Ankle and Foot Arthropathies
Original Editors - <a href="User:Ward Willaert">Ward Willaert</a>
Top Contributors - <img class="FCK__MWTemplate" src="http://www.physio-pedia.com/extensions/FCKeditor/fckeditor/editor/images/spacer.gif" _fckfakelement="true" _fckrealelement="10" _fck_mw_template="true">
Search Strategy[edit | edit source]
Search terms: “Arthropathy”, “Haemophilic arthropathy”, “Osteoarthritis”, Rheumatoid arthritis”, Gout”, “psoriatic arthritis”, reactive arthritis”, Diabetic foot arthritis”, “Charcot neuropathic osteoarthropathy”
All these terms combined with: … AND “Diagnosis”, … AND “Epidemiology”, … AND “Treatment”, … AND “medical management”, … AND “Physical management”.
Used databases: PubMed, Google Scholar, Web of Science, Pedro, VUB library
Definition/Description [edit | edit source]
Arthropathy
An arthropathy is a disease that effects a joint. So, in this case, “ankle and foot arthropathies” are diseases of the joints in the ankle and/or foot.
Although the terms "arthropathy" and arthritis have very similar meanings, the former is traditionally used to describe the following conditions:
• Reactive arthropathy occurs as a reaction against an infection site elsewhere in the body. (1).
• Enteropathic arthropathy is an arthropathy in association with, or as a reaction to, an enteric (usually colonic) inflammatory condition. (2)
• Crystal arthropathy is characterized by accumulation of tiny crystals in one or more joints.(3)
• Neuropathic arthropathy is a joint disease caused by diminished proprioceptive sensation, with gradual destruction of the joint by repeated subliminal injury. (4)
• Diabetic arthropathy is a neuropathic arthropathy occurring in diabetes. (5)
An arthropathy can be degenerative, such as osteoarthritis, or it can be associated with an inflammation, for example rheumatoid arthritis. A joint disease can also occur after a trauma.
Although an arthropathy is distinctly less common in the ankle than in the hip and knee, it is an equally disabling condition. (6)
Because arthropathy of the ankle and foot is such a wide subject, it is difficult to explain it in general. We decided to discuss some arthropaties separately: osteoarthritis, rheumatoid arthritis, haemophilic arthropathy, diabetic foot arthropathy, gout, psoriatic arthritis and reactive arthritis.
Osteoarthritis Osteoarthritic diseases are a result of both mechanical and biological events that destabilize the normal coupling of degradation and synthesis of articular cartilage chondrocytes, extracellular matrix and subchondral bone. Although they may be initiated by multiple factors, including genetic, developmental, metabolic, and traumatic, OA diseases involve all the tissues of the diathrodial joint.
Ultimately, OA diseases are manifested by morphologic, biochemical, molecular and biomechanical changes of both cells and matrix which lead to a softening, fibrillation, ulceration, loss of articular cartilage, sclerosis and eburnation of subchondral bone, osteophytes, and subchondral cysts. (7)
Rheumatoid arthritis
According to previous studies, rheumatoid foot problems can be roughly categorized into forefoot, midfoot and hindfoot pathologies.(8) Most of the studies have focused on forefoot and hindfoot pathologies are less studies are conducted concentrating on the midfoot RA. (9) Rheumatoid arthritis is a multisystemic chronic progressive inflammatory disease. The joints become swollen, tenderness and painful. This can lead to severe disability.(9)(10)(11)(12)(13)
Haemophilic arthropathy
Haemophilic arthropathy is an important cause of morbidity in patients with severe haemophilia. The degenerative changes that occur in the joints of these patients are usually progressive and result from recurrent bleeding in ‘target’ joints. The ankle is one of the most frequent sources of pain in haemophilic patients. (14)
Diabetic foot arthropathy
Charcot neuropathic osteoarthropathy of the foot is a devastating neuropathic complication of diabetes. (15)(16)(17)(18)(19)(20)
Charcot foot is a progressive and degenerative arthropathy of single or multiple joints that ultimately leads to destruction of normal foot architecture, collapse of the arch. (17) It also frequently leads to foot ulceration, gangrene and foot amputation. (18)(19)(20)
The current accepted origin theory of Charcot neuropathic osteoarthropathy states that an unregulated inflammatory process is triggered in patients with peripheral neuropathy. The inflammatory process eventually stimulates the maturation of osteoclasts from osteoclast precursor cells. (18)(20)
Gout
Gout is a crystal-induced arthritis, in which monosodium urate (MSU) crystals precipitate within joints and soft tissues and elicit a highly inflammatory but localized response. The susceptibility to form MSU crystals is a consequence of excessive blood levels of soluble urate, one of the final products of the metabolic breakdown of purine nucleotides. Hyperuricemia is typically defined as occurring above the saturation point of MSU, at which point the risk of crystallization increases. Using this definition, hyperuricemia occurs at serum urate levels >6.8 mg/dL (21).
Psoriatic arthritis
Psoriatic arthritis is an inflammatory arthritis which affects the skin and musculoskeletal system. (22)(23) If not diagnosed early and treated effectively it can result in joint deformity and disability. (22)
Psoriatic arthritis is a chronic condition which can cause considerable disability and pain if not recognized and treated properly. Approximately 15% of patients affected by psoriasis will develop associated joint disease. It was first recognized in 1964 and is now considered part of the spondyloarthropathy group of diseases. (22)
Reactive arthritis
Reactive arthritis (ReA) is an infectious disease which may be initiated by several microbes in genetically susceptible hosts. (24) Reactive arthritis is one of the types known to primarily affect young men. Because it can be a complication of sexually transmitted infections.
ReA is classified as a type of spondyloarthritis. This group of joint diseases features mono- or oligoarthritis, often associated with extra-articular inflammatory manifestations involving the musculoskeletal, ophthalmologic, dermatologic, and genitourinary systems. These were previously referred to as seronegative spondyloarthritides because the rheumatoid factor is usually negative. (25)
Clinically Relevant Anatomy[edit | edit source]
We will discuss the most relevant anatomy for ankle and foot arthropathies: bones, joints and nerves.
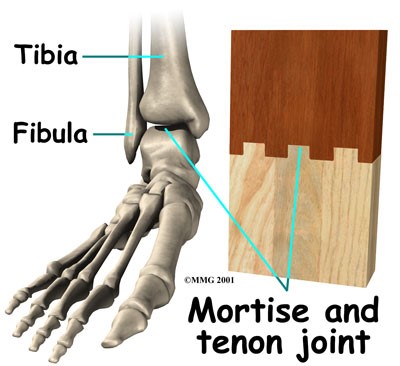
Bones and joints
The two bones of the lower leg, the tibia and the fibula, come together and form the ankle joint together with the talus. They form a very stable structure, known as a mortise and tenon joint. The ankle joint allows the foot to bend up, flexion, and down, extension. (26)(27)
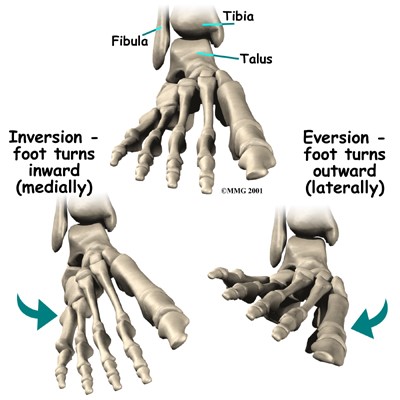
The two bones that make up the back part of the foot, sometimes referred to as the hindfoot, are the talus and the calcaneus. The talus is connected to the calcaneus at the subtalar joint. The subtalar joint allows the foot to rock from side to side. When the foot turns inward, it’s called inversion and when the foot turns outward, it’s called eversion. (26)(27)
Just down the foot from the ankle is a set of five bones called tarsal bones that work together as a group. They exist of 3 cuneiform bones (lateral, intermediate and medial), the navicular bone and the cuboid bone. These bones are unique in the way they fit together. When the foot is twisted in one direction by the muscles of the foot and leg, these bones lock together and form a very rigid structure. When they are twisted in the opposite direction, they become unlocked and allow the foot to conform to whatever surface the foot is contacting. The connection between these tarsal bones and the upper bones is called Chopart’s joint line. (26)(27)
File:Anatomy ankle and foot 3.jpg
The tarsal bones are connected to the five long bones of the foot, called the metatarsals. The two groups of bones are rigidly connected, without much movement at the joints. Finally, there are the bones of the toes, the phalanges. The joints between the metatarsals and the first phalanx are called the metatarsophalangeal joints (MTP). These joints form the ball of the foot, and movement in these joints is very important for a normal walking pattern. Not much motion occurs at the joints between the bones of the toe, the interphalangeal joints. The big toe, or hallux, is the most important toe for walking, and the first MTP joint is a common area for problems in the foot. (26)(27)
Nerves
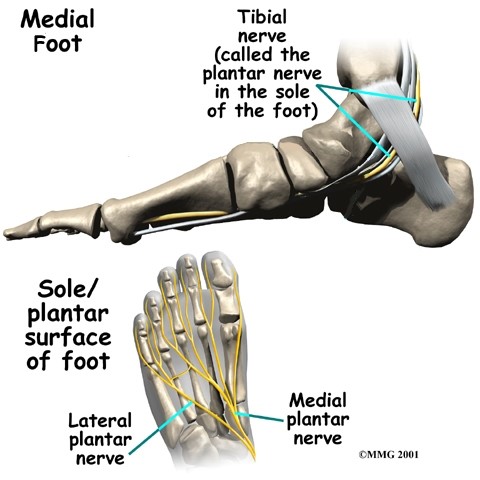
The main nerve to the foot, the tibial nerve, enters the sole of the foot by running behind the inside bump on the ankle, the medial malleolus. It divides into its terminal branches, the medial and lateral plantar nerves. (26)(27)
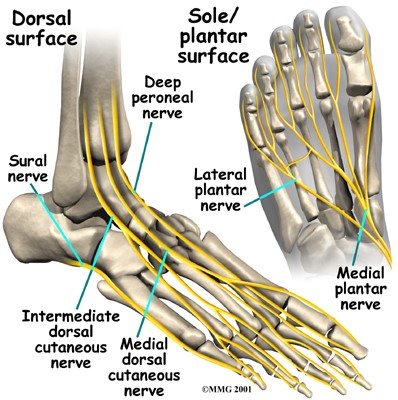
At the dorsal surface of the foot lies the peroneal nerve, divided into the deep peroneal nerve and the superficial peroneal nerve, the sural nerve and the saphenous nerve, divided into the intermediate and medial dorsal cutaneous nerve. (28)
The tibial nerve, divided into medial plantar nerve (MPN) and lateral plantar nerve (LPN) supplies sensation to the toes and sole of the foot and controls the muscles of the sole of the foot. (26)(27)(28)
The deep peroneal nerve (DPN) provides motor innervation to the muscles of the anterior compartment and sensation to the big and second toe. The superficial peroneal nerve (SPN) reaches the dorsum of the foot and supplies the dorsal aspect of the toes, with the exception of the first web space. The sural nerve (SU) provides sensory innervation to the lateral aspect of the foot and fifth toe. The saphenous nerve (SA) to the medial aspect of the foot up to the first metatarsophalangeal joint. (28)
More information about the anatomy of the ankle and foot can be found on the physiopedia page “Biomechanics of Foot and Ankle” and “Ankle Joint”.
Epidemiology /Etiology[edit | edit source]
add text here
Characteristics/Clinical Presentation[edit | edit source]
The characteristics and clinical presentation of ankle arthropathies such as different forms of arthritis can be described as followed:
- Ankle pain
- stiffness
- swelling
- limited range of motion (ROM)
- Pain Mostly gets worse by activities such as standing, walking or running.
We can also speak of the so called “Start-up pain” such as when a patient has pain and stiffness in the ankle after sleeping or sitting in one spot for a while is also a common complaint.
When this happens/occurs it often takes the patient a few minutes (or longer) to “warm-up” the ankle. The ankle will tend to swell more as the day progresses particularly if there is increasing activity( patient is still doing sport activities, work activities,…).
Most of the time Pain is experienced throughout the ankle although it may be more noticeable in the front of the ankle if large bones spurs have formed. When there has been damage to the joint ankle, it’s often seen that arthritis will occur. Cartilage that normally covers the bones of the ankle joint can be lost leading to an ankle arthropathy.
Differential Diagnosis[edit | edit source]
Intra-articular pathologic lesions must be distinguished from surrounding joint tendinitis and bursitis. This can be achieved with diagnostic testing such as magnetic resonance imaging or with injection of local anesthetic.
Primary osteoarthritis is a diagnosis of exclusion. It has been addressed successfully with low tibial osteotomy[1]
Post traumatic osteoarthritis is the most common form of ankle arthritis. Post-traumatic disease can be present after intra-articular fractures or improper joint biomechanics after extra-articular fractures. Frequently, deformity is present in the joint. The extent of bone loss after trauma and joint space collapse can be assessed with weightbearing radiographs and CT scans.
Avascular necrosis must be considered in cases in which sclerosis of the talar dome is present. Patients may have a history of talar neck fracture, steroid or alcohol usage, or nonspecific injuries. Avascular necrosis of the talus can result in progressive segmental collapse and an increasing amount of particulate matter into the joint.
Systematic inflammatory diseases such as rheumatoid arthritis should be excluded prior to considering operative intervention. Ankle arthritis can be effectively treated with a medical regimen prior to considering surgical intervention, particularly during a flare of the disease. The majority of patients with rheumatoid arthritis test positive for rheumatoid factor. In addition, the diagnosis of rheumatoid arthritis requires the presence of certain other symptoms: morning stiffness, multiple joint swelling, rheumatoid nodules, and joint erosion on radiographs[2]
Patients with absence of rheumatoid factor in the serum, but manifestations of inflammatory arthritis are classified as having seronegative arthropathy. The four major disorders include ankylosis spondylitis, psoriatic arthritis, Reiter’s syndrome, and inflammatory bowel arthritides.
Metabolic and infectious causes of arthritis must be considered as well. This can include gonococcal disease, Lyme disease, and gouty uricemia. Patients should be questioned about possible exposure to disease sources for sexually transmitted diseases and insect bites.
H(a)emophilic arthropathy occurs by people who have haemophily, this is a desease which unables the blood from bleeding. When these bleedings occur within the joint it causes multiple defects to the joint, this is the result of a number of mechanisms affecting the synovial lining which becomes progressively fibrotic and the hyaline cartilage which disintegrates and is eventually lost. Mechanical and chemical processes cause degeneration of cells but enzymatic processes appear to be primairily responsible for the degradation of the matrix of the articular cartilage.[3]
Charcot osteoarthropathy or pedal neuropathic joint disease is a condition associated with peripheral neuropathy , it is a progressive deterioration of weight-bearing joints, usually in the foot or ankle, and is characterised in its early stages by acute inflammation that leads to bone and joint fracture, dislocation, instability and Gross deformaties. in patients with diabetes, Charcot osteoarthropathy is associated with a longstanding duration of diabetes and peripheral neuropathy. In the early stages of Charcot osteoarthropathy, the patient presents with a warm, erythematous and oedematous foot with or without associated pain or reported previous injury and can clinically mimic cellulitis or gout.[4]. It can lead to gross structural deformities of the foot and ankle, and subsequent skin ulceration and lower limb amputation from soft tissue or bony infection. The Charcot foot occurs most often in patients with diabetic neuropathy; other predisposing conditions include alcoholic neuropathy, sensory loss caused by cerebral palsy or leprosy, and congenital insensitivity to pain. However, it is often unrecognised, with deleterious consequences..[5][6]
Diagnostic Procedures[edit | edit source]
Osteoarthritis
The diagnosis of osteoarthritic ankle joint starts with clinical assessment, and includes assessment of alignment and stability and measurement of range of motion. Different radiographic modalities may help to recognize and analyse the underlying reasons for ankle OA. Only weight-bearing radiographs of the foot and ankle should be performed. Additional imaging modalities such as MRI and SPECT-CT may help to evaluate the extent of degenerative changes and their biological activities. (29)
Rheumatoid arthritis
Different imaging techniques, e.g. MRI, CT and ultrasonography (US), should help clinicians to detect early or subclinical foot problems, because clinical signs of foot disease in RA are often subtle. (9)(53)
When detecting joint inflammation ultrasonography and MRI have shown to be superior the clinical examination. (54) Sonography is being used more and more and has been found effective for the detection of erosions in patients with RA. Ultrasonography detected 6.5-fold more erosions in early disease than radiography. (53) Because US is easily available and less expensive than MRI it can be recommended as the first imaging method after plain radiography. (54)
Haemophilic arthropathy
Radiography remains the workforce horse in the diagnosis and follow-up of haemophilic arthropathy. The radiographical findings in arthropathy follow an expected sequence of events and are overall similar in different joints. Magnetic resonance imaging (MRI) has advantages over radiography based on its capability of visualizing soft tissue and cartilage changes in haemophilic joints. The recent development and standardization of MRI scoring systems for measuring soft tissue and cartilage abnormalities may enable the comparison of pathological joint findings in clinical trials conducted at different institutions across the world (55)
Diabetic foot arthropathy
The diagnosis is based on patient’s history, clinical examination, and imaging methods. As a result of their lowered perception of pain, patients are quite often not aware of any injury. (20)(31) Local inflammation is the main symptom which can lead to the diagnosis being suspected. (18)
In Charcot feet arthropathies it is very important that the disease is diagnosed quickly, because a delay can lead to worsening structural damage or even limb loss. (16)(56)(57)(58) Unfortunately the diagnosis is often missed at first presentation. A possible reason for the missed diagnosis is that Charcot feet are not emphasized in medical training. The result is that it is difficult to advocate the right choice of approach due to low evidence based information. (16)
Acute Charcot activity can be diagnosed if the temperature of the affected foot is 2°C or more than the contralateral unaffected foot. (58)(20)
Gout
Gout is ideally diagnosed through identification of characteristic negatively birefringent crystals under polarized light microscopy in fluid aspirated from end-organ deposits, typically from a joint (59). However, fewer than 10% of patients with gout see a rheumatologist, and most cases of gout are diagnosed in the primary care setting based on signs, symptoms, and serum uric acid level (60).
Psoriatic arthritis
A diagnostic test for psoriatic arthritis does not exist unlike in RA which is cyclic citrullinated peptide and rheumatoid factor positive. As in other inflammatory conditions, markers such as erythrocyte sedimentation rate and C-reactive protein can be raised in psoriatic arthritis. (22)
Scoring systems have been developed to try and identify psoriatic arthritis at an early stage and criteria have been developed to aid in classification of the disease from the other SPAs and inflammatory arthritides. Not only are they useful for identifying psoriatic arthritis earlier, they can also help identify cases of psoriatic arthritis which do not present in the typical manner. Some criteria include psoriatic arthritis with the SPA group. The classification for psoriatic arthritis (CASPAR) criteria was developed specifically for psoriatic arthritis. It has good sensitivity and specificity for those presenting with disease of <2 years’ duration. Although primarily used for classification, it can be used for diagnostic purposes. (22)
Further imaging such as magnetic resonance imaging (MRI) can help to identify soft tissue involvement in further detail, particularly when a patient is suffering from enthesitis. Ultrasound has also become a useful tool in the investigation of arthritis; it can help to identify bony erosions in those patients where synovitis or dactylitis is not always evident clinically. Studies have shown that ultrasound scan and MRI are more sensitive for detecting inflammation than plain radiographs
in psoriatic arthritis. (22)
Outcome Measures[edit | edit source]
(also see <a href="Outcome Measures">Outcome Measures Database</a>)
Osteoarthritis
The Ankle Osteoarthritis Scale (two subscales: pain and disability) (103) is a reliable and valid self-assessment instrument that specifically measures patient symptoms and disabilities related to ankle arthritis. (109)
More outcome measures of ankle osteoarthritis can be found on the physiopedia page “<a href="http://www.physio-pedia.com/Ankle_Osteoarthritis#Outcome_Measures">Ankle Osteoarthritis Arthritis</a>”
Rheumatoid arthritis
American College of Rheumatology (ACR) response criteria for RA. (104)
The ACR20 response criteria require a 20% improvement in both tender and swollen joint counts, and a 20% improvement in 3 of 5 items: patient global assessment (visual analog scale, VAS), physician global assessment (VAS), patient pain score (VAS), Health Assessment Questionnaire (HAQ), and either erythrocyte sedimentation rate or C-reactive protein (CRP). For some PsAstudies the joint count was increased to 78 to include distal interphalangeal (DIP) joints of the feet. To achieve an ACR50 or ACR70 response, the same guidelines apply but the level of response is 50% or 70% improvement, respectively. (104)
Haemophilic arthropathy
Visualization of bone or cartilage damage in index joints on MRI can be used as outcome measure
Tentative haemophilic arthropathy scales based on MRI findings have been developed in the last decade. In 2005, the International Prophylaxis Study Group (IPSG) presented a preliminary comprehensive scoring scheme that combined the pioneer Denver and European MRI scores. The use of such scales should result in a more consistent assessment of haemophilic joints and should facilitate the development of more targeted treatment to prevent or delay further destructive osteoarticular changes. (105)
Diabetic foot arthropathy
No research found.
Gout
Many different instruments can be used to assess the acute gout core domains. Pain VAS and 5-point Likert scales, 4-point Likert scales of index joint swelling and tenderness and 5-point PGART instruments meet the criteria for the OMERACT filter. (106)
Psoriatic arthritis
The Psoriatic Arthritis Response Criteria (PsARC) is recommended in the assessment and monitoring of PsA. It consists of four components: assessment of joint tenderness and swelling utilizing 68/66 joint counts respectively, the patient’s opinion of their global health and the physician’s global assessment. (104)(107)
Reactive arthritis
The outcome measures of reactive arthritis can be found on the physiopedia page “<a href="http://www.physio-pedia.com/Reactive_Arthritis#Outcome_Measures">Reactive Arthritis</a>”
Examination[edit | edit source]
Osteoarthritis
The examination of osteoarthritis can be found on the physiopedia page “<a href="http://www.physio-pedia.com/Ankle_Osteoarthritis">Ankle Osteoarthritis</a>”
Rheumatoid arthritis
The examination of rheumatoid arthritis can be found on the Physiopedia page “<a href="http://www.physio-pedia.com/Rheumatoid_Arthritis">Rheumatoid Arthritis</a>”
Medical Management
[edit | edit source]
Osteoarthritis
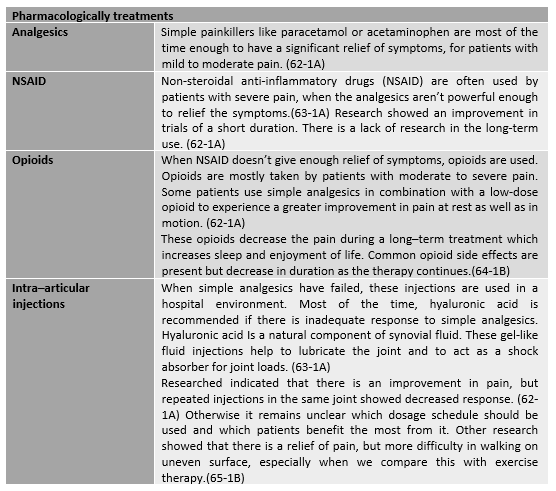
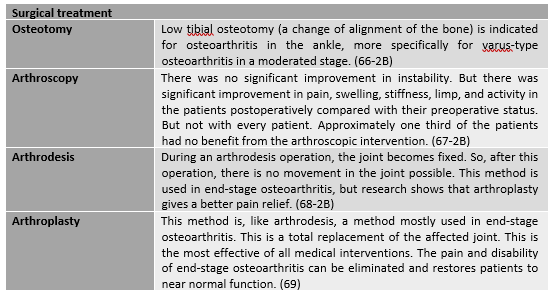
There is no cure of osteoarthritis. There are several treatments we can subdivide in pharmacologically, non- pharmacologically and surgical. The choice of treatment of ankle and foot osteoarthritis(OA) depends on the severity of the disease. (61) The goal of managing OA in foot and ankle includes the control of pain, improvement in function and quality of life. A number of different aspects like discomfort, comorbidity and radiologic damage need to be considered. (62-1A)
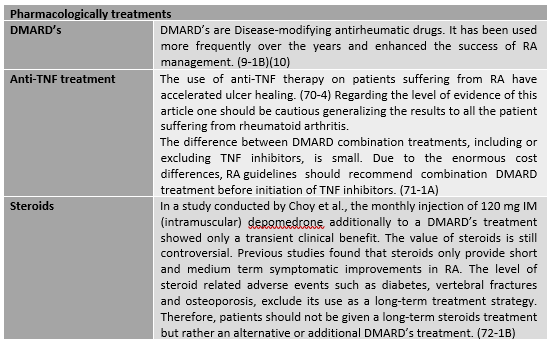
Rheumatoid arthritis
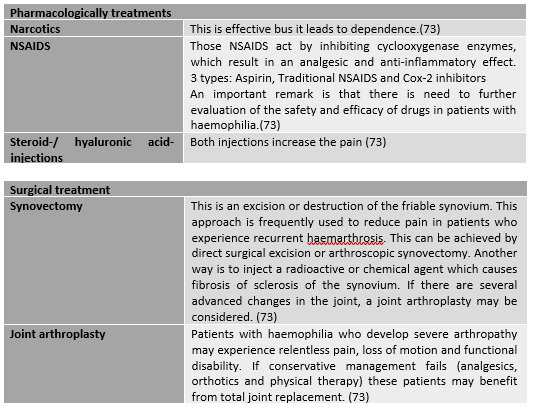
Haemophilic arthropathy
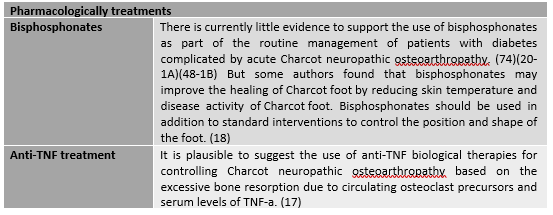
Diabetic foot arthropathy
A multidisciplinary approach is recommended for the management of Charcot foot involving medical and allied health professionals. (19)
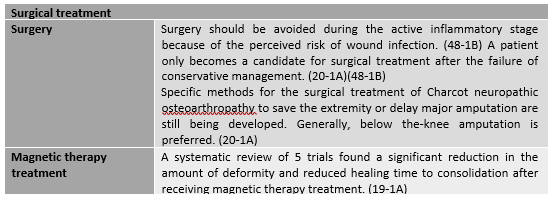
Gout
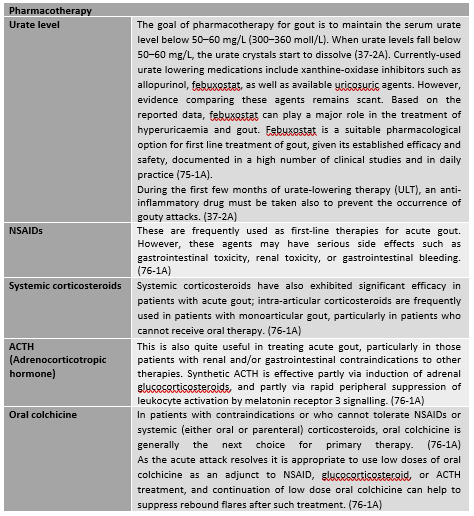
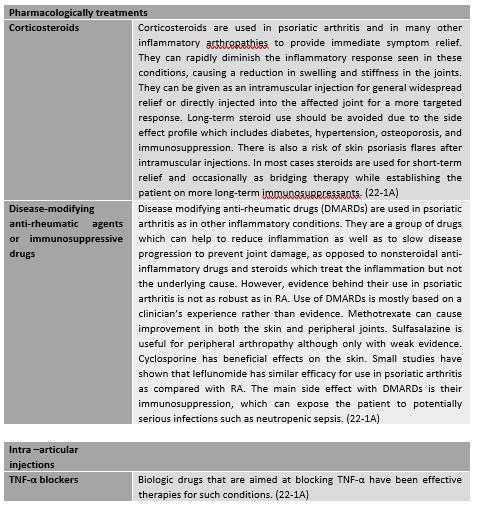
Psoriatic arthritis
Treatments such as oral disease modifying anti-rheumatic drugs and biologic therapy are effective but have side effects which could limit their use in certain individuals. (22-1A)
Reactive arthritis
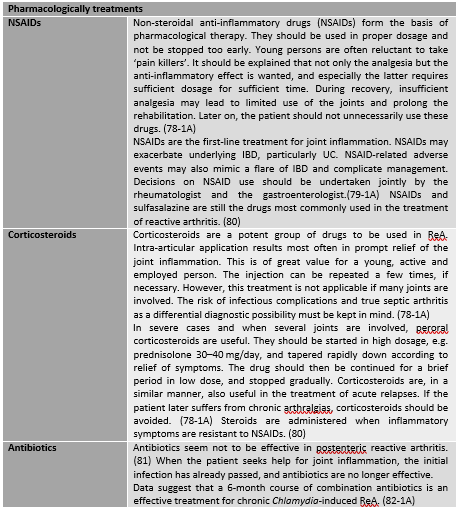
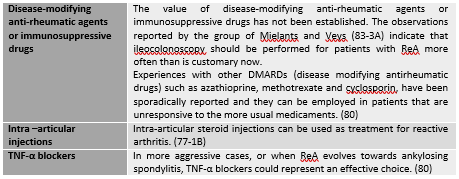
The treatment of reactive arthritis comprises mainly non-steroidal anti-inflammatory drugs, intra-articular steroid injections, and physical treatment. (77-1B)
Physical Therapy Management
[edit | edit source]
add text here
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the <a href="Template:Case Study">case study template</a>)
Resources[edit | edit source]
Clinical Bottom Line[edit | edit source]
Recent Related Research (from PubMed)[edit | edit source]
see tutorial on "Adding PubMed Feed"
Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
<span class="fck_mw_references" _fck_mw_customtag="true" _fck_mw_tagname="references" />
<a href="Category:Musculoskeletal/Orthopaedics">Orthopaedics</a> <a _fcknotitle="true" href="Category:Ankle">Ankle</a> <a _fcknotitle="true" href="Category:Rheumatology">Rheumatology</a> <a _fcknotitle="true" href="Category:Foot">Foot</a>
- ↑ Takakura Y, Tanaka Y, Kumal T, et al: Low tibial osteotomy for osteoarthritis of the ankle. J Bone joint surg Br 1995; 77:50.
- ↑ Geppert MJ, Mizel MS: Management of heel pain in inflammatory arthritides. Clin Orthop 1998; 349:93.
- ↑ J Bone Joint Surg Br. 1981;63B(4):601-9. The pathogenesis of chronic haemophilic arthropathy. Stein H, Duthie RB
- ↑ Aust Fam Physician. 2010 Mar;39(3):117-9. Charcot osteoarthropathy of the foot. Perrin BM, Gardner MJ, Suhaimi A, Murphy D
- ↑ Am Fam Physician. 2001 Nov 1;64(9):1591-8. Charcot foot: the diagnostic dilemma. Sommer TC, Lee TH.
- ↑ J Diabetes Complications. 2009 Nov-Dec;23(6):409-26. Epub 2008 Oct 17. Charcot arthropathy of the foot and ankle: modern concepts and management review. Wukich DK, Sung W.