Ankle Sprain: Difference between revisions
mNo edit summary |
mNo edit summary |
||
| Line 10: | Line 10: | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
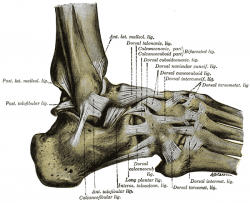
An ankle sprain is a common injury in which one or more of the ankle ligaments is torn or partially torn. Inversion ankle sprains are the most common making up 85% of all ankle sprains. The most commonly torn ankle ligament is the anterior talofibular ligament (ATFL) which is on the lateral aspect of the ankle. | An ankle sprain is a common injury in which one or more of the ankle ligaments is torn or partially torn. Inversion ankle sprains are the most common, making up 85% of all ankle sprains. The most commonly torn ankle ligament is the anterior talofibular ligament (ATFL) which is on the lateral aspect of the ankle. | ||
{| width="40%" cellspacing="1" cellpadding="1" border="0" align="center" class="FCK__ShowTableBorders" | {| width="40%" cellspacing="1" cellpadding="1" border="0" align="center" class="FCK__ShowTableBorders" | ||
|- | |- | ||
| [[Image:Ankle.png|thumb|left|250px|Ankle Complex]] | | [[Image:Ankle.png|thumb|left|250px|Ankle Complex]] | ||
| | | <br> | ||
| align="right" | | | align="right" | | ||
{{#ev:youtube|_u5w856Yjvg|250}} <ref> Dr Glass DPM. Ankle Sprain Injury Explained. Available from: http://www.youtube.com/watch?v=_u5w856Yjvg [last accessed 28/08/12]</ref> | {{#ev:youtube|_u5w856Yjvg|250}} <ref> Dr Glass DPM. Ankle Sprain Injury Explained. Available from: http://www.youtube.com/watch?v=_u5w856Yjvg [last accessed 28/08/12]</ref> | ||
| Line 23: | Line 23: | ||
== Epidemiology /Etiology == | == Epidemiology /Etiology == | ||
The most common mechanism of injury for an ankle sprain involving the lateral aspect of the ankle (commonly called a lateral | The most common mechanism of injury for an ankle sprain involving the lateral aspect of the ankle (commonly called a lateral or inversion ankle sprain) is when the foot is forced into a combined movement of plantarflexion and inversion. In this situation the ankle would roll into an outward direction with the foot and toes moving inward toward the midline of the body. <br> | ||
A less common mechanism of injury involves a forceful eversion movement at the ankle | A less common mechanism of injury involves a forceful eversion movement at the ankle, resulting in injury to the strong [[Deltoid ligament complex|deltoid ligament complex]]. | ||
{| width="60%" cellspacing="1" cellpadding="1" border="0" align="center" | {| width="60%" cellspacing="1" cellpadding="1" border="0" align="center" | ||
| Line 49: | Line 49: | ||
== Differential Diagnosis<br> == | == Differential Diagnosis<br> == | ||
[[Ottawa Ankle Rules|The Ottawa ankle rules]] | [[Ottawa Ankle Rules|The Ottawa ankle rules]] constitute an accurate tool to exclude fractures within the first week after an ankle injury.<ref name="kngf0" /><br> | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
| Line 79: | Line 79: | ||
=== Step 1: Inflammatory Phase (0-3 days) === | === Step 1: Inflammatory Phase (0-3 days) === | ||
Reduction of pain and swelling and improve circulation and partial foot support<br>Actions <br>The most common approach to manage ankle sprain consists of rest, ice, compression, and elevation (RICE | Reduction of pain and swelling and improve circulation and partial foot support<br>Actions <br>The most common approach to manage ankle sprain consists of rest, ice, compression, and elevation (RICE)<br>1. Recommendations for the patient:<br>o REST: advise to rest for the first 24 hours after injury, possibly with crutches to offload the injured ankle and altering work and sport/exercise requirements as needed<br>o ICE: Apply a cold application (15 to 20 minutes, one to three times per day) <br>o Apply a compression bandageto control the swelling caused by the ankle sprain <br>o ELEVATION: ideally elevate the ankle above the level of the heart but minimally avoid positions where the ankle is in a dependent position relative to the body <br>2. Practice foot and ankle functions:<br>Ask your patient to move toes and anke within pain-free limits to improve the local circulation. <ref name="Allen" /><ref name="Chris M Bleakley1">Bleakley CM, O'Connor S, Tully MA, Rocke LG, MacAuley DC, McDonough S. The PRICE study (Protection Rest Ice Compression Elevation): design of a randomised controlled trial comparing standard versus cryokinetic ice applications in the management of acute ankle sprain. BMC Musculoskelet Disord. 2007; 8:125. Available from: http://www.biomedcentral.com/content/pdf/1471-2474-8-125.pdf (accessed 29 Aug 2012) </ref><ref name="The Use of Ice">Bleakley C, McDonough S, MacAuley D. The use of ice in the treatment of acute soft-tissue injury. A systematic review of randomized controlled trials. Am J Sports Med. 2004;32(1):251-61. Available from: http://www.smawa.asn.au/_uploads/res/120_3630.pdf (accessed 29 Aug 2012) </ref><br> | ||
=== Step 2: Proliferative Phase (4-10 days) === | === Step 2: Proliferative Phase (4-10 days) === | ||
<br>Recovery of foot and ankle | <br>Goals: Recovery of foot and ankle function and improved load-carrying capacity. <br>Actions: <br>1. Patient eduation regarding gradual increase in activity level, guided by symptoms. <br> | ||
2. Practise foot and ankle functions | 2. Practise foot and ankle functions - range of motion, [[Active stability|active stability]], [[Motor coordination|motor coordination]] | ||
Still it remains uncertain | 3. [[Tape|Tape]]/[[Brace|Brace]] :<br>Apply tape as soon as the swelling is decreased. Whether you use a tape or a brace depends on the preferences of the patient. Boyce et al (2005) found that the use of an Aircast ankle brace for the treatment of lateral ligament ankle sprains produces a significant improvement in ankle joint function compared with standard management with an elastic support bandage.<ref name="S H Boyce"> Boyce SH, Quigley MA, Campbell S. Management of ankle sprains: a randomised controlled trial of the treatment of inversion injuries using an elastic support bandage or an Aircast ankle brace. Br J Sports Med. 2005;39(2):91-6. Available from: http://bjsm.bmj.com/content/39/2/91.full.pdf+html (accessed 29 Aug 2012)</ref> | ||
Still it remains uncertain which treatment (brace, bandage, tape) is most beneficial. <ref name="kngf0" /><br> | |||
=== Step 3: Early Remodelling (11 -21 days) === | === Step 3: Early Remodelling (11 -21 days) === | ||
<u></u> Improve [[Muscle strength of the ankle|muscle strength]], active (functional) stability, foot/ankle motion, mobility (walking, walking stairs, running)<br>Actions <br>1. | Goals:<u></u> Improve [[Muscle strength of the ankle|muscle strength]], active (functional) stability, foot/ankle motion, mobility (walking, walking stairs, running).<br>Actions: <br>1. Education:<br> | ||
*Provide information about possible preventive measures (tape or brace) | *Provide information about possible preventive measures (tape or brace) | ||
*Advise to wear | *Advise regarding appropriate shoes to wear during sport activities - judge the quality of the shoes in relation to the type of sport and surface | ||
2. Practise foot and ankle functions | 2. Practise foot and ankle functions <br> | ||
*Practice balance, muscle strength, ankle/foot motion and mobility (walking, | *Practice balance, muscle strength, ankle/foot motion and mobility (walking, stairs, running). Look for a [[Walk pattern|symmetric walk pattern]]. | ||
*Work on dynamic stability | *Work on dynamic stability as soon as the load-bearing capacity allows, focusing on balance and coordination exercises. Gradually progress the loading, from statical to dynamic exercises, from partially loaded to fully loaded exercises and from simple to functional multi-tasking exercises. Alternate cycled with non-cycled exercises (abrupt, irregular exercises). Use different types of surfaces to increase the level of difficulty. <br> | ||
*Encourage the patient to continue practicing the | *Encourage the patient to continue practicing the functional activities at home with precise instructions regarding the expectations for each exercise. | ||
3. Bandage | 3. Bandage | ||
| Line 108: | Line 110: | ||
=== Step 4: Late Remodelling and Maturation <br> === | === Step 4: Late Remodelling and Maturation <br> === | ||
<br>Improve the regional load-carrying capacity, walking skills and improve the skills needed during activities of daily living | <br>Goals: Improve the regional load-carrying capacity, walking skills and improve the skills needed during activities of daily living as well as work and sports.<br>Actions: <br>1. Practise and adjust foot abilities (functions and activities)<br> | ||
*Practise motor coordination skills while practising [[Mobility exercises of the ankle|mobility exercises]] | *Practise motor coordination skills while practising [[Mobility exercises of the ankle|mobility exercises]] | ||
* | *Continue to progress the load-bearing capacity as described above until the pre-injury load-carrying capacity is reached | ||
*Increase the compexity of motor coordination exercises in varied situations until the pre-injury level is reached | |||
*Increase the | *Encourage the patient to continue practicing at home<br> | ||
*Encourage the patient to continue practicing at home | |||
== Key Research == | == Key Research == | ||
Revision as of 19:25, 31 August 2012
Original Editor - Dale Boren, Michael Kauffmann, Pieter Jacobs
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Definition/Description[edit | edit source]
An ankle sprain is where one or more of the ligaments of the ankle are partially or completely torn.
Clinically Relevant Anatomy[edit | edit source]
An ankle sprain is a common injury in which one or more of the ankle ligaments is torn or partially torn. Inversion ankle sprains are the most common, making up 85% of all ankle sprains. The most commonly torn ankle ligament is the anterior talofibular ligament (ATFL) which is on the lateral aspect of the ankle.
| [1] |
Epidemiology /Etiology[edit | edit source]
The most common mechanism of injury for an ankle sprain involving the lateral aspect of the ankle (commonly called a lateral or inversion ankle sprain) is when the foot is forced into a combined movement of plantarflexion and inversion. In this situation the ankle would roll into an outward direction with the foot and toes moving inward toward the midline of the body.
A less common mechanism of injury involves a forceful eversion movement at the ankle, resulting in injury to the strong deltoid ligament complex.
File:Inversion of ankle.jpg Ankle Inversion |
File:Eversion of ankle.jpg Ankle Eversion |
| [2] | [3] |
Characteristics/Clinical Presentation[edit | edit source]
add text here relating to the clinical presentation of the condition
Differential Diagnosis
[edit | edit source]
The Ottawa ankle rules constitute an accurate tool to exclude fractures within the first week after an ankle injury.[4]
Diagnostic Procedures[edit | edit source]
add text here related to medical diagnostic procedures
Outcome Measures[edit | edit source]
add links to outcome measures here (also see Outcome Measures Database)
Lower Extremity Functional Scale (LEFS) - www.manualphysicaltherapy.net/Downloads/Lower_Extremity.doc
Examination[edit | edit source]
add text here related to physical examination and assessment
Medical Management
[edit | edit source]
add text here
Physical Therapy Management[edit | edit source]
CASE1: Mild ankle sprain (natural full recovery within 14 days)
Taping and making an appointment for a check-up to evaluate the healing of the ankle sprain[4][5]
CASE2: Severe ankle sprain
In this case physiotherapy is required. Functional therapy of the ankle is shown to be more efficient than immobilisation. Functional therapy treatment will be divided in four steps, related to the four steps in the tissue recovery after an acute ankle sprain, [4] Inflammatory phase, Proliferative phase, Early Remodelling, Late Maturation and Remodelling. [4][5][6][7][8]
Step 1: Inflammatory Phase (0-3 days)[edit | edit source]
Reduction of pain and swelling and improve circulation and partial foot support
Actions
The most common approach to manage ankle sprain consists of rest, ice, compression, and elevation (RICE)
1. Recommendations for the patient:
o REST: advise to rest for the first 24 hours after injury, possibly with crutches to offload the injured ankle and altering work and sport/exercise requirements as needed
o ICE: Apply a cold application (15 to 20 minutes, one to three times per day)
o Apply a compression bandageto control the swelling caused by the ankle sprain
o ELEVATION: ideally elevate the ankle above the level of the heart but minimally avoid positions where the ankle is in a dependent position relative to the body
2. Practice foot and ankle functions:
Ask your patient to move toes and anke within pain-free limits to improve the local circulation. [5][9][10]
Step 2: Proliferative Phase (4-10 days)[edit | edit source]
Goals: Recovery of foot and ankle function and improved load-carrying capacity.
Actions:
1. Patient eduation regarding gradual increase in activity level, guided by symptoms.
2. Practise foot and ankle functions - range of motion, active stability, motor coordination
3. Tape/Brace :
Apply tape as soon as the swelling is decreased. Whether you use a tape or a brace depends on the preferences of the patient. Boyce et al (2005) found that the use of an Aircast ankle brace for the treatment of lateral ligament ankle sprains produces a significant improvement in ankle joint function compared with standard management with an elastic support bandage.[11]
Still it remains uncertain which treatment (brace, bandage, tape) is most beneficial. [4]
Step 3: Early Remodelling (11 -21 days)[edit | edit source]
Goals: Improve muscle strength, active (functional) stability, foot/ankle motion, mobility (walking, walking stairs, running).
Actions:
1. Education:
- Provide information about possible preventive measures (tape or brace)
- Advise regarding appropriate shoes to wear during sport activities - judge the quality of the shoes in relation to the type of sport and surface
2. Practise foot and ankle functions
- Practice balance, muscle strength, ankle/foot motion and mobility (walking, stairs, running). Look for a symmetric walk pattern.
- Work on dynamic stability as soon as the load-bearing capacity allows, focusing on balance and coordination exercises. Gradually progress the loading, from statical to dynamic exercises, from partially loaded to fully loaded exercises and from simple to functional multi-tasking exercises. Alternate cycled with non-cycled exercises (abrupt, irregular exercises). Use different types of surfaces to increase the level of difficulty.
- Encourage the patient to continue practicing the functional activities at home with precise instructions regarding the expectations for each exercise.
3. Bandage
- Advise to wear tape or brace during physical activities. These procedures are needed until the patient is able to execute correctly the static and dynamic exercises of balance and motor coordination.
Step 4: Late Remodelling and Maturation
[edit | edit source]
Goals: Improve the regional load-carrying capacity, walking skills and improve the skills needed during activities of daily living as well as work and sports.
Actions:
1. Practise and adjust foot abilities (functions and activities)
- Practise motor coordination skills while practising mobility exercises
- Continue to progress the load-bearing capacity as described above until the pre-injury load-carrying capacity is reached
- Increase the compexity of motor coordination exercises in varied situations until the pre-injury level is reached
- Encourage the patient to continue practicing at home
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
J Whitman, et al. Predicting short term response to thrust and non-thrust manipulation and exercise in patients post inversion ankle sprain. J Orthop Phys Ther, 2009; 39(3):188-200.
Resources
[edit | edit source]
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=10AkQ1Iw49RNj1Cqs_4wNakMkqbX7LuY-6-rVEFqFMH3xQJMDP|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
- ↑ Dr Glass DPM. Ankle Sprain Injury Explained. Available from: http://www.youtube.com/watch?v=_u5w856Yjvg [last accessed 28/08/12]
- ↑ MsBlackbetty92. Inversion Ankle Sprains. Available from: http://www.youtube.com/watch?v=T5qCI0T4Fhs [last accessed 28/08/12]
- ↑ MrAdyBoy. Unbelievable Tennis Accident. Available from: http://www.youtube.com/watch?v=o9-U_Iv0O78 [last accessed 28/08/12]
- ↑ 4.0 4.1 4.2 4.3 4.4 Van der Wees PJ, Lenssen AF, Feijts YAEJ, Bloo H, van Moorsel SR, Ouderland R, et al. KNGF-Guideline for Physical Therapy in patients with acute ankle sprain. Dutch J Phys Ther. 2006; 116(Suppl 5):**. Available from: https://www.kngfrichtlijnen.nl/images/imagemanager/guidelines_in_english/KNGF_Guideline_for_Physical_Therapy_in_patients_with_Acute_Ankle_Sprain.pdf (accessed 29 Aug 2012).
- ↑ 5.0 5.1 5.2 Fongemie A, Dudero A, Standemo G, Stovitz S, Dahm D, THomas A, et al. Health Care Guideline [Internet]. Institute for Clinical Systems Improvement. Health care guideline: ankle sprain. 7th ed. 2006. Available from: http://www.icsi.org/ankle_sprain/ankle_sprain_4.html (accessed 29 Aug 2012)
- ↑ Van der Wees PJ, Lenssen AF, Hendriks EJM, Stomp DJ, Dekker J, de Brie RA. Effectiveness of exercise therapy and manual mobilisation in acute ankle sprain and functional instability: a systematic review. Aust J Physiother. 2006; 52:27-37. Available from: http://svc019.wic048p.server-web.com/ajp/vol_52/1/AustJPhysiotherv52i1van_der_Wees.pdf (accessed 29 Aug 2012)
- ↑ Bleakley CM, O’Connor SR, Tully MA, Rocke LG, MacAuley DC, Bradbury I et al. Effect of accelerated rehabilitation on function after ankle sprain: randomised controlled trial. BMJ. 2010; 340:c1964. Available from: http://www.bmj.com/content/340/bmj.c1964.pdf%2Bhtml(accessed 29 Aug 2012)
- ↑ Kerkhoffs GM, Rowe BH, Assendelft WJ, Kelly KD, Struijs PA, van Dijk CN. Immobilisation for acute ankle sprain. A systematic review.. Arch Orthop Trauma Surg. 2001;121(8):462-71. Available from: http://www.springerlink.com/content/knrf19kk4tvc2668/
- ↑ Bleakley CM, O'Connor S, Tully MA, Rocke LG, MacAuley DC, McDonough S. The PRICE study (Protection Rest Ice Compression Elevation): design of a randomised controlled trial comparing standard versus cryokinetic ice applications in the management of acute ankle sprain. BMC Musculoskelet Disord. 2007; 8:125. Available from: http://www.biomedcentral.com/content/pdf/1471-2474-8-125.pdf (accessed 29 Aug 2012)
- ↑ Bleakley C, McDonough S, MacAuley D. The use of ice in the treatment of acute soft-tissue injury. A systematic review of randomized controlled trials. Am J Sports Med. 2004;32(1):251-61. Available from: http://www.smawa.asn.au/_uploads/res/120_3630.pdf (accessed 29 Aug 2012)
- ↑ Boyce SH, Quigley MA, Campbell S. Management of ankle sprains: a randomised controlled trial of the treatment of inversion injuries using an elastic support bandage or an Aircast ankle brace. Br J Sports Med. 2005;39(2):91-6. Available from: http://bjsm.bmj.com/content/39/2/91.full.pdf+html (accessed 29 Aug 2012)