Cervical Instability: Difference between revisions
No edit summary |
No edit summary |
||
| Line 19: | Line 19: | ||
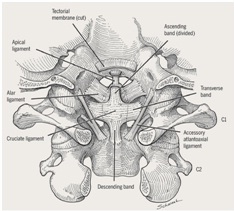
Figure 1:Posterior view of upper cervical <br>spine ligaments.<sup><ref name="Mintken et al">Mintken PE, Metrick L, Flynn TW. Upper cervical ligament testing in a patient with os odontoideum presenting with headaches. J Orthop Sports Phys Ther. 2008 Aug;38(8):465-75.</ref></sup> | Figure 1:Posterior view of upper cervical <br>spine ligaments.<sup><ref name="Mintken et al">Mintken PE, Metrick L, Flynn TW. Upper cervical ligament testing in a patient with os odontoideum presenting with headaches. J Orthop Sports Phys Ther. 2008 Aug;38(8):465-75.</ref></sup> | ||
[[Image:Ligaments Alar and Transverse.jpg|frame|left]] Cervical instability is commonly associated with the upper cervical spine. Ghanem<sup><ref name="Ghanem et al">Ghanem I, El Hage S, Rachkidi R, Kharrat K, Dagher F, Kreichati G. Pediatric cervical spine instability. J Child Orthop. 2008 Mar;2(2):71-84.</ref></sup> proposes that the anatomical nature of the upper cervical spine creates an inherent instability. The alar and transverse ligaments provide the primary source of stability for the upper cervical spine. The transverse ligament is located across the arch of the atlas and positions the dens against the anterior arch of the atlas. Functionally, the transverse ligament limits flexion and provides support from anterior translation of C1.<ref name="Dvorak et al">Dvorak J, Schneider E, Saldinger P, Rahn B. Biomechanics of the craniocervical region: the alar and transverse ligaments. J Orthop Res. 1988;6(3):452-61.</ref> <sup></sup>If the transverse ligament is disrupted by injury or is congenitally lax, neural or vascular compromise could occur. This is due to the proximity of the spinal cord and vertebral arteries.<sup><ref name="Ghanem et al">Ghanem I, El Hage S, Rachkidi R, Kharrat K, Dagher F, Kreichati G. Pediatric cervical spine instability. J Child Orthop. 2008 Mar;2(2):71-84.</ref></sup> The alar ligaments connect the cranium to C1 from the sides of the dens to the lateral borders of the foramen magnum. The alar ligaments function to prevent excessive rotation at the atlanto-occipital joint.<sup><ref name="Moore and Dalley">Moore KL, Dalley AF. Clinically Oriented Anatomy. 5th ed. Baltimore: Lippincott Williams &amp; Wilkins;2005.</ref></sup> The alar ligament is most commonly injured in motor vehicle accidents. However disruption of the alar ligament is less likely to lead to neurological or vascular injury. | [[Image:Ligaments Alar and Transverse.jpg|frame|left]] Cervical instability is commonly associated with the upper cervical spine. Ghanem<sup><ref name="Ghanem et al">Ghanem I, El Hage S, Rachkidi R, Kharrat K, Dagher F, Kreichati G. Pediatric cervical spine instability. J Child Orthop. 2008 Mar;2(2):71-84.</ref></sup> proposes that the anatomical nature of the upper cervical spine creates an inherent instability. The alar and transverse ligaments provide the primary source of stability for the upper cervical spine. The transverse ligament is located across the arch of the atlas and positions the dens against the anterior arch of the atlas. Functionally, the transverse ligament limits flexion and provides support from anterior translation of C1.<ref name="Dvorak et al">Dvorak J, Schneider E, Saldinger P, Rahn B. Biomechanics of the craniocervical region: the alar and transverse ligaments. J Orthop Res. 1988;6(3):452-61.</ref> <sup></sup>If the transverse ligament is disrupted by injury or is congenitally lax, neural or vascular compromise could occur. This is due to the proximity of the spinal cord and vertebral arteries.<sup><ref name="Ghanem et al">Ghanem I, El Hage S, Rachkidi R, Kharrat K, Dagher F, Kreichati G. Pediatric cervical spine instability. J Child Orthop. 2008 Mar;2(2):71-84.</ref></sup> The alar ligaments connect the cranium to C1 from the sides of the dens to the lateral borders of the foramen magnum. The alar ligaments function to prevent excessive rotation at the atlanto-occipital joint.<sup><ref name="Moore and Dalley">Moore KL, Dalley AF. Clinically Oriented Anatomy. 5th ed. Baltimore: Lippincott Williams &amp;amp; Wilkins;2005.</ref></sup> The alar ligament is most commonly injured in motor vehicle accidents. However disruption of the alar ligament is less likely to lead to neurological or vascular injury. | ||
'''Lower Cervical Spine (C3-C7) ''' | '''Lower Cervical Spine (C3-C7) ''' | ||
| Line 65: | Line 65: | ||
'''Clinical Testing''' | '''Clinical Testing''' | ||
In the literature, cervical spine instability consistently is described as being difficult to diagnose. Clinically, ligamentous tests to assess the stability of the upper cervical spine are limited by reliability, validity, and no consensus for sequencing of such tests. It is recommended to first assess with the Sharp-Pursor test, and then, only if it is negative, to proceed with other ligamentous tests in order of provocation (alar ligamentous stress then anterior shear test). Research remains inconclusive in what order it should be performed. Some authors feel as though if the Sharp-Pursor test is performed first, it can elicit a false negative response. Thus, if the patient does not experience a provocative test first, there would be a chance the patient’s symptoms would not be relieved by the Sharp-Pursor test. More research is required in this area to clarify the order and diagnostic accuracy for upper cervical spine instability testing.<sup></sup><ref name="Mintken et al" /> | In the literature, cervical spine instability consistently is described as being difficult to diagnose. Clinically, ligamentous tests to assess the stability of the upper cervical spine are limited by reliability, validity, and no consensus for sequencing of such tests. It is recommended to first assess with the Sharp-Pursor test, and then, only if it is negative, to proceed with other ligamentous tests in order of provocation (alar ligamentous stress then anterior shear test). Research remains inconclusive in what order it should be performed. Some authors feel as though if the Sharp-Pursor test is performed first, it can elicit a false negative response. Thus, if the patient does not experience a provocative test first, there would be a chance the patient’s symptoms would not be relieved by the Sharp-Pursor test. More research is required in this area to clarify the order and diagnostic accuracy for upper cervical spine instability testing.<sup></sup><ref name="Mintken et al" /> | ||
<br> | <br> | ||
{| style="width: 659px; height: 274px" border="1" cellspacing="1" cellpadding="1" | {| style="width: 659px; height: 274px" border="1" cellspacing="1" cellpadding="1" | ||
|+ Table 1: Clinical testing for upper cervical spine instability<sup></sup><ref name="Mintken et al" /><sup></sup> | |+ Table 1: Clinical testing for upper cervical spine instability<sup></sup><ref name="Mintken et al" /><sup></sup> | ||
|- | |- | ||
| Test<br> | | Test<br> | ||
| Line 118: | Line 118: | ||
'''Diagnostic Imaging''' | '''Diagnostic Imaging''' | ||
''' '''Radiography is the primary diagnostic tool for cervical instability. Whenever possible, radiographs should be taken in sitting or standing to account for the effect of gravity and to capture an accurate picture of the normal curvature of the patient’s spine under physiological loading.<sup><ref name="Ghanem et al" /> </sup>Radiographs should be taken in 3 views: anteroposterior, open-mouth anteroposterior, and lateral.<sup></sup><ref name="Vandemark">Vandemark RM. Radiology of the cervical spine in trauma patients: practice pitfalls and recommendations for improving efficiency and communication. AJR. 1990; 155:465-472.</ref> | ''' '''Radiography is the primary diagnostic tool for cervical instability. Whenever possible, radiographs should be taken in sitting or standing to account for the effect of gravity and to capture an accurate picture of the normal curvature of the patient’s spine under physiological loading.<sup><ref name="Ghanem et al" /> </sup>Radiographs should be taken in 3 views: anteroposterior, open-mouth anteroposterior, and lateral.<sup></sup><ref name="Vandemark">Vandemark RM. Radiology of the cervical spine in trauma patients: practice pitfalls and recommendations for improving efficiency and communication. AJR. 1990; 155:465-472.</ref> | ||
[[Image:Radiograph Fig 2.jpg|Image:Radiograph_Fig_2.jpg]] | [[Image:Radiograph Fig 2.jpg|Image:Radiograph_Fig_2.jpg]] | ||
| Line 128: | Line 128: | ||
[[Image:MRI Fig 3.jpg|Image:MRI_Fig_3.jpg]]<br> | [[Image:MRI Fig 3.jpg|Image:MRI_Fig_3.jpg]]<br> | ||
Figure 3:Cervical MRI shows<br>increased ADI (13mm) displacing <br>dens and increasing pressure on <br>the spinal cord.<sup></sup><ref name="Onerci et al" /> | Figure 3:Cervical MRI shows<br>increased ADI (13mm) displacing <br>dens and increasing pressure on <br>the spinal cord.<sup></sup><ref name="Onerci et al" /> | ||
Imaging procedures such as magnetic resonance imaging (MRI), functional MRI, computed tomography (CT) scanning, and dynamic fluoroscopy may be used when radiograph images are unclear or incomplete and/or for complex cases that require a detailed analysis of pathoanatomical structures or involve significant neurological deficits.<sup><ref name="Ghanem et al" />,<ref name="Platzer et al">Platzer P, Jaindl M, Thalhammer G, Dittrich S, Wieland T, Vecsel V, Gaebler C. Clearing the cervical spine in critically injured patients: a comprehensive c-spine protocol to avoid unnecessary delays in diagnosis. Eur Spine J. (2006); 15:1801-1810.</ref></sup> | Imaging procedures such as magnetic resonance imaging (MRI), functional MRI, computed tomography (CT) scanning, and dynamic fluoroscopy may be used when radiograph images are unclear or incomplete and/or for complex cases that require a detailed analysis of pathoanatomical structures or involve significant neurological deficits.<sup><ref name="Ghanem et al" />,<ref name="Platzer et al">Platzer P, Jaindl M, Thalhammer G, Dittrich S, Wieland T, Vecsel V, Gaebler C. Clearing the cervical spine in critically injured patients: a comprehensive c-spine protocol to avoid unnecessary delays in diagnosis. Eur Spine J. (2006); 15:1801-1810.</ref></sup> | ||
Revision as of 22:53, 20 March 2011
Let me know if you need any assistance.Be the first to edit this page and have your name permanently included as the originating editor, see the editing pages tutorial for help.
|
Original Editor - Your name will be added here if you created the original content for this page. Lead Editors - If you would like to be a lead editor on this page, please contact us. |
Clinically Relevant Anatomy[edit | edit source]
The cervical spine is structurally distinguished by differences between the upper cervical spine (C1 and C2) and the lower cervical spine (C3-C7) segments. Anatomical and functional distinctions allow for differences in segmental mobility and movement direction. The upper cervical spine allows for a greater degree of rotation with some frontal and sagittal movement. In contrast, the lower cervical spine moves in flexion-extension and inclination-rotation.[1]
Upper Cervical Spine (C1-C2)
Figure 1:Posterior view of upper cervical
spine ligaments.[2]
Cervical instability is commonly associated with the upper cervical spine. Ghanem[1] proposes that the anatomical nature of the upper cervical spine creates an inherent instability. The alar and transverse ligaments provide the primary source of stability for the upper cervical spine. The transverse ligament is located across the arch of the atlas and positions the dens against the anterior arch of the atlas. Functionally, the transverse ligament limits flexion and provides support from anterior translation of C1.[3] If the transverse ligament is disrupted by injury or is congenitally lax, neural or vascular compromise could occur. This is due to the proximity of the spinal cord and vertebral arteries.[1] The alar ligaments connect the cranium to C1 from the sides of the dens to the lateral borders of the foramen magnum. The alar ligaments function to prevent excessive rotation at the atlanto-occipital joint.[4] The alar ligament is most commonly injured in motor vehicle accidents. However disruption of the alar ligament is less likely to lead to neurological or vascular injury.
Lower Cervical Spine (C3-C7)
In contrast to the upper cervical spine, the frontal plane orientation of facet joints of the lower cervical spine serves as the primary source of stability. In addition, spinal ligaments including ligamentum nuchae, anterior longitudinal ligament, posterior longitudinal ligament, and ligamentum flavum contribute to stability in the lower cervical spine.
Mechanism of Injury / Pathological Process[edit | edit source]
Traumatic
- Whiplash
- Motor vehicle accident
- Head/neck surgery
Systemic
- Recent upper respiratory infection
Congenital
- Down syndrome
- Juvenile rheumatoid arthritis
- Ankylosing spondylosis
- Cerebral palsy
- Neurofibromatosis
- Os odontoideum
- Klippel-Feil syndrome (KFS)
Clinical Presentation[edit | edit source]
Mintken et al[2] described the cardinal symptoms of clinical instability: drop attacks, facial or lip paresthesias, bilateral or quadrilateral limb paresthesias, or nystagmus. These signs and symptoms are usually provoked with active or passive movement of the head or neck. Furthermore, in their case study, they address other secondary impairments such as dizziness and bilateral blurred vision.
In a Delphi survey study, Cook et al[5] reported that physical therapists attribute the following symptoms with cervical instability:
- “intolerance to prolonged static postures”
- “fatigue and inability to hold head up”
- "better with external support, including hands or collar"
- "frequent need for self-manipulation"
- "feeling of instability, shaking, or lack of control"
- "frequent episodes of acute attacks"
- "sharp pain, possibly with sudden movements"
Since there is little evidence supportive of clinical tests for cervical spine instability, recognition of these symptoms along with clinical judgment could warrant referral. During examination, it is important to collect a thorough history from the patient to understand the patient’s chief complaint, signs and symptoms - neural or vascular compromise, duration and pain level.
Diagnostic Procedures[edit | edit source]
Clinical Testing
In the literature, cervical spine instability consistently is described as being difficult to diagnose. Clinically, ligamentous tests to assess the stability of the upper cervical spine are limited by reliability, validity, and no consensus for sequencing of such tests. It is recommended to first assess with the Sharp-Pursor test, and then, only if it is negative, to proceed with other ligamentous tests in order of provocation (alar ligamentous stress then anterior shear test). Research remains inconclusive in what order it should be performed. Some authors feel as though if the Sharp-Pursor test is performed first, it can elicit a false negative response. Thus, if the patient does not experience a provocative test first, there would be a chance the patient’s symptoms would not be relieved by the Sharp-Pursor test. More research is required in this area to clarify the order and diagnostic accuracy for upper cervical spine instability testing.[2]
| Test |
Description |
Positive Test |
Diagnostic Accuracy |
| Sharp-Pursor Test |
|
Reduction in symptoms with and/or no sliding or “clunking” noted with PA movement. |
Sensitivity= 0.69 Specificity= 0.96 +LR= 17.3 -LR=0.32 |
| Alar Ligament Stress Test |
|
With passive movement of the head there is a lag or delay of C2 spinous process movement |
No available research |
| Anterior Shear Test ( Transverse Ligament Test) |
|
Sensation of lump in the throat or the presence of cardinal signs. |
No available research |
Diagnostic Imaging
Radiography is the primary diagnostic tool for cervical instability. Whenever possible, radiographs should be taken in sitting or standing to account for the effect of gravity and to capture an accurate picture of the normal curvature of the patient’s spine under physiological loading.[1] Radiographs should be taken in 3 views: anteroposterior, open-mouth anteroposterior, and lateral.[6]
Figure 2: Lateral cervical
radiograph with increased ADI.[7]
Standard anteroposterior radiographs provide visualization of the lower cervical spine, while open-mouth radiographs provide visualization of the upper cervical spine. Lateral radiographs allow for the measurement of the atlantodens interval (ADI), the space between the posterior surface of the anterior ring of the atlas and the anterior surface of the dens. An ADI greater than 3mm in adults or 5mm in children is indicative of atlantoaxial instability. In adults, an ADI of greater than 5mm typically indicates a rupture of the transverse ligament. However, in patient populations with chronic ligamentous laxity such as Rheumatoid Arthritis, Down Syndrome, or congenital abnormalties, the ADI measurement may not be as useful for diagnosing laxity of the transverse ligament. Such patients may present as asymptomatic. It is important to consider the increased risk associated with ligamentous laxity in these populations and to exercise caution in treatment.[8],[9]
Figure 3:Cervical MRI shows
increased ADI (13mm) displacing
dens and increasing pressure on
the spinal cord.[7]
Imaging procedures such as magnetic resonance imaging (MRI), functional MRI, computed tomography (CT) scanning, and dynamic fluoroscopy may be used when radiograph images are unclear or incomplete and/or for complex cases that require a detailed analysis of pathoanatomical structures or involve significant neurological deficits.[1],[10]
Outcome Measures[edit | edit source]
There are no patient reported outcome measures to specifically address cervical instability. However clinicians can address the patient’s reported impairments by administering the Numeric Pain Rating Scale (NPRS) and Neck Disability Index (NDI).
Numeric Pain Rating Scale (NPRS)
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions
[edit | edit source]
Upon examination findings of positive ligamentous testing and clinically observable signs such as cardinal symptoms, a referral for imaging should be implemented. Depending on the mechanism of injury or the pathological origin of cervical spine instability, the mode for medical management varies. Ghanem reports that treatments include surgical correction, immobilization or traction depending on the diagnosis of the patient’s case.[1]Patients may benefit from conservative physical therapy interventions, especially those patients without severe ligamentous injury or neurovascular complications. Conservative therapy should focus on motor control retraining exercises for the cervical spine including the deep neck flexors. Manual therapy such as non-thrust manipulation and soft tissue mobilization could be considered to improve mobility of adjacent regions and for symptomatic relief. Aggressive manual techniques that would place strain through the compromised ligaments or cause neurovascular signs/symptoms are contraindicated.
Differential Diagnosis
[edit | edit source]
- Fracture
- Cervical myelopathy
- Vertebral basilar insufficiency
- Cervical spondylosis
- Torticollis
- Mechanical neck pain
- Headache
- TMJ dysfunction
Key Evidence
[edit | edit source]
Resources
[edit | edit source]
add appropriate resources here
Case Studies[edit | edit source]
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Ghanem I, El Hage S, Rachkidi R, Kharrat K, Dagher F, Kreichati G. Pediatric cervical spine instability. J Child Orthop. 2008 Mar;2(2):71-84.
- ↑ 2.0 2.1 2.2 2.3 Mintken PE, Metrick L, Flynn TW. Upper cervical ligament testing in a patient with os odontoideum presenting with headaches. J Orthop Sports Phys Ther. 2008 Aug;38(8):465-75.
- ↑ Dvorak J, Schneider E, Saldinger P, Rahn B. Biomechanics of the craniocervical region: the alar and transverse ligaments. J Orthop Res. 1988;6(3):452-61.
- ↑ Moore KL, Dalley AF. Clinically Oriented Anatomy. 5th ed. Baltimore: Lippincott Williams &amp; Wilkins;2005.
- ↑ Cook C, Brismée JM, Fleming R, Sizer PS Jr. Identifiers suggestive of clinical cervical spine instability: a Delphi study of physical therapists. Phys Ther. 2005 Sep;85(9):895-906.
- ↑ Vandemark RM. Radiology of the cervical spine in trauma patients: practice pitfalls and recommendations for improving efficiency and communication. AJR. 1990; 155:465-472.
- ↑ 7.0 7.1 Onerci M, Ogretmenoglu O, Ozcan OE. Atlantoaxial subluxation after tonsillectomy and adenoidectomy. Otolaryngol Head Neck Surg. 1997 Feb;116(2):271-3.
- ↑ Neva MH, Hakkinen A, Makinen H, Hannonen P, Kauppi M, Sokka T. High prevalence of asymptomatic cervical spine subluxation in patients with rheumatoid arthritis waiting for orthopaedic surgery. Ann Rheum Dis. 2006;65:884-888.
- ↑ Ali FE, Al-Bustan MA, Al-Busairi WA, Al-Mulla FA, Esbaita EY. Cervical spine abnormalities associated with Down syndrome. International Orthopaedics (SICOT) 2006;30:284-289.
- ↑ Platzer P, Jaindl M, Thalhammer G, Dittrich S, Wieland T, Vecsel V, Gaebler C. Clearing the cervical spine in critically injured patients: a comprehensive c-spine protocol to avoid unnecessary delays in diagnosis. Eur Spine J. (2006); 15:1801-1810.
- Ghanem I, El Hage S, Rachkidi R, Kharrat K, Dagher F, Kreichati G. Pediatric
cervical spine instability. J Child Orthop. 2008 Mar;2(2):71-84. - Mintken PE, Metrick L, Flynn TW. Upper cervical ligament testing in a patient
with os odontoideum presenting with headaches. J Orthop Sports Phys Ther. 2008
Aug;38(8):465-75. - Dvorak J, Schneider E, Saldinger P, Rahn B. Biomechanics of the craniocervical
region: the alar and transverse ligaments. J Orthop Res. 1988;6(3):452-61. - Moore KL, Dalley AF. Clinically Oriented Anatomy. 5th ed. Baltimore: Lippincott Williams & Wilkins;2005.
- Cook C, Brismée JM, Fleming R, Sizer PS Jr. Identifiers suggestive of clinical
cervical spine instability: a Delphi study of physical therapists. Phys Ther.
2005 Sep;85(9):895-906. - Vandemark RM. Radiology of the cervical spine in trauma patients: practice pitfalls and recommendations for improving efficiency and communication. AJR. 1990; 155:465-472.
- Onerci M, Ogretmenoglu O, Ozcan OE. Atlantoaxial subluxation after tonsillectomy and adenoidectomy. Otolaryngol Head Neck Surg. 1997 Feb;116(2):271-3.
- Ali FE, Al-Bustan MA, Al-Busairi WA, Al-Mulla FA, Esbaita EY. Cervical spine abnormalities associated with Down syndrome. International Orthopaedics (SICOT) 2006;30:284-289.
- Neva MH, Hakkinen A, Makinen H, Hannonen P, Kauppi M, Sokka T. High prevalence of asymptomatic cervical spine subluxation in patients with rheumatoid arthritis waiting for orthopaedic surgery. Ann Rheum Dis. 2006;65:884-888.
- Platzer P, Jaindl M, Thalhammer G, Dittrich S, Wieland T, Vecsel V, Gaebler C. Clearing the cervical spine in critically injured patients: a comprehensive c-spine protocol to avoid unnecessary delays in diagnosis. Eur Spine J. (2006); 15:1801-1810.
| The content on or accessible through Physiopedia is for informational purposes only. Physiopedia is not a substitute for professional advice or expert medical services from a qualified healthcare provider. Read more. |