Evidence-Based Upper Extremity Thrust Manipulation: Difference between revisions
No edit summary |
No edit summary |
||
| Line 121: | Line 121: | ||
*Intervention | *Intervention | ||
'''+''' Lateral Thrust Manipulation of Humeroulnar Joint | |||
Patient lying in supine position. Grasp distal medial humerus proximal to humeroulnar joint with one hand. Support proximal radius, immediatley distal to the humeroulnar joint with the other hand. Thrust manipulation performed at humeroulnar barrier by hand on distal humerus moving in a medial to lateral direction. | Patient lying in supine position. Grasp distal medial humerus proximal to humeroulnar joint with one hand. Support proximal radius, immediatley distal to the humeroulnar joint with the other hand. Thrust manipulation performed at humeroulnar barrier by hand on distal humerus moving in a medial to lateral direction. | ||
+ Palmar Thrust Manipulation of Triquetrum on Hamate | |||
Patient in seated position. Grasp patient's wrist with their palm down. Stabilize the hamate palmarly with both index fingers, one over top of the other. Place thumbs over the patient's triquetral on the dorsum of the wrist. Patient asked to gently lean back, producitng a small amount of traction through the carpals. While maintaining slight wrist flexion, thumbs exert a downward pressure in a palmar direction to the triquetral. | Patient in seated position. Grasp patient's wrist with their palm down. Stabilize the hamate palmarly with both index fingers, one over top of the other. Place thumbs over the patient's triquetral on the dorsum of the wrist. Patient asked to gently lean back, producitng a small amount of traction through the carpals. While maintaining slight wrist flexion, thumbs exert a downward pressure in a palmar direction to the triquetral. | ||
| Line 131: | Line 131: | ||
*Results | *Results | ||
'''+''' After the first visit: | |||
- Immediate relief of elbow pain following lateral thrust manipulation of humeroulnar joint. | |||
- Pain-free wrist extension and ulnar deviation following the palmar thrust manipulation of triquetrum on hamate. | |||
- Full and pain-free elbow flexion and supination was attained. | |||
- Lateral glide of humeroulnar joint was restored. | |||
- Normalized mobility of the carpals was attained. | |||
'''+''' After the 5th (final) visit: | |||
- Negative elbow flexion test, negative ULTT, carpal and humeroulnar joint mobility WNL, 0.10 on numeric pain rating scale.<br> | |||
= [http://www.physio-pedia.com/Carpel_Tunnel_Syndrome Carpal Tunnel Syndrome] = | = [http://www.physio-pedia.com/Carpel_Tunnel_Syndrome Carpal Tunnel Syndrome] = | ||
Revision as of 02:23, 11 November 2013
Introduction [edit | edit source]
Manipulation is a manual technique often used in physical therapy as an adjunctive treatment for a variety of musculoskeletal pathologies. However, quality research and evidence-based practice recommendations are extremely lacking with regard to thrust manipulation of the upper extremity. The purpose of this literature review was to help clinicians identify upper extremity pathologies for which thrust manipulation is supported by research.
Evidence Summary Table [edit | edit source]
| Author (Year) | Level of Evidence | Pathology | Upper Extremity Manipulation(s) Performed |
| Struijs et al. (2003)[1] | 1b | Lateral Epicondylitis |
|
| Nagrale et al. (2009)[2] | 1b | Lateral Epicondylitis |
|
| Goyal et al. (2013)[3] | 1b | Lateral Epicondylitis |
|
| Kearns et al. (2012)[4] | 4 | Cubital Tunnel Syndrome |
|
| Sucher BM (1994)[5] | 1b |
Carpal Tunnel Syndrome |
|
| Siu et al. (2012)[6] | 5 |
Carpal Tunnel Syndrome |
|
Lateral Epicondylitis [edit | edit source]
Struijs et al. (2003)
[edit | edit source]
- Intervention
+ Wrist manipulated from neutral position to maximal extension
- Results
+ Following 3 weeks of treatment
- 62% of patients receiving thrust manipulation reported being "much improved or "completely improved"
- Only 20% of the control group achieved these outcomes
- Manipulation of the wrist might have additional treatment effects compared with ultrasound, friction massage, and muscle stretching and strengthening exercises for management of lateral epicondylitis over the short term
Nagral et al. (2009)[edit | edit source]
- Intervention
+ Cyriax physiotherapy (deep tendon massage + Mill's manipulation) vs. Phonophoresis
- Results
+ Following 4 weeks of treatment
- 26% increase in function on the Tennis Elbow Function Scale
- pain-free grip improved 25% more with elbow manipulation compared to phonophoresis and exercise group
- Cyriax physiotherapy was found to provide a superior benefit in terms of pain, pain-free grip, and functional status when compared to a treatment regimen consisting of phonophoresis with supervised exercise and static stretching. The long-term effects of treatment remain unknown past 8 weeks.
- Intervention
+ Cyriax Physiotherapy (Mills manipulation and deep transverse friction massage) vs. Wrist Manipulation (scaphoid)
- Results
+ Following 3 weeks of treatment:
- Both the Cyriax group and the wrist manipulation group improved.
- Pain reduction favored the wrist manipulation group (47% reduction vs. 26% reduction with Cyriax).
- Grip strength improvements favored the wrist manipulation group (24% increase vs. 12% increase with Cyriax).
Cubital Tunnel Syndrome[edit | edit source]
Kearns et al. (2012) [edit | edit source]
- Intervention
+ Lateral Thrust Manipulation of Humeroulnar Joint
Patient lying in supine position. Grasp distal medial humerus proximal to humeroulnar joint with one hand. Support proximal radius, immediatley distal to the humeroulnar joint with the other hand. Thrust manipulation performed at humeroulnar barrier by hand on distal humerus moving in a medial to lateral direction.
+ Palmar Thrust Manipulation of Triquetrum on Hamate
Patient in seated position. Grasp patient's wrist with their palm down. Stabilize the hamate palmarly with both index fingers, one over top of the other. Place thumbs over the patient's triquetral on the dorsum of the wrist. Patient asked to gently lean back, producitng a small amount of traction through the carpals. While maintaining slight wrist flexion, thumbs exert a downward pressure in a palmar direction to the triquetral.
- Results
+ After the first visit:
- Immediate relief of elbow pain following lateral thrust manipulation of humeroulnar joint.
- Pain-free wrist extension and ulnar deviation following the palmar thrust manipulation of triquetrum on hamate.
- Full and pain-free elbow flexion and supination was attained.
- Lateral glide of humeroulnar joint was restored.
- Normalized mobility of the carpals was attained.
+ After the 5th (final) visit:
- Negative elbow flexion test, negative ULTT, carpal and humeroulnar joint mobility WNL, 0.10 on numeric pain rating scale.
Carpal Tunnel Syndrome[edit | edit source]
Sucher BM (1994)[edit | edit source]
- History and physical examination along with electrodiangostic results were positive for carpal tunnel syndrome.
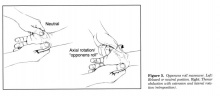
- Patients received osteopathic manipulative treatment with the “opponens roll” maneuver and self-stretching.
+ Thumb is brought into "retroposition"
- combination of aduction and extension with the added component of lateral rotation along the axis of the first metacarpal bone.
- The high velocity lateral rotation of the thumb introduces substantial traction of muscle attachment of the opponens pollicis muscles which blends into the flexor retinaculum.
- distal edge of ligament “lifts up” ventrally off median nerve and relieves direct pressure
- stretches muscle and ligament at same time and take pressure off nerve
+ Those who were treated in this manner improved clinically with a decrease in both symptoms and palpatory restriction.
Siu et al. (2012)
[edit | edit source]
- Opponens roll maneuver: This maneuver involves lateral and axial rotation of the thumb, which creates substantial traction on the attachment of the opponens pollicis muscle. The muscle originates from the transverse carpal ligament and tubercle of the trapezium bone. This maneuver stretches the muscle and transverse carpal ligament, releasing pressure within the carpal tunnel and unloading pressure on the median nerve
- The technique is performed by grasping the hypothenar region of the patient and then using his or her other hand to grasp the patient's thenar area. The patient's thenar area is gradualy pulled laterally while simultaneously moving the thumb into extension to create traction. In addition, the abductor pollicis brevis is extended and abducted. A progressive phase of stretch further extends and abducts the opponens and abductor muscles.This technique is especially useful as patients can be educated on how to self-perform the opponens roll maneuver by using the contralateral hand to grasp and extend the thumb.
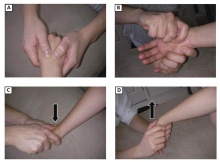
- Carpal Bone: High-velocity, low-amplitude technique (mobilization with impulse)— (A) The clinician's hands grasp the patient's hand and wrist. (B) The clinician's index fingers grasp the anterior aspect of the carpal bones. (C) A dorsiflexion barrier is engaged, and the clinician applies a mobilization with impulse thrust moving the patient's wrist toward the floor in a whipping motion. (D) A palmar flexion barrier is engaged, and the physician applies a mobilization with impulse thrust by moving the patient's wrist in the opposite direction.
- Metacarpophalangeal and Carpometacarpal Joints: High-velocity, low-amplitude technique (mobilization with impulse)— (A) The clinician grasps an individual phalanx with his or her index fingers and palm. Traction is then applied to the metacarpophalangeal joint and a mobilization with impulse thrust is applied distally in an axial manner. (B) With the clinician's thumb contacting the dorsal aspect of an individual metacarpal, the index fingers grasp the dorsal aspect of the metacarpal. Mobilization occurs by gently applying a downward force with the thumb until a barrier is engaged and subsequently applying an upward force with the index fingers.
- Posterior radial head dysfunction: High-velocity, low-amplitude technique (mobilization with impulse) —The clinician places his or her thenar eminence on the patient's posterior radial head using his or her index fingers to grasp the patient's medial elbow. The patient's forearm is then rotated into supination until the restrictive barrier is reached. The forearm is then extended and a mobilization with impulse thrust is applied with the thenar eminence.
References
[edit | edit source]
1. Struijs P, Damen PJ, Bakker E, Blankevoort L, Assendelft W, Dijk CN. Manipulation of the Wrist for Management of Lateral Epicondylitis: A Randomized Pilot Study. Phys Ther 2003; 83(7):608-616.
2. Nagrale AV, Herd CR, Ganvir S, Remteke G. Cyriax physiotherapy versus phonophoresis with supervised exercises in subjects with lateral epicondylagia: a randomized clinical trial. J Man Manip Ther. 2009; 17(3): 171-8.
3. Goyal M, Kumar A, Monga M, Moitra M. Effect of Wrist Manipulation & Cyriax Physiotherapy Training on Pain & Grip Strength in Lateral Epicondylitis Patients. J Ex Sci Physiother. 2003; 9(1): 17-22.
4. Kearns G, Sharon W. Medical diagnosis of cubital tunnel syndrome ameliorated with thrust manipulation of the elbow and carpals. J Man Manip Ther. 2012; 20(2): 90-95.
5. Sucher BM. Palpatory diagnosis and manipulative management of carpal tunnel syndrome. J Am Osteopath Assoc. 1994; 94(8): 647-63.
6. Siu G, Jaffe JD, Rafique M, Weinik MM. Osteopathic Manipulative Medicine for Carpal Tunnel Syndrome. J Am Osteopath Assoc. 2012; 112(3): 127-139.
- ↑ Struijs P, Damen PJ, Bakker E, Blankevoort L, Assendelft W, Dijk CN. Manipulation of the Wrist for Management of Lateral Epicondylitis: A Randomized Pilot Study. Phys Ther 2003; 83:608-616.
- ↑ Nagrale AV, Herd CR, Ganvir S, Remteke G. Cyriax physiotherapy versus phonophoresis with supervised exercises in subjects with lateral epicondylagia: a randomized clinical trial. J Man Manip Ther. 2009; 17(3): 171-8.
- ↑ Goyal M, Kumar A, Monga M, Moitra M. Effect of Wrist Manipulation &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Cyriax Physiotherapy Training on Pain &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Grip Strength in Lateral Epicondylitis Patients. J Ex Sci Physiother. 2003; 9(1): 17-22.
- ↑ Kearns G, Sharon W. Medical diagnosis of cubital tunnel syndrome ameliorated with thrust manipulation of the elbow and carpals. J Man Manip Ther. 2012; 20(2): 90-95.
- ↑ Sucher BM. Palpatory diagnosis and manipulative management of carpal tunnel syndrome. J Am Osteopath Assoc. 1994; 94(8): 647-63.
- ↑ Siu G, Jaffe JD, Rafique M, Weinik MM. Osteopathic Manipulative Medicine for Carpal Tunnel Syndrome. J Am Osteopath Assoc. 2012; 112(3): 127-139.