxated) or outside (dislocated) the confines of the acetabulum.5,6,7 | <br>Developmental dysplasia of the hip is better known as a congenital hip dislocation. It is a collective term for a spectrum of anatomical abnormalities of the hip joint like dislocatability, dislocation or inadequate joint development nearly always diagnosed within the first two years of life. In the joint the articulating bones are displaced which leads to separation of the joint surfaces. There are two types of dislocation: typical and teratological. DDH occurs in approximately 1 in 1000 live births. The dislocation is more common in girls and the left hip is more affected than the right. There is also a chance that the dislocation is bilateral. A hip is unstable when the femoral head is able to move within (subluxated) or outside (dislocated) the confines of the acetabulum.5,6,7 | ||
<br> | |||
Clinically Relevant Anatomy | |||
Clinically Relevant Anatomy | |||
<br>Embryologically, the femoral head and acetabulum develop from the same block of mesenchymal cells. A cleft develops after 7 to 8 weeks and will separate the femoral head from the acetabulum. Postnatal the acetabulum will develop and there will be a growth of the labrum which will deepen the socket. A deep concentric position of the femoral head in the acetabulum is necessary for a normal development of the hip. When the bone structures of the hip are fully grown, we can speak of a ball and socket joint between the rounded head of the femur and the cup-like acetabulum of the femur. 1 | <br>Embryologically, the femoral head and acetabulum develop from the same block of mesenchymal cells. A cleft develops after 7 to 8 weeks and will separate the femoral head from the acetabulum. Postnatal the acetabulum will develop and there will be a growth of the labrum which will deepen the socket. A deep concentric position of the femoral head in the acetabulum is necessary for a normal development of the hip. When the bone structures of the hip are fully grown, we can speak of a ball and socket joint between the rounded head of the femur and the cup-like acetabulum of the femur. 1 | ||
<br> | |||
Etiology | |||
Etiology | |||
<br>There are several causes of DDH. First of all there is the genetically determined joint laxity. This means that ligamentous laxity leads to lack of stability at the hip so that dislocation may easily occur in certain positions of the hip.<br>Furthermore it is possible that in females a ligament relaxing hormone may be secreted by the foetal uterus. This may cause instability in the same way as genetically determined joint laxity. This is probably the reason while this disorder occurs more common in girls than in boys.<br>Finally genetically determined dysplasia of the hip can occur. Due to a defect in the development of the acetabulum and also of the femoral head a dislocation can be developed. 5,6 | <br>There are several causes of DDH. First of all there is the genetically determined joint laxity. This means that ligamentous laxity leads to lack of stability at the hip so that dislocation may easily occur in certain positions of the hip.<br>Furthermore it is possible that in females a ligament relaxing hormone may be secreted by the foetal uterus. This may cause instability in the same way as genetically determined joint laxity. This is probably the reason while this disorder occurs more common in girls than in boys.<br>Finally genetically determined dysplasia of the hip can occur. Due to a defect in the development of the acetabulum and also of the femoral head a dislocation can be developed. 5,6 | ||
<br> | |||
Characteristics/ Clinical presentation | |||
Characteristics/ Clinical presentation | |||
<br>Hip dysplasia will occur during the development of the hip. This means prenatal, during infancy and childhood. In this case the femoral head will be dislocated upwards and laterally from the acetabulum. This is because femoral head in not reduced into the depth of the socket. The femoral neck will be anteverted and the ossific centre for the roof of the acetabulum will develope late. Because of this process the surrounding muscles become contracted and there will be a limited abduction of the hip.5,6 | <br>Hip dysplasia will occur during the development of the hip. This means prenatal, during infancy and childhood. In this case the femoral head will be dislocated upwards and laterally from the acetabulum. This is because femoral head in not reduced into the depth of the socket. The femoral neck will be anteverted and the ossific centre for the roof of the acetabulum will develope late. Because of this process the surrounding muscles become contracted and there will be a limited abduction of the hip.5,6 | ||
| Line 25: | Line 27: | ||
<br>It is important to examine DDH in an early stage. This is not easy because of the lack of a definitive test or finding on examination. The disorder is also painless so there are no symptoms in the infant. Particularly bilateral dislocations are difficult to detect. <br>All newborns are to be screened by physical examination. This examination includes an Ortolani or Barlow test. If the tests are positive, the infant should be referred to an orthopedist.<br>If the test is negative, but no asymmetric skin folds were detected or if the subluxation provocation test is positive, it is recommended that there is a follow up after two weeks by a pediatrician. When he then finds a positive Ortolani test or Barlow test, it is recommended to send the newborn to an orthopedist. If these tests are negative but the provocation test is positive, an ultrasonography is recommended. In most cases, an ultrasonography will provide clarity about the disorder, but it is not recommended to carry out such a test for all newborn. 1,2,8 | <br>It is important to examine DDH in an early stage. This is not easy because of the lack of a definitive test or finding on examination. The disorder is also painless so there are no symptoms in the infant. Particularly bilateral dislocations are difficult to detect. <br>All newborns are to be screened by physical examination. This examination includes an Ortolani or Barlow test. If the tests are positive, the infant should be referred to an orthopedist.<br>If the test is negative, but no asymmetric skin folds were detected or if the subluxation provocation test is positive, it is recommended that there is a follow up after two weeks by a pediatrician. When he then finds a positive Ortolani test or Barlow test, it is recommended to send the newborn to an orthopedist. If these tests are negative but the provocation test is positive, an ultrasonography is recommended. In most cases, an ultrasonography will provide clarity about the disorder, but it is not recommended to carry out such a test for all newborn. 1,2,8 | ||
Medical Management | Medical Management | ||
<br>We need to make a difference between the neonatal cases and the cases where the disorder is examined between 6 months and 6 years. In the case where the dislocation is found on neonatal screening we need to wait 3 weeks to intervene. Sometimes the hip becomes stable spontaneously. In this case it is still important that the child is reexamined at the age of 5 or 6 months. If on the other hand the hip is still unstable after three weeks, splinting in the reduced position in moderate abduction is recommended for a minimum of six weeks or for as long as instability persists. When splinting is needed for a longer period, the risk will increase for the development of avascular necrosis of the femoral head.<br>Between six months and six years there are three essential principles of treatment. First of all to secure the concentric reduction, secondly to provide conditions favorable to continued stability and normal development and thirdly to observe the hips regularly in order to detect any failure of normal development of the acetabulum and to apply appropriate treatment when necessary. <br>If possible, it is important to obtain reduction by non-operative means. Operation can only being used when other methods fail. <br>Closed reduction is often possible in babies up to eighteen months. When DDH is diagnosed later the chances increase that an operation is needed. Closed reduction is the standard practice and will apply weight traction to the limbs with the child either on a frame or in gallows suspension. While traction is maintained gradually to abduct the hips, a little more each day, until 80 degrees of abduction is reached. This will take three to four weeks. 3,5,6,9 | <br>We need to make a difference between the neonatal cases and the cases where the disorder is examined between 6 months and 6 years. In the case where the dislocation is found on neonatal screening we need to wait 3 weeks to intervene. Sometimes the hip becomes stable spontaneously. In this case it is still important that the child is reexamined at the age of 5 or 6 months. If on the other hand the hip is still unstable after three weeks, splinting in the reduced position in moderate abduction is recommended for a minimum of six weeks or for as long as instability persists. When splinting is needed for a longer period, the risk will increase for the development of avascular necrosis of the femoral head.<br>Between six months and six years there are three essential principles of treatment. First of all to secure the concentric reduction, secondly to provide conditions favorable to continued stability and normal development and thirdly to observe the hips regularly in order to detect any failure of normal development of the acetabulum and to apply appropriate treatment when necessary. <br>If possible, it is important to obtain reduction by non-operative means. Operation can only being used when other methods fail. <br>Closed reduction is often possible in babies up to eighteen months. When DDH is diagnosed later the chances increase that an operation is needed. Closed reduction is the standard practice and will apply weight traction to the limbs with the child either on a frame or in gallows suspension. While traction is maintained gradually to abduct the hips, a little more each day, until 80 degrees of abduction is reached. This will take three to four weeks. 3,5,6,9 | ||
Physical Therapy Management | Physical Therapy Management | ||
<br>The traditional physical therapy includes ball catching, ball bouncing, target throwing, kicking, balance beam activities, gait and stairs and unleveled terrain, running and jumping as well as sensory integration activities including swiss ball, vestibular swing tasks and scooter board.<br>In addition, there is another therapy called hippotherapy. The protocol for hippotherapy includes riding a forward, backward, and side saddle position while the horse walked in a four beat gait moving in a serpentine and figure eight patters. Ball throwing and catching on the horse while stationary as well as ring tossing and placing. The session ends with the horse trotting while the subject faced forward working on advanced balance and core control. | <br>The traditional physical therapy includes ball catching, ball bouncing, target throwing, kicking, balance beam activities, gait and stairs and unleveled terrain, running and jumping as well as sensory integration activities including swiss ball, vestibular swing tasks and scooter board.<br>In addition, there is another therapy called hippotherapy. The protocol for hippotherapy includes riding a forward, backward, and side saddle position while the horse walked in a four beat gait moving in a serpentine and figure eight patters. Ball throwing and catching on the horse while stationary as well as ring tossing and placing. The session ends with the horse trotting while the subject faced forward working on advanced balance and core control. | ||
| Line 37: | Line 39: | ||
- Primaire bronnen | - Primaire bronnen | ||
1. American Academy of Pediatrics, Committee on Quality Improvement, Subcommittee on Developmental Dysplasia of the Hip, Clinical Practice Guideline : Early detection of developmental Dysplasia of the hip, Offical Journal of the American Academy of Pediatrics Vol 105 No 4 April 2000, downloaded from pediatrics. Applications.org at Swets Blackwell 30680247 on November 23, 2011. | 1. American Academy of Pediatrics, Committee on Quality Improvement, Subcommittee on Developmental Dysplasia of the Hip, Clinical Practice Guideline : Early detection of developmental Dysplasia of the hip, Offical Journal of the American Academy of Pediatrics Vol 105 No 4 April 2000, downloaded from pediatrics. Applications.org at Swets Blackwell 30680247 on November 23, 2011. | ||
<br>Level of evidence: 1 A | <br>Level of evidence: 1 A | ||
<br>2. Andreas Roposch, Liang Q. Liu, Fritz Hefti, M. P. Clarke, John H. Wedge, Standardized Diagnostic Criteria for Developmental Dysplasia of the Hip in Early Infancy, Clinical Orthopaedics and Related Research (2011) 469:3451 – 3461. | <br>2. Andreas Roposch, Liang Q. Liu, Fritz Hefti, M. P. Clarke, John H. Wedge, Standardized Diagnostic Criteria for Developmental Dysplasia of the Hip in Early Infancy, Clinical Orthopaedics and Related Research (2011) 469:3451 – 3461. | ||
<br>Level of evidence: 1 B | <br>Level of evidence: 1 B | ||
<br>3. Christian Tschauner, Frank Fürntrath, Yasaman Saba, Andrea Berghold, Roman Radl, Developmental dysplasia of the hip : impact of sonographic newborn hip screening on the outcome of early treated decentered hip joints – a single center retrospective comparative cohort study based on Graf’s method of hip ultrasonography; J. Child Orthop (2011) 5:415-424. | <br>3. Christian Tschauner, Frank Fürntrath, Yasaman Saba, Andrea Berghold, Roman Radl, Developmental dysplasia of the hip : impact of sonographic newborn hip screening on the outcome of early treated decentered hip joints – a single center retrospective comparative cohort study based on Graf’s method of hip ultrasonography; J. Child Orthop (2011) 5:415-424. | ||
<br>Level of evidence: 1 B | <br>Level of evidence: 1 B | ||
<br>4. Roy Aldridge, Farley Schweighart, Megan Easley, Blair Wagoner, Performance and Function in an individual with bilateral developmental dysplasia of the Hip, JPT. 2011; 2(2): 54-63 | <br>4. Roy Aldridge, Farley Schweighart, Megan Easley, Blair Wagoner, Performance and Function in an individual with bilateral developmental dysplasia of the Hip, JPT. 2011; 2(2): 54-63 | ||
. <br>Level of evidence: 3 B | . <br>Level of evidence: 3 B | ||
<br> | |||
- Secundaire bronnen | |||
<br>5. John Crawford Adams, David L. Hamblem, Outline of Orthopaedics, Churcill Livingstone, 1995, twelfth edition, p. 292 – 301. | |||
<br>5. John Crawford Adams, David L. Hamblem, Outline of Orthopaedics, Churcill Livingstone, 1995, twelfth edition, p. 292 – 301. | |||
<br>6. John Crawford Adams, David L. Hamblem, Outline of Orthopaedics, Churcill Livingstone, 2001, thirteenth edition, p. 305 – 312. | <br>6. John Crawford Adams, David L. Hamblem, Outline of Orthopaedics, Churcill Livingstone, 2001, thirteenth edition, p. 305 – 312. | ||
<br>7. Hema Patel, with the Canadian Task Force on Preventive Health Care, Preventive Health care, 2001 update: screening and management of developmental dysplasia of the hip in newborns, Cmaj, June 12, 2001; 164 (12), p. 1669 -1677. | <br>7. Hema Patel, with the Canadian Task Force on Preventive Health Care, Preventive Health care, 2001 update: screening and management of developmental dysplasia of the hip in newborns, Cmaj, June 12, 2001; 164 (12), p. 1669 -1677. | ||
<br>8. Harry B. Skinner, Current : Diagnosis and treatment in Orthopedics, McGraw Hill Medical Publishing Division, 2000, second edition, p.1537 – 1540. | <br>8. Harry B. Skinner, Current : Diagnosis and treatment in Orthopedics, McGraw Hill Medical Publishing Division, 2000, second edition, p.1537 – 1540. | ||
<br>9. Lawrence W. Way, Current : Surgical Diagnosis and Treatment, Prentice Hall International, 1994, tenth edition, p. 1085 – 1087.<br> | <br>9. Lawrence W. Way, Current : Surgical Diagnosis and Treatment, Prentice Hall International, 1994, tenth edition, p. 1085 – 1087.<br> | ||
Revision as of 03:34, 5 May 2013
Definition
Developmental dysplasia of the hip is better known as a congenital hip dislocation. It is a collective term for a spectrum of anatomical abnormalities of the hip joint like dislocatability, dislocation or inadequate joint development nearly always diagnosed within the first two years of life. In the joint the articulating bones are displaced which leads to separation of the joint surfaces. There are two types of dislocation: typical and teratological. DDH occurs in approximately 1 in 1000 live births. The dislocation is more common in girls and the left hip is more affected than the right. There is also a chance that the dislocation is bilateral. A hip is unstable when the femoral head is able to move within (subluxated) or outside (dislocated) the confines of the acetabulum.5,6,7
Clinically Relevant Anatomy
Embryologically, the femoral head and acetabulum develop from the same block of mesenchymal cells. A cleft develops after 7 to 8 weeks and will separate the femoral head from the acetabulum. Postnatal the acetabulum will develop and there will be a growth of the labrum which will deepen the socket. A deep concentric position of the femoral head in the acetabulum is necessary for a normal development of the hip. When the bone structures of the hip are fully grown, we can speak of a ball and socket joint between the rounded head of the femur and the cup-like acetabulum of the femur. 1
Etiology
There are several causes of DDH. First of all there is the genetically determined joint laxity. This means that ligamentous laxity leads to lack of stability at the hip so that dislocation may easily occur in certain positions of the hip.
Furthermore it is possible that in females a ligament relaxing hormone may be secreted by the foetal uterus. This may cause instability in the same way as genetically determined joint laxity. This is probably the reason while this disorder occurs more common in girls than in boys.
Finally genetically determined dysplasia of the hip can occur. Due to a defect in the development of the acetabulum and also of the femoral head a dislocation can be developed. 5,6
Characteristics/ Clinical presentation
Hip dysplasia will occur during the development of the hip. This means prenatal, during infancy and childhood. In this case the femoral head will be dislocated upwards and laterally from the acetabulum. This is because femoral head in not reduced into the depth of the socket. The femoral neck will be anteverted and the ossific centre for the roof of the acetabulum will develope late. Because of this process the surrounding muscles become contracted and there will be a limited abduction of the hip.5,6
Diagnostic procedures
It is important to examine DDH in an early stage. This is not easy because of the lack of a definitive test or finding on examination. The disorder is also painless so there are no symptoms in the infant. Particularly bilateral dislocations are difficult to detect.
All newborns are to be screened by physical examination. This examination includes an Ortolani or Barlow test. If the tests are positive, the infant should be referred to an orthopedist.
If the test is negative, but no asymmetric skin folds were detected or if the subluxation provocation test is positive, it is recommended that there is a follow up after two weeks by a pediatrician. When he then finds a positive Ortolani test or Barlow test, it is recommended to send the newborn to an orthopedist. If these tests are negative but the provocation test is positive, an ultrasonography is recommended. In most cases, an ultrasonography will provide clarity about the disorder, but it is not recommended to carry out such a test for all newborn. 1,2,8
Medical Management
We need to make a difference between the neonatal cases and the cases where the disorder is examined between 6 months and 6 years. In the case where the dislocation is found on neonatal screening we need to wait 3 weeks to intervene. Sometimes the hip becomes stable spontaneously. In this case it is still important that the child is reexamined at the age of 5 or 6 months. If on the other hand the hip is still unstable after three weeks, splinting in the reduced position in moderate abduction is recommended for a minimum of six weeks or for as long as instability persists. When splinting is needed for a longer period, the risk will increase for the development of avascular necrosis of the femoral head.
Between six months and six years there are three essential principles of treatment. First of all to secure the concentric reduction, secondly to provide conditions favorable to continued stability and normal development and thirdly to observe the hips regularly in order to detect any failure of normal development of the acetabulum and to apply appropriate treatment when necessary.
If possible, it is important to obtain reduction by non-operative means. Operation can only being used when other methods fail.
Closed reduction is often possible in babies up to eighteen months. When DDH is diagnosed later the chances increase that an operation is needed. Closed reduction is the standard practice and will apply weight traction to the limbs with the child either on a frame or in gallows suspension. While traction is maintained gradually to abduct the hips, a little more each day, until 80 degrees of abduction is reached. This will take three to four weeks. 3,5,6,9
Physical Therapy Management
The traditional physical therapy includes ball catching, ball bouncing, target throwing, kicking, balance beam activities, gait and stairs and unleveled terrain, running and jumping as well as sensory integration activities including swiss ball, vestibular swing tasks and scooter board.
In addition, there is another therapy called hippotherapy. The protocol for hippotherapy includes riding a forward, backward, and side saddle position while the horse walked in a four beat gait moving in a serpentine and figure eight patters. Ball throwing and catching on the horse while stationary as well as ring tossing and placing. The session ends with the horse trotting while the subject faced forward working on advanced balance and core control.
References
- Primaire bronnen
1. American Academy of Pediatrics, Committee on Quality Improvement, Subcommittee on Developmental Dysplasia of the Hip, Clinical Practice Guideline : Early detection of developmental Dysplasia of the hip, Offical Journal of the American Academy of Pediatrics Vol 105 No 4 April 2000, downloaded from pediatrics. Applications.org at Swets Blackwell 30680247 on November 23, 2011.
Level of evidence: 1 A
2. Andreas Roposch, Liang Q. Liu, Fritz Hefti, M. P. Clarke, John H. Wedge, Standardized Diagnostic Criteria for Developmental Dysplasia of the Hip in Early Infancy, Clinical Orthopaedics and Related Research (2011) 469:3451 – 3461.
Level of evidence: 1 B
3. Christian Tschauner, Frank Fürntrath, Yasaman Saba, Andrea Berghold, Roman Radl, Developmental dysplasia of the hip : impact of sonographic newborn hip screening on the outcome of early treated decentered hip joints – a single center retrospective comparative cohort study based on Graf’s method of hip ultrasonography; J. Child Orthop (2011) 5:415-424.
Level of evidence: 1 B
4. Roy Aldridge, Farley Schweighart, Megan Easley, Blair Wagoner, Performance and Function in an individual with bilateral developmental dysplasia of the Hip, JPT. 2011; 2(2): 54-63
.
Level of evidence: 3 B
- Secundaire bronnen
5. John Crawford Adams, David L. Hamblem, Outline of Orthopaedics, Churcill Livingstone, 1995, twelfth edition, p. 292 – 301.
6. John Crawford Adams, David L. Hamblem, Outline of Orthopaedics, Churcill Livingstone, 2001, thirteenth edition, p. 305 – 312.
7. Hema Patel, with the Canadian Task Force on Preventive Health Care, Preventive Health care, 2001 update: screening and management of developmental dysplasia of the hip in newborns, Cmaj, June 12, 2001; 164 (12), p. 1669 -1677.
8. Harry B. Skinner, Current : Diagnosis and treatment in Orthopedics, McGraw Hill Medical Publishing Division, 2000, second edition, p.1537 – 1540.
9. Lawrence W. Way, Current : Surgical Diagnosis and Treatment, Prentice Hall International, 1994, tenth edition, p. 1085 – 1087.