Anatomy Slings and Their Relationship to Low Back Pain
Introduction[edit | edit source]
The following wiki page will aim to investigate the body’s anatomical slings and the ways in which a dysfunction could potentially result in lower back pain. We will be discussing the stability of the lumbo-pelvic complex and the systems (both local and global) which govern it. We will also attempt to present the literature available in this underreported, but essential, area of dynamic stability whilst providing a detailed breakdown which will include exercises to target the individual myofascial slings.
Dr Joseph Shepherd is an expert and module lead lecturer in the field of dynamic global movement, and strength and conditioning. In the following video, he introduces the concept of viewing the body as a whole, and the implications that a limited approach may have.The authors of this article hope that the information on this page helps the reader better understand stability, and that it may influence a more comprehensive approach to instability and lower back pain.
Stability in the Lumbo-Pelvic Region[edit | edit source]
As human beings our bodies are subject to constantly changing demands placed upon us by the external environment. Therefore, the ability to adapt our bodies in order to cope with these varying stresses is vital in order to protect internal structures. The lumbo-pelvic complex plays a key role in distributing load and maintaining stability during movement and changes in external demands. The primary function of this unit is to allow the transfer of forces safely in order to allow complex movement, without injury, and whilst facilitating efficient respiratory function[2]. It helps aid the prevention of injury to vital structures such as the spinal cord, as well as the bony and soft tissue structures of the area.
When investigated in an in-vitro environment, it has been estimated that the human spine can withhold loads of approximately 90N before buckling. However, research suggests that in functioning human beings this load can reach up to 1500N. This indicates a heavy dependence upon other structures in order to provide the stability required to cope with the forces that the spine is subjected to in reality. The relationship between the sacrum, pelvis and lumbar spine, alongside their surrounding structures, is fundamental to stability. The contribution of the design and structure of pelvic anatomy to stability is known as sacroiliac joint form closure. As alluded to before, the bony structure of the spine and pelvis alone is insufficient to deal with the forces the body is exposed to. Therefore, other structures such as ligaments, muscles, and fascia are required to distribute forces across the region. This is known as force closure of the sacroiliac joint [3].
A model for explaining stability of the spine was devised by Panjabi in 1992, and comprises of three components. The spinal column and its structural anatomy as described using the sacroiliac form closure theory is the first component, and is seen as a passive stabiliser. Secondly, the neural control unit is perceived as fundamental in order to mediate responses to movement and adapt spinal stability as required. The final component, as proposed by Panjabi is the muscular system, is an active stabiliser which consists of global and local muscle units[4].
In spite of this theory, there is still discrepancy within the literature as to the contributors to spinal stability. A core stabilisation approach is commonly used by clinicians in order to treat pain in the spinal region. As purported by Norris (2008), this perspective focuses more on intrinsic mono or bi-articular muscles as primary stabilisers of the spine, and pays little attention to global systems[5].
A significantly broader approach is becoming increasingly common within the literature. This perspective considers the force closure stability mechanism as a complex system of selective co-contraction, between the deep and superficial muscles of the lumbo-pelvic region. It is believed that the term ‘control’ holds greater aptitude than ‘stability’, as it pertains to the constantly changing contribution of intrinsic and extrinsic muscles, and the ongoing mediation by the central nervous system (CNS)[6]. It is believed that in order to achieve functional control, the CNS has the ability to dampen some systems whilst exciting others; this may in fact result in reduced ‘stability’ in sacrifice for greater mobility[2][6].
The CNS has multiple strategies at its disposal, and utilises these depending upon the quantity of stabilisation required, the predictability of movement, and the risk to the bodily structures[2]. Work carried out by Richardson (2002) upon subjects who carried out sacroiliac stability exercises in a static position, found a lower sacroiliac joint (SIJ) laxity when intrinsic muscles were contracted, compared to more superficial muscles[7]. This demonstrates that different roles are played by the varying muscular groups in order to achieve optimal control. Another example of this is the recruitment of the intrinsic muscles when anticipating movement. The slow-twitch, type one fibres in the multifidus, for example, will be stimulated by the CNS to contract when a change in posture is predicted[8].
Within this harmony of stability control a different approach can be taken when viewing the more extrinsic and global musculature of the lumbo-pelvic region, and this will be explored in the further in the subsequent sections.
Myofascial Slings[edit | edit source]
Serge Gracovetsky offered a theory of human motion which he called “The Spinal Engine”, (Gracovetsky 1988, revised: 2008) stating that quadruple amputees could “walk” on the bones at the base of their pelvises. He reasoned that spinal rotation and the muscle systems around the lumbo-pelvic region might be at the base of human movement. Thus, the efficiency and harmony of these muscle systems is very significant, as the limbs merely amplify movement that originates in the musculature of the spine and trunk. It has since been proposed and developed from this, by the likes of Andry Vleeming, Diane Lee, and Thomas Myers, that anatomy slings are a large part of these systems and our ability to generate efficient dynamic movement.
As noted above, the superficial muscle activity should occur in synergy with the deep muscles, which is an integral part of dynamic movement. Anatomy slings can be otherwise known as the ‘myofascial slings’ and relate very closely to superficial muscle activity (PANJABI). Anatomy slings were first described by Vleeming, and the term ‘myofascial’ relates to the structures involved within a sling. Anatomy slings aren’t comprised by only one type of tissue; they are comprised of muscles, fascia and ligaments all working together to create stability and mobility (Vleeming et al 1993). Is critical to understand how they connect and function together.
A muscle contraction produces a force that spreads beyond the origin and insertion of the active muscle (Brown and McGill, 2009). These forces are transmitted through structures within an anatomical sling, allowing forces to be produced quite distant from the origin of the initial muscle contraction; this can be referred to as a force vector. The muscles depicted within a myofascial sling are connected via facia to produce these force vectors that assist in the transfer of load within the pelvis and lumbar spine. These muscles within a myofascial sling may overlap and interconnect with other slings depending on the change in force vectors needed for a competent dynamic movement. When the force vectors are balanced, they provide optimal alignment of the bones and joints throughout dynamic movement. In contrast, imbalanced force vectors resulting from altered tension in the myofascial slings, can create malalignment and potentially contribute to loss of stability during static or dynamic tasks[2].
The body is a complex system made up of many of these anatomical slings. As explained above, when the slings are working efficiently. They also help us move better, produce more force, and create more speed[9]. However, when there is a weak component in the sling, clinicians don’t often address the slings, but rather the muscles individually and a person’s general movement pattern. An understanding of this is becoming increasingly important for clinicians failing to recognise the integral role of anatomy slings (Brookbush, 2013).
In physiotherapist Diane Lee’s book, The Pelvic Girdle (2011), she discusses four important sling systems that work together for load transfer through the pelvic/ lumbar region. A “hole” or weakness of a component in any of these systems can create dysfunction and resulting poor performance and/or injury[2].
Anterior Oblique Sling[edit | edit source]
The anterior oblique system (AOS) consists of the external oblique, internal oblique and the transversus abdominis via the rectus sheath, connecting with contralateral adductor muscles via the adductor-abdominal fascia (See image A1 - red arrows). When this group of muscles contract together, it provides stability by acting like an abdominal binder, compressing the entire pelvic girdle, resulting in force closure of the symphysis pubis. When working interchangeably with the other AOS (See image A1 - yellow arrows), and in harmony with other slings, it will also cause relative movement of the pelvis[2].
Image A1: The two Anterior Oblique Systems supporting the pelvis, as described by Vleeming and Lee.
When walking, the AOS is important in providing stability. The adductors work in harmony with the internal oblique and opposite external oblique muscles, utilising a balance of force vectors to both stabilise the body on top of the stance leg and to rotate the pelvis forward. This is to position the pelvis and hip optimally for the succeeding heel-strike[9] (See image A2). Basmajan (1967) concluded this when looking at the EMG recordings of the oblique abdominals during gait. It was clear in his findings that both sets of muscles, together, contribute to stability at the initiation of the stance phase of gait, as well as to rotating the pelvis and pulling the leg through during the swing phase. His findings also supported that as the speed of walking progresses to running, activation of the anterior oblique system becomes more prominent. The opposite AOS will be working in reciprocity, lengthening whilst the on shown in Image A2 is shortening in order to allow the hip to extend back, with control (Vleeming, 1998).
The demands on the AOS are great in multi-directional sports such as tennis, soccer, football, basketball, rugby and hockey. In such sporting environments, the AOS must not only contribute to accelerating the body, but also to rotating and decelerating it during the change of direction (Brookbush, 2013). Accelerating, decelerating and changing directions are all activities that result in immediate pain in the presence of both abdominal and groin strains or tears, which strongly suggests a link within the AOS and its function.
Image A2: To show the adductors working in harmony with the internal oblique and opposite external oblique abdominal muscles to support the pelvis when walking.
Static resistance and isometric training like planks and crunches can be used to strengthen isolated parts of the AOS, much like strengthening specific body parts. This is beneficial when addressing a specific dysfunction within an anatomy sling that has been identified. However, dynamic training utilises whole anatomy slings. This is more appropriate, allowing us to cope with stresses and demands placed upon us throughout dynamic movements. An example of more dynamic exercises incorporating the AOS are Russian twists and hill sprints (Brookbush, 2013) (Page et al, 2010).
The AOS can be trained and appreciated when running in sand due to the fact that sand gives way during the initiation of the stance and following contact phases of gait. The ground reaction force that aids dynamic movement is disrupted, resulting in poor use of the thoracolumbar fascia and posterior systems. This increases activation of the AOS to compensate for the lost kinetic potential and muscular energy of the posterior systems, in turn, making it a good way to train the AOS. It is important to know that this increased work may result in injury, especially if there is an underlying dysfunction within the AOS. (Gracovetsky, 2008).
Posterior Oblique Sling[edit | edit source]
Evolution has seen human beings develop from quadrupedal into bipedal creatures. This adaptation has allowed us to carry out tasks at a more advanced level than we would have done previously, however, has also brought about changing demands upon the body. This has meant that the body has had to adapt in order to cope with different stresses. With the transformation of humans into upright-functioning beings, the demand upon the posterior structures of the body has changed dramatically, and these have had to adapt accordingly. For example, the gluteus maximus has evolved from a relatively small muscle (as observed in chimpanzees) to being the largest muscle in the body (Vleeming 2012). It has become part of a system which is specialised and integral in supporting functional control in movements such as human gait – the posterior oblique muscle sling (POS).
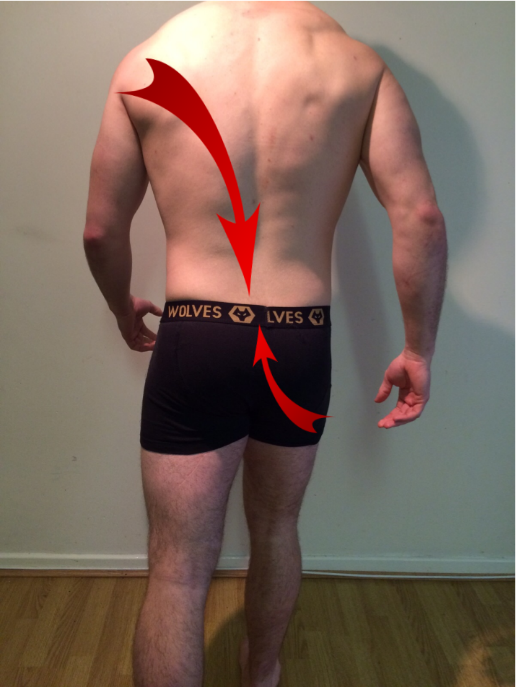
This sling system consists of the latissimus dorsi (LD), the gluteus maximus (GM), and the inter-connecting thoracolumbar fascia (TLF)[2]. The POS, otherwise known as the back functional line, crosses approximately at the level of the sacro-lumbar junction. The lower portion of the sling, consisting of the distal GM fibres, passes underneath the iliotibial tract to attach to the posterolateral edge of the femur, thus this system becomes linked with the lateral sling[10]. Within recent decades’ clinicians have begun to identify that stability is a complex phenomenon, and “a system of assisting movement whilst stabilising” exists (Vleeming 1995). The POS is fundamental to this method of functioning.
Image P1: The posterior oblique sling consists of the latissimus dorsi, contralateral gluteus maximus, and the inter-connecting thoraco-lumbar fascia.
The role of the POS is most distinguished during the single support (stance) phase of gait. Prior to heel strike, the ipsilateral hamstring muscle contracts in order to prepare the limb for weight-bearing. During this, the proximal hamstring also carries the role of stabilising the ipsilateral pelvis against the activity of the quadriceps, in order to prevent excessive anterior rotation of the ilium. However, once heel strike occurs, hamstring activity diminishes and its role of limiting ilium movement is largely undertaken by the GM. At this point the muscle is in a lengthened position. Simultaneously, counter-rotation of the trunk also begins to takes place. During this process, the arm contra-lateral to the stance leg is ante-flexed, undergoing an eccentric contraction of the LD in order to control the forward momentum of the limb, whilst taking the LD also into a lengthened position[11][9]. The propulsive phase of gait then follows, with both the GM and contralateral LD concentrically contracting from a lengthened to shortened position, resulting in extension of the arm with the opposite propelling leg. When these two simultaneously occurring mechanisms are coupled, a contraction of GM alongside its contralateral LD is observed[9]. As discussed previously, this causes an increase in tension within the TLF, eliciting stabilisation of the SIJ and lumbar spine[2]. This theory also adds credence to the remark that weakening of the GM aspect of the POS often results in hamstring dysfunction, due to the compensatory activity in order to stabilise the ilium (Sahrmann 2012).
Image P2: Shows the direction of force created by the POS during gait.
As well as the SIJ compressional stability that this system produces through the TLF, some authors also believe that the mechanism acts a ‘smart spring’, using phasic contractions to release and store energy during gait. Vleeming theorises that kinetic energy is built up in the GM and LD as they lengthen prior to and during heel strike, respectively. This energy is then released as these muscles shorten immediately following the lengthening phase, causing this kinetic energy to be released[11]. A similar response is observed when a finger rapidly returns to a neutral position, when it is released following passive full extension. There is debate surrounding whether this kinetic energy is stored within the muscles or the TLF (Dorman 1992). Regardless of this, it is widely believed that this mechanism reduces energy expenditure of surrounding muscles of locomotion, thus reducing the metabolic cost of gait[11][9].
Traditional exercise training to stabilise the SIJ focuses on ‘core’ units, often with the aim of isolating muscles in order to strengthen them. As discussed in the section “Stability in the Lumbo-Sacral Region” the demands upon human beings suggest that strengthening techniques should be incorporated into dynamic movements. Thus, in order to train the POS, the GM and LD should not be viewed in isolation, rather utilised in synergy with each other to promote efficient gait as described previously. A good example of an exercise that can be used for treating POS dysfunction is the reverse lunge. A therapist should utilise this once a patient can achieve pain-free hip motion and satisfactory static stability (Nickelston 2013). A demonstration of this exercise is shown in the video below:
As alluded to previously, it is vital that the muscle slings of the body function harmoniously in order to facilitate efficient movement and prevent injury. This is especially pertinent between the anterior oblique sling (AOS) and the POS. These systems can be viewed similarly to a muscle pair, with an antagonist and an agonist: whilst one is contracting, the other may work to control the movement being produced. An example of this in the AOS and POS is during the swing of a tennis racket. The movement and power is produced by the AOS which causes a rotation and forward movement of the pelvis, trunk and arm. However, the POS is also crucial during this action in order decelerate the movement when appropriate, using eccentric control. This helps to aid an individual in maintaining their balance during a highly dynamic movement such as this, whilst stabilising the lumbo-pelvic hip complex[10].
Deep Longitudinal Sling[edit | edit source]
Lateral Sling[edit | edit source]
The anatomy of the lateral sling consists of the gluteus medius, gluteus minimus, tensor fascia latae (TFL) and iliotibial band (ITB)[2]. The lateral sling begins at the origin of the gluteus medius and minimus on the external surface of the ilium, and ends at the insertion of the ITB on the upper tibia. This gives the lateral sling broad coverage of the lateral aspect of the hip and knee joint. IMAGE 1 IMAGE 2
[[Image:{Lateral_Sling_12.png}|{width}px]][[Image:{Lateral_Sling_2.png}|{width}px]]
According to Drake et al (2015), the deep fascia in the lower limb forms a thick ‘stocking-like’ membrane which covers the limb. The fascia is thicker in the thigh and gluteal region and is called the fascia lata. This fascia lata is thickened on the lateral side of the thigh and forms the ITB, which is an integral part of the lateral sling. The muscle fibres of the gluteus medius and minimus blend with the connecting fascia to the TFL. The TFL is partially enclosed by and inserts into the superior aspect of the ITB. This interconnecting nature of the lateral sling allows it to work together and act as a unit to provide stability.
The lateral sling is used in coronal plane stability and is involved in pelvo-femoral stability in dynamic movements such as gait, lunges and stair climbing. In order to understand the relevance of the sling, the action of the muscles needs to be understood. The gluteus medius and minimus are hip abductors and medial rotators whilst the TFL works in synergy with these muscles to hold the pelvis level in single leg movements. Additionally, the TFL works with the gluteus maximus on the ITB to stabilise the hip joint by holding the head of the femur in the acetabulum (Drake, 2015).
Functionally, the pelvic girdle should be neutral in all three planes: coronal, sagittal and transverse. During movements involving single leg stance, such as walking, the lateral sling comes into tension to maintain the pelvis stable over the stance leg, preventing pelvic drop on the opposite side of the pelvis. Failed control by the lateral sling often presents as a hip drop/ trendelenburg sign during stance phase of gait and single leg stance. A compensation for a trendelenburg is to side flex the trunk to the affected side to maintain the level of the pelvis. IMAGE 3
Maintaining a neutral pelvis is vital in correct alignment of the lower limb during movement; ensuring your hip lines up with your knee and knee lines up with your toes. This alignment allows the joints to be in their best functional positioning and allows the muscles to work in their optimal range. This ensures that the forces going through the region are distributed appropriately and not putting excessive strain on the structures.
An example of a strengthening exercise for the lateral sling is a single leg squat.
How Do These Link to Low Back Pain?[edit | edit source]
Conclusion[edit | edit source]
References[edit | edit source]
- ↑ Dr Joseph Shepherd: Introduction to Anatomy Slings. Available at: https://www.youtube.com/watch?v=GcgUtkDLSvc
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 Lee, D; Vleeming, A; Jones, M. The Pelvic Girdle: An Integration of Clinical Expertise and Research. Edinburgh: Elsevier/Churchill Livingstone, 2011.
- ↑ Hoffman, J; Gabel, P. Expanding Panjabi’s stability model to express movement: A theoretical model. Medical Hypotheses, Volume 80, 2013. Pages 692-697.
- ↑ Panjabi, M. The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. Journal of Spinal Disorders, Volume 5, Issue 4, 1992. Pages 383-389.
- ↑ Norris, C. Back Stability: Integrating Science and Therapy, Second Edition. USA: Human Kinetics, 2008.
- ↑ 6.0 6.1 Reeves, P; Narendrac, K; Cholewicki, J. Spine stability: the six blind men and the elephant. Clinical Biomechanics. Bristol, Avon, Volume 22, Issue 3, 2007. Pages 266-274.
- ↑ Richardson, CA; Snijders, CJ; Hides, JA; Damen, L; Pas, MS; Storm, J. The relation between the transversus abdominis muscles, sacroiliac joint mechanics, and low back pain. Spine, Volume 27, Issue 4; 2002. Pages 399-405.
- ↑ Currie, S; Myers, C; Davidson, B; Enebo, B. Anticipatory Activation of the Erector Spinar and Multifidus in Patients With and Without Low Back Pain. Pain Journal, Volume 74, Issue 33, 2012. Pages 64-65.
- ↑ 9.0 9.1 9.2 9.3 9.4 Chek, P. Core Stability: The Outer Unit. International Association of Athletics Federations, NSA 1-2.00, 2011.
- ↑ 10.0 10.1 Myers, T. Anatomy Trains, Third Edition. UK: Churchill Livingstone, 2013.
- ↑ 11.0 11.1 11.2 Vleeming, A; Mooney, V; Stoeckart, R. Movement, Stability & Lumbopelvic Pain, Integration of Research and Therapy. UK: Churchill Livingstone, 2007
- ↑ Dynamic Chiropractic: The Reverse Lunge. Available from: https://www.youtube.com/watch?v=MPV_ZAf7ITw