Cervicogenic Headache: Difference between revisions
No edit summary |
No edit summary |
||
| Line 193: | Line 193: | ||
<br> Jull et al<ref name="Jull" /> reported that a six week physiotherapy program including manual therapy and exercise interventions was an effective treatment option for reduction of cervicogenic headache symptoms and decreasing medication intake in both the short term and at one-year follow-up. | <br> Jull et al<ref name="Jull" /> reported that a six week physiotherapy program including manual therapy and exercise interventions was an effective treatment option for reduction of cervicogenic headache symptoms and decreasing medication intake in both the short term and at one-year follow-up. | ||
<br> | {| width="100%" cellspacing="1" cellpadding="1" | ||
|- | |||
| {{#ev:youtube|zmh1FisBeeM|300}} <ref>ShaychiITA. Tibialis Posterior Basic Strengthening. Available from: http://www.youtube.com/watch?v=zmh1FisBeeM [last accessed 24/11/12]</ref> | |||
| {{#ev:youtube|1smVSuQiQx8|300}} <ref>OptimumCareProviders. 1.2 Deep Neck Flexor - Longus Colli Strengthening Level 2. Available from: http://www.youtube.com/watch?v=1smVSuQiQx8 [last accessed 09/03/13]</ref> | |||
|- | |||
| {{#ev:youtube|Rj4Y5JGNPZs|300}}<ref> ReligiosoPT. Supine Thoracic Thrust. Available from: http://www.youtube.com/watch?v=Rj4Y5JGNPZs[last accessed 09/03/13]|}</ref> | |||
| {{#ev:youtube|IyNntKOE0J4|300}}<ref> DEEPAKKUMARCAPRI. Self SNAGs Self Treatment Cervical Spine pain & Stiffness Mulligan Concept. Available from: http://www.youtube.com/watch?v=IyNntKOE0J4[last accessed 09/03/13]|}</ref> | |||
|} | |||
<br> | |||
==== Outcome Measures ==== | ==== Outcome Measures ==== | ||
Revision as of 07:53, 10 March 2013
Original Editor - Christopher Covert, Jeremy Brady, Mary Harris, Thomas Lawlor and Rick Wetherald as part of the Texas State University Evidence-based Practice Project
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Search Strategy[edit | edit source]
Databases Searched: PubMed, CINAHL, Cochrane, JOSPT, Wiley
Keywords Searched: atlantioaxial, cervicogenic headache, cervical headache, cervical spine, joint mobilization, trigeminocervical, "medical management" cervicogenic headache
Search Timeline: April 4th 2011 - May 1st, 2011
Definition/Description[edit | edit source]
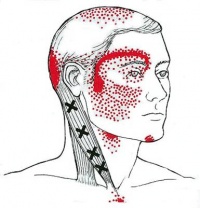
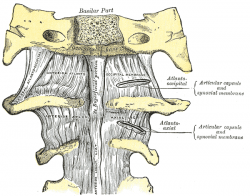
A chronic headache that arises from the atlanto-occipital and upper cervical joints and perceived in one or more regions of the head and/or face.[1] These occur due to a neck disorder or lesion and feature the converging of trigeminal and cervical afferents in the trigeminocervical nucleus within the upper cervical spinal cord.[2] By definition the headache should be abolished following a diagnostic blockade of a cervical structure or its nerve supply.[3]
The International Headache Society (IHS) has validated cervicogenic headache as a headache type that is hypothesized to originate due to nociception in the cervical area. [4]
Epidemiology/Etiology[edit | edit source]
Of all chronic headaches, the incidence of cervicogenic headache has been estimated to be 14-18%,[5] though in a recent population-based study a 2.2% prevalence was found[6]. As such, it is important we can distinguish cervicogenic headache from the other headaches like migraine, tension type headache.
The term cervicogenic headache (CGH) was coined almost 3 decades ago, and the general condition of pain located in the head but originating in the cervical spine was described over 100 years ago. It is similar to other non-specific spinal conditions in its relative lack of high level evidence regarding pathoanatomical etiology. Since there is no objective test set for diffinitive diagnosis of CGH, the condition is ruled in, and treatment chosen, based on the patient's subjective report of pain patterns. [7]
There is some evidence that multiple structures in the upper cervical spine can be the source that is referring pain into the head. The implicated structures are generally centered around C1, C2, and C3 spinal levels. This may include the joints, disc, ligaments, and musculature.[8] The lower cervical spine may play an indirect role in pain production if dysfunctional, but there is no evidence of a direct referral pattern.[8] Through controlled nerve blocking of various structures in the cervical spine, it appears that the zygoapophyseal joints, especially those of C2/C3, are the most common sources of CGH pain. This finding is even more common in patients with a history of whiplash. [8]
Characteristics/Clinical Presentation[edit | edit source]
Challenging to diagnose clinically, but often includes the below:
- Unilateral “ram’s horn” or unilateral dominant headache[9]
- Excluding those with bilateral headache or symptoms that typify migrane headaches
- Exacerbated by neck movement or posture[9]
- Tenderness of the upper 3 cervical spine joints[9]
- Association with neck pain or dysfunction[10]
- Definitive diagnosis made through selective nerve blocking through injection of specific sites[8]
- Compared to migraine headache and control groups, cervicogenic headache group patients tend to have increased tightness of upper trapezius, levator scapulae, scales and suboccipital extensors[1]
Differential Diagnosis[edit | edit source]
| Type | Location | Intensity | Frequency | Duration | Additional Symptoms |
| Cluster | Unilateral: (orbital, supraorbital, temporal) | Severe | 1x every other day -> 8x day | 15-180 minutes | Associated with ipsilateral: conjunctival injection, lacrimation, nasal congestion, rhinorrhoea, forehead and facial sweating, miosis, ptosis, eyelid edema. Restlessness or agitation. |
| Tension | Bilateral | Mild-Moderate | >15day/mo, >3 mo | Hours-continuous |
Pressing, tightening <1 of photophobia, phonophobia or mild nausea |
| Migraine without aura | Unilateral: Frontotemporal in adults, Occipital in children | Moderate-Severe | >14 days/month |
4-72 hours | Flickering lights/spots in vision, pulsating quality, nausea, photophobia, phonophobia |
For more detailed classification information
| Cluster | Tension | Migrane |

|

|

|
Cybex Dynamometry[edit | edit source]
Another possibility to distinguish cervicogenic headache from migraine and tension headache is the use of a Cybex dynamometry.[11] Testing using Cybex dynamometry has shown that the ranges of cervical flexion, extension and rotation are significantly less in patients with cervicogenic than in patients with migraine and tension type headache (p < 0.001). Investigators also found that tenderness is a factor that varies between patients with CGH and patients with migraine or tension type headaches. Bovim measured pressure pain thresholds at ten points on the head and suboccipital region in patients with CGH, tension type headache and migraine.[12] Lower scores were found in patient with cervicogenic headaches than without.
Examination[edit | edit source]
Diagnostic Criteria (as described by the IHS)[3]:[edit | edit source]
- Pain localized in the neck and occiput, which can spread to other areas in the head, such as forehead, orbital region, temples,vertex, or ears, usually unilateral.
- Pain is precipitated or aggravated by specific neck movements or sustained postures.
- At least one of the following:
- Resistance to or limitation of passive neck movements
- Changes in neck muscle contour, texture, tone, or response to active and passive stretching and contraction
- Abnormal tenderness of neck musculature
- Radiological examination reveals at least one of the following:
- Movement abnormalities in flexion/extension
- Abnormal posture
- Fractures, congenital abnormalities, bone tumors, rheumatoid arthritis, or other distinct pathology (not spondylosis orosteochondrosis)
Flexion-Rotation Test Sn = 0.91, Sp = 0.90[13]
[edit | edit source]
The inverse relationship between headache severity of CGH and ROM towards the most restricted side for the Cervical Flexion-Rotation Test (FRT) was statistically significant for all patients with cervicogenic headaches.[13] The patient should feel no pain at the time of the test. During this test, the neck of the patient is passively held in end range flexion. The therapist rotates the neck to each side until they feel resistance or until the patient says they are in pain. At this end point, the therapist makes a visual estimate of the rotation range and says on which side the FRT was positive or negative. The test was positive when the estimated range was reduced by more than 10° from the anticipated normal range (44°).
"Red flags"[edit | edit source]
- Sudden onset of a new severe headache;
- A worsening pattern of a pre-existing headache in the absence of obvious predisposing factors;
- Headache associated with fever, neck stiff ness, skin rash, and with a history of cancer, HIV, or other systemic illness;
- Headache associated with focal neurologic signs other than typical aura;
- Moderate or severe headache triggered by cough, exertion, or bearing down; and
- New onset of a headache during or following pregnancy.
Patients with one or more red flags should be referred for an immediate medical consultation and further investigation.[13]
Medical Management (current best evidence)[edit | edit source]
The failure to conclusively demonstrate a specific disease or dysfunction of the neck in relation to cervicogenic headache has been an impediment to specific treatment for individuals with the diagnosis.
Cervical epidural steroid injections: Indicated for multilevel disc or spine degeneration
Nerve Blocks: Disrupting the cascade of signals leading to sensitization to central mechanisms via:
- Nerve blocks
- Trigger point injections
- Radiofrequency thermal neurolysis
Current best evidence suggests that there is not sufficient evidence meeting the EBM criteria to support the use of RF facet denervation for cervicogenic headaches.[14]
Surgical interventions: Often only provide temporary relief with the possibility of longer intensification of pain.[1] Procedures Include:
- Neurotomy
- Dorsal rhizotomy
- Microvascular decompression of nerve roots
Other Medications:
Tricyclic antidepressants - Used at lower dosage than required for pts diagnosed with depression
Muscle relaxants - Related to the CNS, may be beneficial, evidence is still pending
Botulinum toxin - A neurotoxin injected into tender muscles to reduce hypertonia
Physical Therapy Management (current best evidence)[edit | edit source]
The preferred practice pattern for cervicogenic headache is 5D: Impaired Motor Function and Sensory Integrity Associated with Nonprogressive Disorders of the Central Nervous System-Acquired in Adolescence or Adulthood. Goodman states that "Although this type of headache is responsive to therapy oriented at treating the soft tissue restrictions, the method of examination, assessment, and treatment needs to be specific to the neck and occiput."[1]
Treatment[edit | edit source]
- Cervical spine manipulation or mobilization[15]
- Strengthening exercises[15]
- Deep neck flexors
- Upper quarter muscles
- Thoracic spine thrust manipulation & exercise[16]
- C1-C2 Self-sustained Natural Apophyseal Glide (SNAG)[17]
- shown to be effective for reducing cervicogenic headache symptoms
- shown to be effective for reducing cervicogenic headache symptoms
Jull et al[9] reported that a six week physiotherapy program including manual therapy and exercise interventions was an effective treatment option for reduction of cervicogenic headache symptoms and decreasing medication intake in both the short term and at one-year follow-up.
| [18] | [19] |
| [20] | [21] |
Outcome Measures[edit | edit source]
- Neck_Disability_Index
- Headache Disability Index
- Northwick Park Neck Pain Questionnaire
- Numeric Pain Rating Scale
- Pain visual analog scale
- Headache frequency and duration
Treatment Examples[edit | edit source]
| Seated CT Manipulation | Seated Mid Thoracic Manipulation |
| Deep Neck Flexor Exercises | |
| Middle Trapezius Strengthening | Lower Trapezius Strengthening |

|

|
Key Research[edit | edit source]
- Jull G, Stanton W. Predictors of responsiveness to physiotherapy management of cervicogenic headache. Cephalalgia. 2005;25:101-108.[9]
- Hall T et all. Clinical Evaluation of Cervicogenic Headache: A Clinical Perspective. Journal of Manual and Manipulative Therapy. 2008;16:73-80.[13]
Resources[edit | edit source]
- International Headache Society
- Diagnosis and management of cervicogenic headache. Sizer PS Jr, Phelps V, Azevedo E, Haye A, Vaught M. Pain Pract. 2005 Sep;5(3):255-74.
- The diagnostic validity of the cervical flexion-rotation test in C1/2-related cervicogenic headache. Ogince M, Hall T, Robinson K, Blackmore AM. Man Ther. 2007 Aug;12(3):256-62.
- Efficacy of a C1-C2 self-sustained natural apophyseal glide (SNAG) in the management of cervicogenic headache. Hall T, Chan HT, Christensen L, Odenthal B, Wells C, Robinson K. J. Orthop Sports Phys Ther. 2007 Mar;37(3):100-7.
- Clinical evaluation of cervicogenic headache: a clinical perspective. Fernández-de-Las-Peñas C. J Man Manip Ther. 2008;16(2):81.
Recent Case Studies[edit | edit source]
- J Man Manip Ther. 2007;15(1):10-24.
- van Duijn J, van Duijn AJ, Nitsch W. Orthopaedic manual physical therapy including thrust manipulation and exercise in the management of a patient with cervicogenic headache: a case report.
Clinical Bottom Line[edit | edit source]
Cervicogenic headaches are brought on by neck dysfunction and present in a unilateral "ram’s horn" pattern. The flexion-rotation test is a diagnostic method with high sensitivity and specificity that assists in differentiating it from other types, such as migraines, tension, and cluster headaches. PT treatment should include cervical mobilization, cervical or thoracic thrust manipulation, and deep neck flexor and upper quarter strengthening.
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1LC7_OBLVE9Hc3UrOAdwx9miGAMRquG4Mg6-pr5u6uky_VMIMD|charset=UTF-8|short|max=10: Error parsing XML for RSS
References
[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Goodman, C, Fuller, K. Pathology: Implications for the Physical Therapist. 3rd ed. St. Louis: Saunders Elsevier, 2009.
- ↑ Bogduk N, Govind J. Cervicogenic headache: an assessment of the evidence on clinical diagnosis, invasive tests, and treatment. Lancet Neurol 2009; 8: 959–68.
- ↑ 3.0 3.1 HIS Classification ICHD-II. Cervicogenic headache [M99]. http://ihs-classification.org/en/02_klassifikation/03_teil2/11.02.01_cranial.html (accessed 13 April 2011).
- ↑ Headache Classification Subcommittee of the International HeadacheSociety. The international classification of headache disorders.2nd edition. Cephalalgia 2004;24:suppl 1.
- ↑ Pfaffenrath and Kaube(1990); Nilsson (1995)
- ↑ Antonaci F, Sjaastad O. Cervicogenic headache: a real headache. Curr Neurol Neurosci Rep. 2011;4:149-155
- ↑ Haldeman S. Dagenais S. Choosing a treatment for cervicogenic headache: when? what? how much?. The Spine journal 2010;10 169-171
- ↑ 8.0 8.1 8.2 8.3 Becker WJ. Cervicogenic Headache: Evidence that the neck is a pain generator. Headache. 2010;4 699-705
- ↑ 9.0 9.1 9.2 9.3 9.4 Jull G, Stanton W. Predictors of responsiveness to physiotherapy management of cervicogenic headache. Cephalalgia. 2005;25:101-108.
- ↑ Haas M, Spegman A, Peterson D, Aickin M, Vavrek D. Dose response and efficacy of spinal manipulation for chronic cervicogenic headache: a pilot randomized controlled trial. Spine Journal [serial on the Internet]. (2010, Feb), [cited May 1, 2011]; 10(2): 117-128.
- ↑ Zwart JA. Neck mobility in different headache disorders. Headache 1997;37:6–11.
- ↑ Bovim G. Cervicogenic headache, migraine, and tension-type headache. Pressure-pain threshold measurements. Pain 1992;51: 169–73.
- ↑ 13.0 13.1 13.2 13.3 Hall T et all. Clinical Evaluation of Cervicogenic Headache: A Clinical Perspective. Journal of Manual and Manipulative Therapy. 2008;16:73-80. Cite error: Invalid
<ref>tag; name "Hall" defined multiple times with different content - ↑ Boxem K, Erd M, Brinkhuize T, Patijn J, Kleef M, Zundert J. Radiofrequency and Pulsed Radiofrequency Treatment of Chronic Pain Syndromes: The Available Evidence. Pain Practice 2008;8:385-393.
- ↑ 15.0 15.1 Fritz JM, Brennan GP. Preliminary Examination of a Proposed Treatment-Based Classification System for Patients Receiving Physical Therapy Interventions for Neck Pain. Physical Therapy. 2007;87:513-524.
- ↑ Cleland et al. Examination of a Clinical Prediction Rule to Identify Patients with Neck Pain Likely to Benefit from Thoracic Spine Thrust Manipulation and a General Cervical Range of Motion Exercise: Muti-Center Randomized Clinical Trial. Physical Therapy. 2010;90:1239-1253.
- ↑ Hall T et al. Efficacy of a C1-C2 Self-sustained Natural Apophyseal Glide (SNAG) in the Management of Cervicogenic Headache JOSPT 2007;37:100-107.
- ↑ ShaychiITA. Tibialis Posterior Basic Strengthening. Available from: http://www.youtube.com/watch?v=zmh1FisBeeM [last accessed 24/11/12]
- ↑ OptimumCareProviders. 1.2 Deep Neck Flexor - Longus Colli Strengthening Level 2. Available from: http://www.youtube.com/watch?v=1smVSuQiQx8 [last accessed 09/03/13]
- ↑ ReligiosoPT. Supine Thoracic Thrust. Available from: http://www.youtube.com/watch?v=Rj4Y5JGNPZs[last accessed 09/03/13]|}
- ↑ DEEPAKKUMARCAPRI. Self SNAGs Self Treatment Cervical Spine pain & Stiffness Mulligan Concept. Available from: http://www.youtube.com/watch?v=IyNntKOE0J4[last accessed 09/03/13]|}