Chronic Obstructive Pulmonary Disease Rehabilitation Class: Difference between revisions
Laura McCabe (talk | contribs) No edit summary |
No edit summary |
||
| Line 642: | Line 642: | ||
O'Shea, S.D., Taylor, N.F. and Paratz, J.D. 2007. [horizontal ellipsis]But Watch Out for the Weather: FACTORS AFFECTING ADHERENCE TO PROGRESSIVE RESISTANCE EXERCISE FOR PERSONS WITH COPD. Journal of Cardiopulmonary Rehabilitation & Prevention, 27 (3) May/June, pp.166-174. | O'Shea, S.D., Taylor, N.F. and Paratz, J.D. 2007. [horizontal ellipsis]But Watch Out for the Weather: FACTORS AFFECTING ADHERENCE TO PROGRESSIVE RESISTANCE EXERCISE FOR PERSONS WITH COPD. Journal of Cardiopulmonary Rehabilitation & Prevention, 27 (3) May/June, pp.166-174. | ||
British Thoracic Society. Standards of care committee on pulmonary rehabilitation. 2001. Thorax, 56, pp.827-834. | British Thoracic Society. Standards of care committee on pulmonary rehabilitation. 2001. Thorax, 56, pp.827-834. | ||
Davidson, A.C. and Morgan, M.D.L. 1998. A UK survey of the provision of pulmonary rehabilitation. Thorax, 53, pp. 86. | Davidson, A.C. and Morgan, M.D.L. 1998. A UK survey of the provision of pulmonary rehabilitation. Thorax, 53, pp. 86. | ||
Guëll, M.R., Lucas, P., Gáldiz, J.B., Montemayor, T., González-Moro, J.M.R., Gorostiza, A., Ortega, F., Bellón, J.M. and Guyatt, G. 2008. Home vs hospital-based pulmonary rehabilitation for patients with chronic obstructive pulmonary disease: A Spanish multicenter trial. Archive Bronconeumol, 44 (10), pp.512-518. | Guëll, M.R., Lucas, P., Gáldiz, J.B., Montemayor, T., González-Moro, J.M.R., Gorostiza, A., Ortega, F., Bellón, J.M. and Guyatt, G. 2008. Home vs hospital-based pulmonary rehabilitation for patients with chronic obstructive pulmonary disease: A Spanish multicenter trial. Archive Bronconeumol, 44 (10), pp.512-518. | ||
Khdour, M.R., Agus, A.M., Kidney, J.C., Smyth, B.M., Elnay, J.C. and Crealey, G.E. 2011. Cost-ultility analysis of a pharmacy-led self-management programme for patients with COPD. International Journal of Clinical Pharmacy, 33, pp. 665-673. | Khdour, M.R., Agus, A.M., Kidney, J.C., Smyth, B.M., Elnay, J.C. and Crealey, G.E. 2011. Cost-ultility analysis of a pharmacy-led self-management programme for patients with COPD. International Journal of Clinical Pharmacy, 33, pp. 665-673. | ||
Lacasse, Y., Goldstein, R., Lasserson, T.J. and Martin, S. 2006. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Systematic Review, CD003793. | Lacasse, Y., Goldstein, R., Lasserson, T.J. and Martin, S. 2006. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Systematic Review, CD003793. | ||
Maltais, F., Bourbeau, J., Shapiro, S., Lacasse, Y., Perrault, H., Baltzan, M., Hernandez, P., Rouleau, M., Julien, M., Parenteau, S., Paradis, B., Levy, R.D., Camp, P., Lecours, R., Audet, R., Hutton, B., Penrod, J.R., Picard, D. and Bernard, S. 2008. Effects of home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease. Annals of Internal Medicine, 149, pp.869-878. | Maltais, F., Bourbeau, J., Shapiro, S., Lacasse, Y., Perrault, H., Baltzan, M., Hernandez, P., Rouleau, M., Julien, M., Parenteau, S., Paradis, B., Levy, R.D., Camp, P., Lecours, R., Audet, R., Hutton, B., Penrod, J.R., Picard, D. and Bernard, S. 2008. Effects of home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease. Annals of Internal Medicine, 149, pp.869-878. | ||
Strijbos, J.H., Postma, D.S., van Altena, R., Gimeno, F. and Koëter, G.H. 1996. A comparison between an outpatient hospital-based pulmonary rehabilitation program and a home-care pulmonary rehabilitation program in patients with COPD. A follow up of 18 months. Chest, 109, pp. 366-372. | Strijbos, J.H., Postma, D.S., van Altena, R., Gimeno, F. and Koëter, G.H. 1996. A comparison between an outpatient hospital-based pulmonary rehabilitation program and a home-care pulmonary rehabilitation program in patients with COPD. A follow up of 18 months. Chest, 109, pp. 366-372. | ||
Ward, J.A., Akers, G., Ward, D.G., Pinnuck, M., Williams, S., Trott, J. and Halpin, D.M.G. 2002. Feasibility and effectiveness of a pulmonary rehabilitation programme in a community hospital setting. British Journal of General Practice, 52, pp.539-542. | Ward, J.A., Akers, G., Ward, D.G., Pinnuck, M., Williams, S., Trott, J. and Halpin, D.M.G. 2002. Feasibility and effectiveness of a pulmonary rehabilitation programme in a community hospital setting. British Journal of General Practice, 52, pp.539-542. | ||
Waterhouse, J.C., Walters, S.J., Oluboyede, Y. and Lawson, R.A. 2010. A randomized 2 x 2 trial of community versus hospital pulmonary rehabilitation for chronic obstructive pulmonary disease followed by telephone or conventional follow-up. Health Technology Assessment, 14, pp.1-164. | Waterhouse, J.C., Walters, S.J., Oluboyede, Y. and Lawson, R.A. 2010. A randomized 2 x 2 trial of community versus hospital pulmonary rehabilitation for chronic obstructive pulmonary disease followed by telephone or conventional follow-up. Health Technology Assessment, 14, pp.1-164. | ||
Slovic, P., Finucane, M.L., Peters, E. and MacGregor, D.G. 2004. Risk as analysis and risk as feelings: some thoughts about effect, reason, risk and rationality. ''Risk Analysis'', 24 (2), pp.311-322.<br> | Slovic, P., Finucane, M.L., Peters, E. and MacGregor, D.G. 2004. Risk as analysis and risk as feelings: some thoughts about effect, reason, risk and rationality. ''Risk Analysis'', 24 (2), pp.311-322.<br> | ||
BBC, 2012. commmissioningsuccess.com. [Online] <br>Available at: http://commissioningsuccess.com/2012/07/nhs-budget-squeeze-could-last-a-decade/<br>[Accessed 20th October 2012].<br><br> | |||
Britton, M., 2003. The burden of COPD in the UK: results from the Confronting COPD survey. Respiratory Medicine, 97(Supplement C), pp. S71-S79.<br> | |||
Gardiner, C. et al., 2010. Exploring the care needs of patients with advanced COPD: An Overview of the literature. Respiratory Medicine, Volume 104, pp. 159-165.<br> | |||
Crawford, R. & Emmerson, C., 2012. NHS and social care funding: the outlook to 2021/22, s.l.: Institute for Fiscal Studies.<br> | |||
Matthew, J. & Diffley, M., 2007. Managing Long-term Conditions, Edinburgh: Audit Scotland. | |||
NHS Lothian, 2011. Chronic Obstructive Pulmonary Disease Guideline, Edinburgh: NHS Lothian. | |||
NHS Quality Improvement Scotland, 2010. Healthcare Improvement Scotland COPD services - Clinical Standards, Edinburgh: NHS Quality Improvement Scotland.<br>The Scottish Government, 2011. Scottish Spending Review 2011 and Draft Budget 2012-13, Edinburgh: The Scottish Government.<br> | |||
<br> | |||
== Appendices == | == Appendices == | ||
Revision as of 18:36, 11 November 2012
Community Rehab COPD[edit | edit source]
Executive summary
[edit | edit source]
Background information
[edit | edit source]
Disease process[edit | edit source]
COPD describes a number of conditions including chronic bronchitis and emphysema, where people have difficulty breathing due to long term damage to their lungs. Individuals with COPD will often have a mixture of both chronic bronchitis and emphysema. COPD leads to permanent damaged airways, which causes them to become narrower making it difficult for air to go into and out of lungs (NHS). Chronic bronchitis is defined as inflammation of the bronchi, which increases muscus production in airways and thus causes obstruction whereas emphysema involves the alveoli losing their elasticity, which reduces the support of the airways causing them to narrow and trapping air in lungs during expiration. This also causes problems with oxygen delivery, which may result in increase work of breathing and shortness of breath (BLF). The pathophysiological changes that occur to the lungs depends on the nature of the patients disease.
Causes[edit | edit source]
The largest single cause of COPD is cigarette smoking (BLF). The likelihood of developing COPD increases the more the patient smokes and the longer they have been smoking (NHS). Smoking cessation will gradually reduce the patients chances of getting COPD as it slows down the process. Other potential causes of COPD:
- Exposure to air pollution
- Exposure to fumes or particles at work (ie) welding fumes or coal dust
- Alpha-1-antitrypsin deficiency, a genetic condition
Common symptoms of COPD are: cough, sputum production and shortness of breath.
Impact on QoL: [edit | edit source]
There is a large impact on quality of life in individuals living with COPD. They have decreased exercise tolerance, decreased ability to carry out activities of daily living (ADLs) and reduced income due to the patient’s ability to work (loss of productivity). A study by Willgoss et al. (2011) illustrated that many people living with COPD also suffer from anxiety, which can lead to feelings of isolation, decreased social participation and inability to carry out ADLs which all affect quality of life. A second study by Stahl et al. (2005) determined that health related quality of life (HRQL) in COPD deteriorates in parallel with lung function impairment; HRQL decreases with increasing severity of the disease. They also found that HRQL deteriorates with increasing age.
Epidemiology of COPD[edit | edit source]
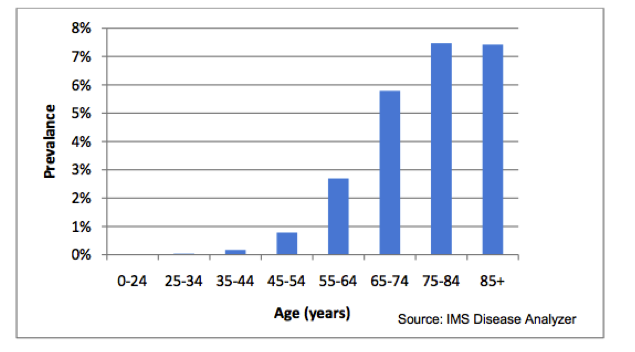
COPD is the 5th largest killer in the UK. It is the 2nd most common cause of emergency admission to hospital and it is the most costly inpatient condition treated by the NHS (ERPHO). An estimated 3 million people have COPD in the UK although approximately 2 million of this estimation remain undiagnosed (NICE). The rate of COPD in the population is estimated at between 2% and 4% and the diagnosed prevelance of COPD in England alone is 1.6% (quality and outcomes framework 2008/09). The prevalence of COPD is largely influenced by age (NICE). The diagnosed prevelance for individuals between 45-54 is < 1% which increases to > 5% for individuals aged 65+. This is depicted in Figure 1. The mortality of COPD in the UK is estimated at 23,000 people per year.
Figure 1: Estimated prevalence of diagnosed COPD by age (NICE):
Cost to NHS[edit | edit source]
NHS is currently spends approximately £1 billion annually on COPD. It costs nearly 10 times more to treat severe COPD than the mild disease (DH).
Current service and achievements[edit | edit source]
There are currently many guidelines and initiatives for COPD; NICE guidelines, British Thoracic Society guidelines, GOLD: global initiative for COPD, NHS improvement. All of these guidelines discuss the importance of smoking cessation and pulmonary rehabilitation. There is currently an NHS stop smoking service available in Lothian that offers one-to-one support. Hospital based pulmonary rehabilitation programs are also available throughout the UK.
Rationale for Change: [edit | edit source]
Pulmonary rehabilitation is an exercise program combined with educational information. It can increase an individuals exercise capacity, mobility and self-confidence leading to an increased quality of life (NHS). Exercise has been shown to slow the progression of the disease, decrease exacerbations and readmissions. Having a pulmonary rehabilitation class held in a sports facility in the community may increase adherence, as it may be more accessible and individuals may feel less anxious about a class held in a community setting as opposed to a hospital. If more people are attending pulmonary rehabilitation classes in the community it will ultimate lead to a reduction of long-term costs for the NHS:
- More people attending pulmonary rehabilitation
- Less exacerbations and readmissions
- Slowing the progress of the disease
Evidence for pulmonary rehabilitation[edit | edit source]
Eligibility for the proposed pulmonary rehabilitation program shall be in line the NICE COPD guideline (2010). This states that “pulmonary rehabilitation should be offered to all patients who feel functionally disabled by COPD” (NICE 2010).
“The opportunity for structured, on going exercise with peer and professional support, in a suitable venue, is perceived as important to people with COPD in facilitating a physically active lifestyle following pulmonary rehabilitation” (Hogg et al. 2012).
According to General Practice Airways group's sharing of best practice meeting (2005) and the American Thoracic Society/European Respiratory Society Statement on Pulmonary Rehabilitation (2006), at least one supervised session is required per week for effective pulmonary rehabilitation. It has also been suggested that two supervised sessions per week may have a better impact on health-related quality of life (Liddell and Webber 2010). Making it a regular weekly program would give the program a structure and would ensure that the participants have regular support which has been found to be important in exercise regimes, especially in this population (O'Shea et al. 2007). Therefore, to make this program as cost effective as possible, we suggest that it will contain two weekly exercise classes as a number of individual supervised rehabilitation sessions would be capital and labour intensive.
As is desirable, exercise sessions would be delivered by healthcare professionals, including a physiotherapist and physiotherapy technical instructor, both with experience in cardio-respiratory rehabilitation (Backley et al. 2005). The location of these sessions would be in the community as according to the COPD guidelines published by NICE, pulmonary rehabilitation classes should be held in locations which are easily accessed by participants to ensure their effectiveness (NICE 2010). In addition, it has been found that difficulties with transport is a barrier to completion of pulmonary rehabilitation (Keating et al. 2011). The NICE guideline also states that these are to be held at times which suit the participants (NICE 2010). These group sessions would be interspersed with exercise sessions which participants would do in their own time at home or in a local leisure facility. It is suggested that a minimum of four home sessions are completed per week (Backley et al. 2005).
As recommended by the American Thoracic Society/European Respiratory Society Statement on Pulmonary Rehabilitation (2006), a minimum of twenty exercise sessions would be included in this pulmonary rehabilitation program at a frequency of at least three per week, with one or two of these being supervised. According to the NICE COPD guideline (2010), duration of initial pulmonary rehabilitation should be between six and 12 weeks. To conform to both of these guidelines, we propose a 10 week pulmonary rehabilitation program consisting of two supervised sessions per week.
Although exercise of varied intensity has been shown to be beneficial for people with COPD, high intensity exercises would be encouraged in this rehabilitation program for greater physiological effects (Nici et al. 2006). In addition to the traditional lower limb training included in pulmonary rehabilitation, such as treadmill walking or cycling, upper limb exercises, such as arm ergometer or hand weights, will be included as a number of beneficial effects have been noted including reduce ventilator requirements while using the arms (Couser et al. 1993, Epstein et al. 1997). Ideally, the rehabilitation program would contain aerobic exercise at an intensity of between four and six on Borg dyspnoea scale or more than 60% of max workload for at least 30 minutes. For resistance exercise, between two and four sets of six to twelve repetitions at an intensity of 50-80% of 1RM (Nici et al. 2006).
In addition to the structured exercise class, an essential educational component will be included in the pulmonary rehabilitation program (Backley et al. 2005). This would include teaching participants the importance of exercise. This is of specific importance with people in this population as many individuals with COPD elect not to take up a referral to pulmonary rehabilitation as they think they would not experience any health benefits from attendance. Ensuring good attendance at pulmonary rehabilitation requires consideration of how information regarding the proven benefits of pulmonary rehabilitation can be conveyed to participants (Keating et al. 2011). It is also important to supply the participants with information on how to transfer exercise into environments outside the class, such as their home, as this will be required for between supervised sessions and once they have completed the program (Nici et al. 2006). Information on relaxation, anxiety management, medication and self management (Backley et al. 2005), including an action plan for exacerbations (Nici et al. 2006), would also be included as this seen as being essential in an effective pulmonary rehabilitation program.
Analysis of needs[edit | edit source]
SWOT[edit | edit source]
Strengths:
The location of our class will be in a location that is easy to access, increasing adherence
- The community setting of this program will, potentially, cause less anxiety for participants than hospital setting
- The setting of the program will have more available space than most hospitals thus more capacity for participants
- Since the rehabilitation program is not been run in the hospital, there is a lower chance of participants acquiring healthcare related infections
- Our program will have qualified staff including first aiders who are trained in defibrillator use
- Evidence shows that pulmonary rehabilitation gives numerous benefits to participants including improved quality of life
- There is an increasing body of evidence that pulmonary rehabilitation decreases long term costs to NHS
- The group exercise setting provides peer support which people in this population often need
- <Addresses the need for some women to exercise when men are not present?>
Weaknesses:
- Some participants may find a gym to be an intimidating setting
- Exercise is a undesirable activity for some participants, especially in people with COPD where breathlessness may be an issue
Opportunities:
- There is a large prevalence and incidence of COPD
- Increased referrals to the program will reduce demands on NHS’s limited resources
- Greater exposure of pulmonary rehabilitation in the community will increase public awareness of this treatment option
- <ADDRESSES THE NEED FOR PUL REHAB IN WOMEN?>
Threats:
- Other pulmonary rehabilitation classes:
- Some gyms run pulmonary rehabilitation classes. However, these 1 to 1 sessions with a gym instructor so there is a lack of peer and group support. In addition, this rehabilitation program will have all the material delivered by health professionals with experience in respiratory care.
- Pulmonary rehabilitation is also often held in the hospital. We feel that our program setting is less intimidating and carries fewer negative connotations. There is also the additional benefit of more car parking facilities than what is available at most hospitals.
PESTLE (political, economic, social, technological, legal environmental)[edit | edit source]
Contextual issues[edit | edit source]
[edit | edit source]
Historical Trends and Future Projections for NHS Budget Changes
[edit | edit source]
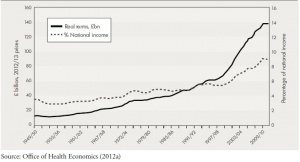
According to Crawford & Emmerson (2012), real public spending* on the NHS has increased faster than economy-wide inflation since the 1950s – from 3.5% of the national income in fiscal year 1949-1950 to 7.9% in fiscal year 2007-2008, prior to the financial crisis and subsequent recession.
The fastest rate of average growth on record was 6.4% per annum between fiscal years 1996-1997 and 2009-2010.
In the 2010 Spending Review, the UK government committed to protecting NHS funding for that year to ensure adequate healthcare delivery to UK citizens. However, a freeze for NHS spending has been planned for fiscal years 2011-2012 to 2014-2015. If implemented, it will be the tightest 4-year funding period on record for the past 50 years.
Projected total public spending cuts average at 0.9% per annum from fiscal years 2015 to 2017. Even with significant cuts in welfare spending, public services spending require average cuts of 1.7% per annum to conform to current spending plans.
For spending on public services to increase by an average of 1.1% per annum from 2014 to 2022, total public spending must increase proportionate to national income at a projected growth rate of 1.2% per annum over the same period.
As can be seen from the above, changes to NHS and other public service funding are highly dependent on the actual economic climate of a given period – if average growth dips below forecasts, the amount available for public spending will be even lower.
* Spending which has been adjusted for the effect of the general level of inflation in the economy.
In Scotland, the cur
rent spending review and latest draft budget includes plans to freeze real NHS spending between fiscal years 2012 to 2015, as can be seen from Table 7.01.
(The Scottish Government, 2011)
According to a report to the Holyrood health committee by Dr Andrew Walker of the University of Glasgow, NHS boards across Scotland have been directed to ensure 3% efficiency savings in fiscal year 2012-2013.
Greater Glasgow and Clyde region leads the pack at a savings target of £58 million, with Lothian coming second at £27 million.
Scottish Labour alleges that funding cuts have targeted mostly frontline staff, with more than 4500 NHS jobs cut since 2009, of which 2000 were nurses.
(BBC, 2012)
COPD cost to NHS and Society
[edit | edit source]
COPD – Its Costs To The NHS And Burden On Greater Society
COPD is a major contributor to healthcare costs UK-wide. It has been estimated that the number of COPD sufferers in the UK ranges between 900,000 to 1.5 million.
In 2003, the UK segment of the Confronting COPD survey estimated that the average annual direct costs per patient to the healthcare system came to £819.42, while average indirect costs – to society via paid sick leave, lost productivity, additional burden of care and so forth – come to £819.66.
COPD’s total estimated cost to the UK healthcare system in fiscal year 1996-1997 came to £817 million, while its estimated annual cost to employers and the economy was £3.8 billion or more.
UK-wide, an estimated 30,000 deaths yearly are attributable to COPD – nearly 20 times that of asthma, and 24 million working days, amounting to 9% of all certified sick leave.
More than 44% of COPD patients in the UK were found to be below retirement age at the time of the 2003 survey. 24% of all COPD patients were completely unable to work due to the disease, while 9% were limited in their ability to work and 5% had to miss work because of the disease. An estimated 4808 total workdays were lost to COPD in the 12 months preceding the survey, averaging at 12.02 days per patient.
At the time of the survey, COPD prevalence in the UK was calculated to be 5% amongst males aged 65-74 years of age, and 10% in males aged 75 years or more. Given the prevalence increase of 25% in males and 69% in females from 1990 to 1997, if this trend continues in the future or prevalence remains the same with an increasing population, the burden of COPD on the healthcare system will only inc
rease, particularly as the population ages, allowing COPD to progress to its later and more care-intensive stages.
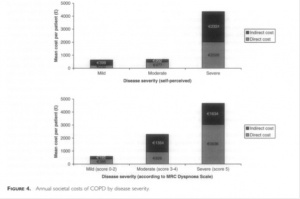
As can be seen from Figure 4, the later stages of COPD cause an across-the-board increase in direct and indirect costs, the former being attributable mostly to hospitalisation.
(Britton, 2003; Gardiner, et al., 2010; Khdour, et al., 2011)
According to Audit Scotland’s 2007 report, there are roughly 100,000 known cases of COPD in Scotland as of 2005, with a 33% increase in prevalence predicted for the next 20 years.
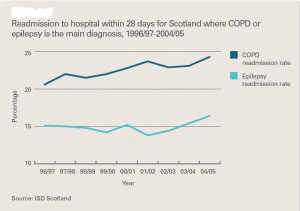
COPD is the 3rd most common reason for hospital admission in Scotland, with 19% of patients readmitted more than once and 16% at least twice more, observed from 2003-2004.
COPD’s direct per-annum cost to NHS Scotland is estimated at £100 million.
(Matthew & Diffley, 2007)
As can be seen from Exhibit 5, inpatient stays have shown a steady downward trend in duration from 1997 to 2005. However, readmission rates have been rising over the same period, as seen in Exhibit 7. From Exhibit 6, it can also be seen that, compared to epilepsy patients, COPD patients have an average longer hospitalisation stay at each category of comorbidity.
NICE COPD guidelines (National Clinical Guideline Centre, 2010')' suggest that average COPD patient per-annum costs to the NHS scale with severity accordingly:
Mild COPD: £150
Moderate COPD: £308
Severe COPD: £1307
A national average of £1036 suggests that most known patients in Scotland have fairly severe disease.
As can be seen from Exhibit 18, there is evidence for pulmonary rehabilitation potentiating large indirect savings by freeing up hospital beds for other patients by reducing inpatient stays. Although it has the highest initial setup cost of the services examined, once implemented, it is likely to pay for itself many times over in inpatient care costs saved.
(Matthew & Diffley, 2007)
National guidelines and targets
[edit | edit source]
Clinical Standards and Guidelines
The National Institute for Clinical Excellence (NICE) in its 2010 guidelines for COPD management states that pulmonary rehabilitation is evidentially sound for:
- Eliciting meaningful improvements to health-related quality of life, functional and maximum exercise capacity in COPD patients
- Reducing dyspnoea
- Decreasing total hospitalisation days and total incidences of hospitalisation required for COPD patients in the years following a comprehensive pulmonary rehabilitation versus the year prior to rehabilitation
- Cost-effectiveness in terms of cost per quality of life-adjusted year (QALY) gained versus conventional treatment.
Having a significantly greater effect on the above outcomes than bronchodilator drugs
On programme content and duration, the consensus was reached that outpatient programmes should last a minimum of 6 weeks and a maximum of 12 weeks, incorporating physical exercise, disease education, psychological and social interventions. The tendency of pulmonary rehabilitation classes to show diminishing returns in outcomes over prolonged durations (>12 weeks) and with repeat patients was noted. The evidential base for significant benefits from pulmonary rehabilitation under such circumstances is limited.
It was also recommended that referral to pulmonary rehabilitation be considered at all stages of disease progression – as soon as symptoms and disability are present and not at predetermined impairment levels.
Additionally, it was noted that patients previously hospitalised for acute COPD exacerbation showed a tendency towards significant benefits from early pulmonary rehabilitation (within 1 month post-discharge), compared to patients receiving standard care modalities or no rehabilitation during this period. Evidential quality was low in the systematic review examined, but it was determined that there was no reason why patients who had a recent COPD exacerbation should not be considered for pulmonary rehabilitation.
(National Clinical Guideline Centre, 2010)
The NHS Lothian COPD Guidelines concur broadly with the NICE 2010 Guidelines, agreeing that there is sufficient evidence that it is evidentially sound in its purported benefits to all COPD patients, and particularly those with severe to extremely severe COPD, or those scoring ≥ 3 on the Medical Research Council (MRC) breathlessness scale.
As with the NICE 2010 Guidelines, this guideline acknowledges that pulmonary rehabilitation:
- Improves exercise tolerance
- Improves Quality of Life
- Reduces symptoms
- Reduces number of exacerbations
- Reduces hospital admissions
Given that pulmonary rehabilitation is available in all Community Health Partnerships (CHPs) throughout Lothian, this guideline recommends that all patients with repeated exacerbations or who are hospitalised for exacerbations be fast-tracked for pulmonary rehabilitation.
(NHS Lothian, 2011)
NHS Quality Improvement Scotland (QIS) lists 6 dimensions of quality practice:
- Safe: avoiding iatrogenic patient harm
- Effective: providing scientifically-based service to all who could benefit, refraining from providing services to those not likely to benefit.
- Patient-centred: providing care respectful of and responsive to individual patient preferences, needs and values, ensuring that patient values guide all clinical decisions.
- Timely: reducing waits and harmful delays for both care recipients and givers.
- Efficient: avoiding waste, inclusive of equipment, supplies, ideas and energy.
- Equitable: providing care quality that does not vary due to personal characteristics such as gender, ethnicity, geographic location and socioeconomic status.
Furthermore, it also acknowledges both the benefits of pulmonary rehabilitation on COPD patients with regard to improving health-related quality of life, exercise capacity and breathlessness, particularly in the wake of acute exacerbation.
Taking into account the cost-effectiveness of pulmonary rehabilitation as estimated in Matthew & Diffley (2007) and echoed in the NICE 2010 Guidelines, it may be seen that an early post-discharge pulmonary rehabilitation programme would fulfil dimensions #1 – 5 of NHS QIS’ quality outcomes.
(NHS Quality Improvement Scotland, 2010)
Patients' Experience of Pulmonary Rehabilitation Classes[edit | edit source]
Patient A’s Story:
Back before I started at breath smart I couldn’t do a lot. I was heavily dependent on oxygen and practically house bound. I couldn’t use the stairs or do my gardening or go to the shops. I was actually wheeled into my 1st class at breath smart because I couldn’t walk far at all. I must have been in hospital 8 or 9 times the year before I started these classes. I’ve been coming twice a week for just over a year and now I don’t use any oxygen at all and I will gladly take the stairs without and trouble. I haven’t been admitted to hospital once this year. I can now use the treadmill for 25mins at a time at a speed of 5.5km/hr and an incline of 3.5. I never thought this would be possible. Breath smart has given me back my freedom I can’t begin to explain the changes it has made to my life. I am however still smoking. If I was able to improve this much while still smoking I can only imagine how much better I would be if I could give them up but I haven’t been able to as of yet.
Patient B’s Story:
Before starting breath smart I spent a lot of time in hospital, my breathing was very bad and my general health was very bad also. I used an awful lot of oxygen. Confidence was a big problem. It was hard to know what to do, that was very very difficult. I had been very very active all my life and then everything came to a standstill. My consultant suggested I come to breath smart. I’m here 2 years now, and the difference in my life is huge! I couldn’t even start to tell people how much of a difference it has made to my life, but I do tell people. My family have all seen the difference it has made to my life. I’m more active. Coming to breath smart gives you an incentive, it gives you the confidence, the people here are professional you trust them, I trust everyone here they are very very good, they explain to you and tell you if you are doing too much or doing too little. This is the 1st year that I haven’t been in hospital since I was diagnosed.
Patient C's Story
Patient D's Story
Patient E's Story
Patient F's Story
Option appraisal/Advantages and disadvantages[edit | edit source]
The British Thoracic Society issued a statement on the benefits of pulmonary rehabilitation declaring the enhancements in exercise tolerance and health related quality of life (HRQOL) in patients with chronic obstructive pulmonary disease (COPD) (Ward et al., 2002). However, a recent survey highlighted that it is only available in 25% of U.K. hospitals (Davidson and Morgan, 1998) meaning lack of availability limits the number of COPD patients that can benefit. The majorities of programs are hospital-based and include individual exercise programmes and educational talks, but a key factor is the sharing of experiences among participants and their spouses.
There are a variety of settings in which pulmonary rehabilitation services for patients with COPD can be provided. Traditionally services were based in hospital inpatient and outpatient settings, but there is growing interest in developing services in community and home settings making it easier for patients to attend and carry out. As pulmonary rehabilitation classes have been long established in hospital based settings it is the standard comparison for any other potential pulmonary rehabilitation class settings.
Location is stated as a core element in the full clinical guideline on COPD, it states that for pulmonary rehabilitation programs to be effective and to improve compliance, they should be held at times that suit patients, in buildings that are easy for patients to get to and have good access for people with disabilities (NICE, 2010). Pulmonary rehabilitation has been found to have a positive impact on lowering health care costs, mainly by reducing the number of exacerbations and hospital admissions (Guëll et al., 2008). Therefore, if more patients can take part in these pulmonary rehabilitation classes it would save the NHS money in the long term as well as improving the patient’s wellbeing.
Waterhouse et al. (2010) conducted a powered, randomized 2 x 2 trial of 240 patients comparing pulmonary rehabilitation in a hospital versus community setting, followed up by telephone or conventional follow up. They found no significant difference in the percentage change in the distance walked during the Endurance Shuttle Walk Test relative to baseline between the hospital and the community rehabilitation groups. There was also no significant difference between the groups in terms of the increase in the time that they were able to walk for post-rehabilitation. The absence of any significant differences in these outcomes continued at 6 month, 12 month and 18month follow ups. There also appeared to be no indication of an effect of telephone versus conventional follow up. An economic analysis also conducted by the authors indicated no cost advantage to either of the rehabilitation settings or to telephone follow up.
Guëll et al. (2008) demonstrates the improvement in exercise tolerance achieved by COPD patients with an unsupervised home pulmonary rehabilitation program is similar to the improvements of patients in a rigorous hospital based program. However the hospital program gave greater benefit on the HRQOL area of emotional function. Similar improvements in both exercise tolerance and symptoms (dyspnea) were accomplished with both the home and hospital programs. It can be seen that dyspnea and exercise tolerance improved in the home based program indicating compliance with the program. It could be speculated that the lack of improvement in HRQOL measurements in the unsupervised home group is down to the inadequate psychological and emotional support from the pulmonary rehabilitation staff as this was an aspect of care that was received by the hospital based group. Results indicate that home based pulmonary rehabilitation can provide an alternative to traditional programs allowing rehabilitation to be given for larger numbers of patients.
Khdour et al. (2011) undertook a cost-utility analysis of a pharmacy-led self-management programme for COPD using a single outpatient COPD clinic. A randomized controlled trial was used with participants either receiving pharmacy-led education and a self-management programme or usual care. One year costs were estimated and quality-adjusted life years were calculated based on responses to EQ-SD at baseline, 6 and 12 months. The mean differences in costs and effects between self-management and education programme and usual care was -£671.59 showing it was less costly and more effective.
Home based pulmonary rehabilitation programs have been introduced in recently, and evidence suggests that they may give similar benefits to those of hospital based rehabilitation (Guëll et al., 2008). However, much of the evidence to support home based programs used resource and exercise intensive methods that may not be feasible in some settings. Findings among the studies were similar finding no significant differences for clinical effectiveness between settings. The differences established in HRQOL scores are important and highlights the proven positive impact of group sessions.
Hospital
| Advantages | Disadvantages |
| Peer support | Difficulty parking – possible |
| No external costs, i.e. rent | Busy environment |
| Patients may deem hospital appointments more important | Lack of available, purposeful space |
| Qualified medical staff | Limited exercise equipment |
| Safe, controlled environment | May associate hospital with acute illness |
| Medical equipment available | Increased chance of contracting an infection |
| Exercise equipment available | Costly, even in outpatient setting |
| Cost comparison found most efficient form of delivery | Suffer from high drop out rates with 20% not completing the program |
| Found to be effective in improving exercise tolerance and QoL | Patients discouraged because of frequent journeys to hospital |
| Patients often have difficulty getting to a hospital |
Community
| Advantages | Disadvantages |
| Peer support | External costs i.e. rent, travel expenses, equipment, resources |
| Motivational environment encouraging compliance | Patients may want to take part more anonymously |
| Familiar, friendly atmosphere | |
| Low drop out rates | |
| Sufficient amount of exercise equipment | |
| Available, purposeful space | |
| More involved within the community | |
| Qualified physiotherapists | |
| Relaxed atmosphere so patients feel more comfortable raising questions/issues | |
| Influence patients participation in physical activity | |
| Greater choice of venue making it more accessible | |
| Local ownership |
Home
| Advantages | Disadvantages |
| Cost effective | Safety |
| No supervision | Adherence |
| Patient may feel safer and more comfortable exercising in own home | Information clear and well instructed? Patient understands and carries out correctly? |
| Can do it at time that suits patient | No supervision |
| No peer support | |
| Any issues that arise may not be addressed immediately | |
| Feasibility of resources and equipment – cost, availability | |
| Practicalities of having equipment in home i.e. space |
So when we look at all the advantages and disadvantages of each setting we can clearly see that the community setting is the outright winner with more advantages than disadvantages. While, the hospital setting appears to have a similar amount of advantages than disadvantages and the home setting appears to have more disadvantages than advantages. This again reinforces our choice of a community setting.
Community v hospital v home[edit | edit source]
So after looking at the evidence we have chosen to hold our pulmonary rehabilitation class in a community setting more specifically in a leisure centre. Evidence proved pulmonary rehabilitation provided in a community setting has comparable benefits to that produced in a more customary hospital-based setting, with both settings producing significant improvements in exercise capacity and quality of life (Maltais et al., 2008: Guell et al., 2008: Waterhouse et al., 2010). The choice of venue has been found to be determined by local factors of convenience, current availability of resources and incremental costs as supported by Waterhouse et al. (2010). The rationale for the choice of venue is multifaceted as the sports equipment such as treadmills and exercise bikes are within the centre and there is plenty of purposeful space to utilise. With the class being out width a clinical setting it has a more relaxed atmosphere free from the negative thoughts and feeling commonly associated with a hospital environment as identified by Slovic et al. (2004). The chances of patients already having visited a local venue helps reduce anxiety as they are familiar with their surroundings. Those taking part in the classes will also benefit from the support and encouragement of meeting local people with the same condition (Ward et al. 2002: Guell et al., 2008). With a sports centre there is a motivational atmosphere as those there are investing in themselves either to be fitter, healthier, look better or to perform better which will influence the patient’s attitude. By influencing the patient’s awareness this will encourage compliance, influence participation in physical activity as well as allowing the patients to become more involved in the community, as many sports centres have notice boards in their reception areas alerting people to other opportunities. Staff characteristics may play a vital role in achieving best possible outcomes so care is required when recruiting and training staff (Ward et al., 2002: Waterhouse et al., 2010). When health economic analysis was considered by Waterhouse et al. (2010) it revealed that neither hospital nor community based programmes were preferential. We found when we looked at the advantages and disadvantages of each setting we found that there were no advantages to using a hospital and many more disadvantages to a home setting while the community setting had far more advantages than disadvantages supporting our choice to use a community setting. When comparing hospital, community and home settings there were no clinical differences however the benefits of having the class in a community setting aided attendance and compliance helping not only patients but in the long run saving the NHS money by preventing exacerbations and reducing hospital admissions.
Evidence suggests that there appears to be no clinical or cost benefit of community based pulmonary rehabilitation programs over hospital based pulmonary rehabilitation and that the venue may be best determined by local access preferences and transport links. This evidence therefore reinforces current recommendations in NICE CG101 (Nice, 2010). So, our choice to hold our pulmonary rehabilitation classes in a community setting has been found to benefit the patients and the budget as supported by the evidence and may be more successful as it takes into consideration other influences on patient’s ability to attend.
Proposed class structure[edit | edit source]
Financing[edit | edit source]
Fixed Expenses:
Below is a table indicating the fixed costs of the “insert name” class by year and by month.
Table 4: Fixed Expenses
| Expenses | Yearly | Monthly |
| Venue | 3600 | 300 |
| Staff (Band 5 Physiotherapist) | 2027.52 | 168.96 |
| Staff (Physiotherapist Assistant) | 1110.24 | 92.52 |
| Personal Indemnity Insurance | Covered by CSP Membership | Covered by CSP Membership |
| Total | £6737.76 | £561.48 |
To calculate the staffing costs we used the following stepped equation:
1. Number of workable hours per year
- Number of weeks per year X hours worked per week
- 52 X 37.5= 1950
2. Number of hours worked per year
- Number of workable hours per year– (Holiday + bank holiday hours)
- 1950 – [(27 X 7.5) + (8 X 7.5)]
- 1950 – (203 + 60)
- 1950 – 263
- 1687
3. Cost per hour for staff
- (Salary + Employers Contribution to National Insurance [13.08% for 2012-2013]) ÷ Hours worked per year
- Physiotherapist = 21,000 + 2750= 22750, 22750 ÷ 1687 = 14.08.
- Physiotherapist Assistant= 11500 + 1504.2 = 13004.2, 13004.2 ÷ 1687 = 7.71
4. Monthly Cost
- Cost per hour X hours per week X hours per month
- 2 class per week @ 1hr each plus 15mins pre and post = 3hrs per week
5. Yearly Cost
- monthly cost X 12
Variable Expenses:
Below is a table indicating the variable costs of the “insert name” class by year and by month.
Table 5: Variable Expenses
| Expenses | Once off | Yearly | Monthly |
| Stationary | |||
| Printer | 49.99 | 16.66 | 1.39 |
| Tea and Coffee | 96 | 8 | |
| Paper Cups | 48 | 4 | |
| Plastic Spoons | 24 | 2 | |
| Milk | 96 | 8 | |
| Total | £49.99 | £340.68 | £28.39 |
The cost of the printer was worked out as follows:
1. Yearly cost
- Cost of printer (priced at PC World) ÷ 3 (estimated minimal life expectancy)
2. Monthly cost
- Yearly cost ÷ months per year
Capital Expenses:
Below is a table indicating the capital costs of the “insert name” class by year and by month.
Table 6: Capital Expenses
| Expenses | Once Off | Yearly | Monthly |
| Blood Pressure Monitor X 4 | 160 | 53.33 | 4.44 |
| Pulse Oximeter | 198 | 66 | 5.50 |
| Total | £358 | £119.33 | £9.94 |
The cost of all capital equipment was worked out as follows:
1. Three quotes were explored and the average cost was taken
2. Yearly Cost
- Cost of item ÷ 3 (estimated minimal life expectancy)
3. Monthly cost
- Yearly cost ÷ months per year
Overhead Cost:
Fixed Expenses + Variable Expenses
Yearly overheads = £7078.44
Monthly overheads = £589.87
Starting Up Costs:
Capital expenses + 1st 3 month’s overheads
358 + (589.87 X 3)
358 + 1769.61
£2127.61
Cost of Service per participant:
(Overhead costs + Capital expenses) ÷ Number of participants
Yearly
(7078.44 + 119.33) ÷ 16
£449.86 per participant per year
Monthly
(589.87 + 9.94) ÷ 16
£37,49 per participant per year
Risk analysis[edit | edit source]
H & S[edit | edit source]
Conclusions[edit | edit source]
Outcome measures[edit | edit source]
References[edit | edit source]
Backley, J., Bloom, J., Bott, J., Jones, R., Langley, C., Singh, S., Smith, J. and Till, J. 2005. A Summary of Recommendations of the Pulmonary Rehabilitation in Thecommunity- Sharing Best Practice Meeting. General Practice Airways Group pp.30/10/12. Available at: http://www.pcrs-uk.org/resources/gpiag_pul_rehab_bestpract_200306.pdf [Accessed 30/10/12].
Couser, J.I., Martinez, F.J. and Celli, B.R. 1993. Pulmonary rehabilitation that includes arm exercise reduces metabolic and ventilatory requirements for simple arm elevation. CHEST Journal, 103 (1) January 1, pp.37-41.
Epstein, S.K., Celli, B.R., Martinez, F.J., Couser, J.I., Roa, J., Pollock, M. and Benditt, J.O. 1997. Arm training reduces the VO2 and VE cost of unsupported arm exercise and elevation in chronic obstructive pulmonary disease. Journal of cardiopulmonary rehabilitation, 17 (3) May-Jun, pp.171-177.
Hogg, L., Grant, A., Garrod, R. and Fiddler, H. 2012. People with COPD perceive ongoing, structured and socially supportive exercise opportunities to be important for maintaining an active lifestyle following pulmonary rehabilitation: a qualitative study. Journal of Physiotherapy, 58 (3) 9, pp.189-195.
Keating, A., Lee, A.L. and Holland, A.E. 2011. Lack of perceived benefit and inadequate transport influence uptake and completion of pulmonary rehabilitation in people with chronic obstructive pulmonary disease: a qualitative study. Journal of Physiotherapy, 57 (3) 9, pp.183-190.
Liddell, F. and Webber, J. 2010. Pulmonary rehabilitation for chronic obstructive pulmonary disease: a pilot study evaluating a once-weekly versus twice-weekly supervised programme. Physiotherapy, 96 (1) 3, pp.68-74.
NICE. 2010. Chronic obstructive pulmonary disease, Management of chronic obstructive pulmonary disease in adults in primary and secondary care (partial update). NICE Clinical Guidelines, 101 (June) pp.1-61.
Nici, L., Donner, C., Wouters, E., Zuwallack, R., Ambrosino, N., Bourbeau, J., Carone, M., Celli, B., Engelen, M., Fahy, B., Garvey, C., Goldstein, R., Gosselink, R., Lareau, S., MacIntyre, N., Maltais, F., Morgan, M., O'Donnell, D., Prefault, C., Reardon, J., Rochester, C., Schols, A., Singh, S., Troosters, T. and on behalf of the ATS/ERS Pulmonary Rehabilitation Writing Committee. 2006. American Thoracic Society/European Respiratory Society Statement on Pulmonary Rehabilitation. American Journal of Respiratory and Critical Care Medicine, 173 (12) June 15, pp.1390-1413.
O'Shea, S.D., Taylor, N.F. and Paratz, J.D. 2007. [horizontal ellipsis]But Watch Out for the Weather: FACTORS AFFECTING ADHERENCE TO PROGRESSIVE RESISTANCE EXERCISE FOR PERSONS WITH COPD. Journal of Cardiopulmonary Rehabilitation & Prevention, 27 (3) May/June, pp.166-174.
British Thoracic Society. Standards of care committee on pulmonary rehabilitation. 2001. Thorax, 56, pp.827-834.
Davidson, A.C. and Morgan, M.D.L. 1998. A UK survey of the provision of pulmonary rehabilitation. Thorax, 53, pp. 86.
Guëll, M.R., Lucas, P., Gáldiz, J.B., Montemayor, T., González-Moro, J.M.R., Gorostiza, A., Ortega, F., Bellón, J.M. and Guyatt, G. 2008. Home vs hospital-based pulmonary rehabilitation for patients with chronic obstructive pulmonary disease: A Spanish multicenter trial. Archive Bronconeumol, 44 (10), pp.512-518.
Khdour, M.R., Agus, A.M., Kidney, J.C., Smyth, B.M., Elnay, J.C. and Crealey, G.E. 2011. Cost-ultility analysis of a pharmacy-led self-management programme for patients with COPD. International Journal of Clinical Pharmacy, 33, pp. 665-673.
Lacasse, Y., Goldstein, R., Lasserson, T.J. and Martin, S. 2006. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Systematic Review, CD003793.
Maltais, F., Bourbeau, J., Shapiro, S., Lacasse, Y., Perrault, H., Baltzan, M., Hernandez, P., Rouleau, M., Julien, M., Parenteau, S., Paradis, B., Levy, R.D., Camp, P., Lecours, R., Audet, R., Hutton, B., Penrod, J.R., Picard, D. and Bernard, S. 2008. Effects of home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease. Annals of Internal Medicine, 149, pp.869-878.
Strijbos, J.H., Postma, D.S., van Altena, R., Gimeno, F. and Koëter, G.H. 1996. A comparison between an outpatient hospital-based pulmonary rehabilitation program and a home-care pulmonary rehabilitation program in patients with COPD. A follow up of 18 months. Chest, 109, pp. 366-372.
Ward, J.A., Akers, G., Ward, D.G., Pinnuck, M., Williams, S., Trott, J. and Halpin, D.M.G. 2002. Feasibility and effectiveness of a pulmonary rehabilitation programme in a community hospital setting. British Journal of General Practice, 52, pp.539-542.
Waterhouse, J.C., Walters, S.J., Oluboyede, Y. and Lawson, R.A. 2010. A randomized 2 x 2 trial of community versus hospital pulmonary rehabilitation for chronic obstructive pulmonary disease followed by telephone or conventional follow-up. Health Technology Assessment, 14, pp.1-164.
Slovic, P., Finucane, M.L., Peters, E. and MacGregor, D.G. 2004. Risk as analysis and risk as feelings: some thoughts about effect, reason, risk and rationality. Risk Analysis, 24 (2), pp.311-322.
BBC, 2012. commmissioningsuccess.com. [Online]
Available at: http://commissioningsuccess.com/2012/07/nhs-budget-squeeze-could-last-a-decade/
[Accessed 20th October 2012].
Britton, M., 2003. The burden of COPD in the UK: results from the Confronting COPD survey. Respiratory Medicine, 97(Supplement C), pp. S71-S79.
Gardiner, C. et al., 2010. Exploring the care needs of patients with advanced COPD: An Overview of the literature. Respiratory Medicine, Volume 104, pp. 159-165.
Crawford, R. & Emmerson, C., 2012. NHS and social care funding: the outlook to 2021/22, s.l.: Institute for Fiscal Studies.
Matthew, J. & Diffley, M., 2007. Managing Long-term Conditions, Edinburgh: Audit Scotland.
NHS Lothian, 2011. Chronic Obstructive Pulmonary Disease Guideline, Edinburgh: NHS Lothian.
NHS Quality Improvement Scotland, 2010. Healthcare Improvement Scotland COPD services - Clinical Standards, Edinburgh: NHS Quality Improvement Scotland.
The Scottish Government, 2011. Scottish Spending Review 2011 and Draft Budget 2012-13, Edinburgh: The Scottish Government.
Appendices[edit | edit source]
Appendix 1 - Sample pre-exercise health check sheet[edit | edit source]
File:Pre-exercise health check.pdf
Appendix 2 - Sample exercise recording sheet[edit | edit source]
Appendix 3 - Rate of preceived dyspoena[edit | edit source]
File:Rate of Perceived Dyspnea.pdf
Appendix 4 - Measure outcome for Quality of life[edit | edit source]