Hemiplegia: Difference between revisions
(edit) |
(edit) |
||
| Line 114: | Line 114: | ||
==== CRANIAL NERVE INTEGRITY ==== | ==== CRANIAL NERVE INTEGRITY ==== | ||
The therapist examines for facial sensation (CN 5) , facial movements (CN 5 and 7), and labrynthine / auditory function (CN 8 ) . The presence of swallowing and drooling necessitates an examination of the motor nuclei of the lower brainstem cranial nerves (CN 9 , 10 and 12) affecting the muscles of the face , tongue , pharynx and larynx. The visual system should be carefully investigated , including tests for visual field defects (CN 2 , optic radiation , visual cortex ), acuity (CN 2 ) ,Pupillary reflexes (CN 2 and 3 ) and extraocular movements (CN 3 , 4 and 6). | The therapist examines for facial sensation (CN 5) , facial movements (CN 5 and 7), and labrynthine / auditory function (CN 8 ) . The presence of swallowing and drooling necessitates an examination of the motor nuclei of the lower brainstem cranial nerves (CN 9 , 10 and 12) affecting the muscles of the face , tongue , pharynx and larynx. The visual system should be carefully investigated , including tests for visual field defects (CN 2 , optic radiation , visual cortex ), acuity (CN 2 ) ,Pupillary reflexes (CN 2 and 3 ) and extraocular movements (CN 3 , 4 and 6). | ||
==== SENSATION ==== | |||
Specific localization areas of dysfunction are common with cortical lesions , whereas diffuse involvement throughout one side of the body suggests deeper lesions involving the thalamus and adjacent structures. Impairment in touch sensation (64% to 94%), proprioception (17%to 52%) , vibration (44%) and loss of pinprick sensation (35% to 71%) have been reported. Symptoms of crossed anesthesia (ipsilateral facial impairments with contralateral trunk and limb involvement ) typify brainstem lesions. | |||
A sensory examination should include testing of superficial sensations (touch , temperature , pressure , sharp or dull discrimination ) and deep sensations (proprioception ,kinesthesia , vibration ). Combined cortical sensation such as stereognosis , tactile localization , two point discrimination , texture recognition should also be examined . Comparison with the intact side should bee viewed with caution because impairment may exist in the supposedly "normal" extremities due to aging and co- morbidities. | |||
==== FLEXIBILITY AND JOINT INTEGRITY ==== | |||
An examination of joint flexibility should include passive ROM using a goniometer , joint hypermobility/hypomobility , and soft tissue changes (swelling ,inflammation or restriction). The shoulder and wrist should be examined closely because joint malalignment problems are common. Edema of the wrist often produces malaligned carpal bones with resulting impingement during wrist extension. Active ROM may be limited or impossible for the patient in early or middle recovery in the presence of paresis , spasticity , or obligatory synergies that can preclude isolated voluntary movements. | |||
Contractures can develop anywhere but are particular apparent in the paretic limbs. As contractures progress , edema and pain may develop and further restrict mobility . In the UE ,limitations in the shoulder motion of flexion , abduction and external rotation are common. Contractures are likely in the elbow and finger flexors , and forearm pronators. In the LE , plantarflexion contractures are common. | |||
==== MOTOR FUNCTION ==== | |||
===== TONE ===== | |||
Flaccidity is present immediately | |||
Revision as of 05:09, 12 March 2018
INTRODUCTION -[edit | edit source]
Paralysis of one side of the body due to Pyramidal tract lesion at any point from its origin in the cerebral cortex down to the fifth Cervical segment ( beginning of origin of cervical plexus ) .
ETIOLOGY[edit | edit source]
VASCULAR - Cerebral hemorrhage , Stroke , Diabetic Neuropathy.
INFECTIVE - Encephalitis , Meningitis , Brain abscess.
NEOPLASTIC - Glioma - meningioma
DEMYLINATION - Disseminated sclerosis , lesions to the Internal capsule .
TRAUMATIC - Cerebral lacerations , Subdural Hematoma . Rare cause of hemiplegia is due to local anaesthsia injections given intra arterially rapidly , instead of given in a nerve branch .
CONGENITAL - Cerebral palsy
DISSEMINATED - Multiple Sclerosis
PSYCHOLOGICAL - Parasomnia (Nocturnal hemiplegia ).
MECHANISM -[edit | edit source]
Damage to the corticospinal tract leads to the injury on the opposite side of the body. This happens because the motor fibres of the corticospinal tract , which take origin from the motor cortex in brain , cross to the opposite side in the lower part of medulla oblongata and then descend down in spinal cord to supply their respective muscles.
Depending on the site of lesion in brain , the severity of hemiplegia varies.
- INTERNAL CAPSULE -
Dense and uniform Hemiplegia ( UMN Facial )
Hemisensory blunting
Homonymous hemianopia
- CORTEX -
Non dense non uniform weakness
Monoplegia
Cortical signs ( Dysphasia , Apraxia , Cortical sensory loss , Convulsions )
- SUBCORTEX -
Pattern of weakness similar to cortical
- BRAINSTEM -
Crossed hemiplegia
Ipsilateral LMN CN Palsy and contralateral hemiplegia
Cerebellar signs.
- MIDBRAIN -
Crossed cerebellar ataxia with Ipsilateral Third nerve palsy ( Claude `s syndrome )
Weber`s syndrome - Third nerve palsy and contralateral hemiplegia
Contralateral hemiplegia - Cerebral peduncle
Contralateral rhythmic , ataxic action tremor ; rhythmic postural or holding tremor (rubral tremor)
- PONS -
LMN Facial and contralateral hemiplegia
Fifth nerve and contralateral hemiplegia
Lateral Gaze palsy and contralateral hemiplegia
- MEDULLA - Lateral medullary syndrome
Same side ( Horner `s syndrome , Loss of pain and touch on the face , Cerebellar signs , Palate weakness )
Opposite side ( Loss of pain and temperature sensation on the body and limbs )
- MEDULLA - Medial medullary syndrome
Same side ( wasting and weakness of the tongue )
Opposite side ( hemiplegia without facial palsy )
- SPINAL CORD -
Rare
No facial
Brown sequard Syndrome
MEDICAL DIAGNOSIS[edit | edit source]
HISTORY AND EXAMINATION[edit | edit source]
An accurate history profiling the timing of neurological events is obtained from the patient or from family members in the case of the unconscious or noncommunicative patient . Of particular importance are the exact time and pattern of symptom occurs . The most common , slowest in hours , wakes up in the morning with weakness , history of TIA , old age is typical with thrombosis . An embolus occurs rapidly with no warning , history of heart disease , younger age group , no progression (maximum deficit occurs at onset) . An abrupt onset with worsening symptoms , history of prolonged hypertension , severe headache described as "worst headache of my life " , altered consciousness , convulsions , vomiting is suggestive of haemorrhage. The patient 's past history , including episodes of TIAs or head trauma , presence of major or minor risk factors and medications , pertinent family history and recent alterations in patient function ( either transient or permanent ) are thoroughly investigated.
The physical examination of the patient includes an investigation of vital signs ( heart rate , respiratory rate , blood pressure , clubbing ) , signs of cardiac decompensation, and function of the cerebral hemispheres , cerebellum , cranial nerves , eyes and sensorimotor system.
OUTCOME MEASURES[edit | edit source]
Dynamic Gait Index, the 4-item Dynamic Gait Index, and the Functional Gait Assessment show sufficient validity, responsiveness, and reliability for assessment of walking function in patients with stroke undergoing rehabilitation, but the Functional Gait Assessment is recommended for its psychometric properties[7].
Chedoke-McMaster Stroke Assessment
Chedoke Arm and Hand Activity Inventory
CRS-R Coma Recovery Scale Revised is used to assess patients with a disorder of consciousness, commonly coma.
Take a look at our Stroke Outcome Measures Overview for more information
CEREBROVASCULAR IMAGING[edit | edit source]
Cerebrovascular imaging is the main tool to establish the diagnosis of suspected hemiplegia. Advanced neuroimaging can rapidly indentify the occluded artery and estimate the size of the core and the penumbra.
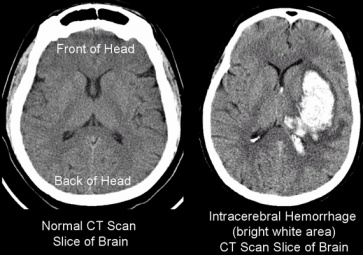
COMPUTER TOMOGRAPHY
Acute bleeding and hemorrhagic transformation are visible on CT scanning . In the subacute phase CT scan can delineate the development of cerebral edema (within 3 days) , which then fades over the next 2 to 3 weeks. Cerebral infarction (within 3 to 5 days) is visible with the addition of contrast material by showing areas of decreased density. Long term parenchymal changes consistent with scar formation are also visible on CT.
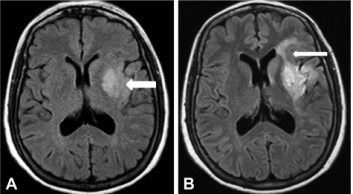
MAGNETIC RESONANCE IMAGING
MRI is more sensitive in the diagnosis of acute stroke , allowing detection of cerebral ischemia as early as 30 minutes after vascular occlusion and infarction within 2 to 6 hours. It is also able to detail the extent of infarction or haemorrhage and can detect smaller lesion than a CT scan . Use of contrast enhancement allows documentation of changes in an infarct over the first 2 to 3 weeks.
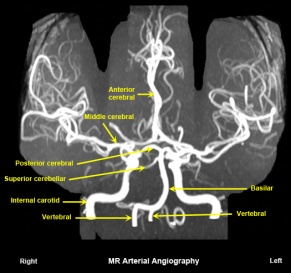
MAGNETIC RESONANCE ANGIOGRAPHY
Magnetic resonance angiography (MRA) is a type of magnetic resonance image that uses special software to create an image of the arteries in the brain. It is used to identify vascular abnormalities (e.g.,stenosis) and alterations in blood flow as a result of embolus or thrombosis.
EXAMINATION[edit | edit source]
The selection of examination procedures will vary based on a number of factors including patient age , location and severity of stroke , stage of recovery , data from initial screenings , phase of rehabilitation and home /community / work situation , as well as other factors.
CRANIAL NERVE INTEGRITY[edit | edit source]
The therapist examines for facial sensation (CN 5) , facial movements (CN 5 and 7), and labrynthine / auditory function (CN 8 ) . The presence of swallowing and drooling necessitates an examination of the motor nuclei of the lower brainstem cranial nerves (CN 9 , 10 and 12) affecting the muscles of the face , tongue , pharynx and larynx. The visual system should be carefully investigated , including tests for visual field defects (CN 2 , optic radiation , visual cortex ), acuity (CN 2 ) ,Pupillary reflexes (CN 2 and 3 ) and extraocular movements (CN 3 , 4 and 6).
SENSATION[edit | edit source]
Specific localization areas of dysfunction are common with cortical lesions , whereas diffuse involvement throughout one side of the body suggests deeper lesions involving the thalamus and adjacent structures. Impairment in touch sensation (64% to 94%), proprioception (17%to 52%) , vibration (44%) and loss of pinprick sensation (35% to 71%) have been reported. Symptoms of crossed anesthesia (ipsilateral facial impairments with contralateral trunk and limb involvement ) typify brainstem lesions.
A sensory examination should include testing of superficial sensations (touch , temperature , pressure , sharp or dull discrimination ) and deep sensations (proprioception ,kinesthesia , vibration ). Combined cortical sensation such as stereognosis , tactile localization , two point discrimination , texture recognition should also be examined . Comparison with the intact side should bee viewed with caution because impairment may exist in the supposedly "normal" extremities due to aging and co- morbidities.
FLEXIBILITY AND JOINT INTEGRITY[edit | edit source]
An examination of joint flexibility should include passive ROM using a goniometer , joint hypermobility/hypomobility , and soft tissue changes (swelling ,inflammation or restriction). The shoulder and wrist should be examined closely because joint malalignment problems are common. Edema of the wrist often produces malaligned carpal bones with resulting impingement during wrist extension. Active ROM may be limited or impossible for the patient in early or middle recovery in the presence of paresis , spasticity , or obligatory synergies that can preclude isolated voluntary movements.
Contractures can develop anywhere but are particular apparent in the paretic limbs. As contractures progress , edema and pain may develop and further restrict mobility . In the UE ,limitations in the shoulder motion of flexion , abduction and external rotation are common. Contractures are likely in the elbow and finger flexors , and forearm pronators. In the LE , plantarflexion contractures are common.
MOTOR FUNCTION[edit | edit source]
TONE[edit | edit source]
Flaccidity is present immediately