Hip Osteoarthritis: Difference between revisions
m (Text replace - '<span>' to '') |
No edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editors '''- [[User:Eric Robertson|Eric Robertson]], [[User:Kim Presiaux|Kim Presiaux]] | '''Original Editors '''- [[User:Eric Robertson|Eric Robertson]], [[User:Kim Presiaux|Kim Presiaux]] | ||
'''Lead Editors''' - Your name will be added here if you are a lead editor on this page. [[Physiopedia:Editors|Read more.]]< | '''Lead Editors''' - Your name will be added here if you are a lead editor on this page. [[Physiopedia:Editors|Read more.]]<br></div> | ||
== Definition/Description == | == Definition/Description == | ||
| Line 31: | Line 19: | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
[[Image:Hip.jpg|frame|right|250x238px|Hip.jpg]]The hip joint is a synovial ball and socket joint, with the convex femoral head articulating with the concave acetabulum. Stability of the joint is achieved through a combination of muscle action and several ligaments forming a loose, but strong joint capsule. Ligaments like the iliofemoral ligament, the ischialfemoral ligament and the pubofemoral ligament keep the femoral head had at his place, in the acetabulum. Another ligament, the ligamentum teres, does not provide stability to the hip but offers a portion of blood supply to the femoral head in some individuals. <br> | [[Image:Hip.jpg|frame|right|250x238px|Hip.jpg]]The hip joint is a synovial ball and socket joint, with the convex femoral head articulating with the concave acetabulum. Stability of the joint is achieved through a combination of muscle action and several ligaments forming a loose, but strong joint capsule. Ligaments like the iliofemoral ligament, the ischialfemoral ligament and the pubofemoral ligament keep the femoral head had at his place, in the acetabulum. Another ligament, the ligamentum teres, does not provide stability to the hip but offers a portion of blood supply to the femoral head in some individuals. <br> | ||
The femoral head and acetablum are covered by smooth hyaline cartilage, and the acetabulum contains a labrum, which functions to facilitate movement and support the forces passed through the joint. | The femoral head and acetablum are covered by smooth hyaline cartilage, and the acetabulum contains a labrum, which functions to facilitate movement and support the forces passed through the joint. | ||
| Line 37: | Line 25: | ||
The hip, despite the requirement to support the weight of the body, has the second largest exursion of motion of any joint in the body. | The hip, despite the requirement to support the weight of the body, has the second largest exursion of motion of any joint in the body. | ||
External Link: [[http://www.hipsknees.info/flash/HTML-HIPS/demo.html Hip Anatomy Video]] | External Link: [[http://www.hipsknees.info/flash/HTML-HIPS/demo.html Hip Anatomy Video]] | ||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
The most important characteristic of hip osteoarthritis is that there’s damage to or loss of the articular cartilage.<ref>Book: CRIELAARD J.M., DEQUEKER J., FAMAEY J.P., FRANCHIMONG P., GRITTEN Ch., HUAUX J.P. et al. ‘Osteoartrose’. Brussel, België: drukkerij Lichtert; maart 1985.</ref> Another typical characteristic is pain, especially pain that starts when the patient start moving. These pain decreases when the patient keeps on moving or increases when he loads the joint for too long or the wrong way. Later on, they complain of a continuous pain and night pain.<ref>Book: CRIELAARD J.M., DEQUEKER J., FAMAEY J.P., FRANCHIMONG P., GRITTEN Ch., HUAUX J.P. et al. ‘Osteoartrose’. Brussel, België: drukkerij Lichtert; maart 1985.</ref> (Level of evidence: A1) | The most important characteristic of hip osteoarthritis is that there’s damage to or loss of the articular cartilage.<ref>Book: CRIELAARD J.M., DEQUEKER J., FAMAEY J.P., FRANCHIMONG P., GRITTEN Ch., HUAUX J.P. et al. ‘Osteoartrose’. Brussel, België: drukkerij Lichtert; maart 1985.</ref> Another typical characteristic is pain, especially pain that starts when the patient start moving. These pain decreases when the patient keeps on moving or increases when he loads the joint for too long or the wrong way. Later on, they complain of a continuous pain and night pain.<ref>Book: CRIELAARD J.M., DEQUEKER J., FAMAEY J.P., FRANCHIMONG P., GRITTEN Ch., HUAUX J.P. et al. ‘Osteoartrose’. Brussel, België: drukkerij Lichtert; maart 1985.</ref> (Level of evidence: A1) | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
| Line 49: | Line 37: | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
Altman et al. have established guidelines by which clinical diagnosis of hip osteoarthritis can be made. The guidelines, established in 1991, present a 3 pronged approach to diagnosis of hip osteoarthritis including clinical, radiological, and laboratory findings. According to these guidlelines, a patient was considered to have osteoarthritis if they presented with:<br> | Altman et al. have established guidelines by which clinical diagnosis of hip osteoarthritis can be made. The guidelines, established in 1991, present a 3 pronged approach to diagnosis of hip osteoarthritis including clinical, radiological, and laboratory findings. According to these guidlelines, a patient was considered to have osteoarthritis if they presented with:<br> | ||
#Hip Pain<br><u>AND</u> | #Hip Pain<br><u>AND</u> | ||
| Line 75: | Line 63: | ||
== Examination == | == Examination == | ||
<span style="font-family: arial" lang="EN-US">The beginning of OA is characterized by limited abduction and </span>rotation in the hip joint. Later on flexion, extension, adduction,.. will become more difficult.<br>Physiotherapeutic examination <ref name="Crieland">CRIELAND, e.a., Osteoartrose, Lichtert, Brussel, 1985</ref><br><br>1) Palpation of M. gluteus medius.<br> Position: patient lies on his side. Upper leg in adduction and flexion<br> OA: Zone of greater Trochanter is sensitive and painful.<br> | |||
<span style="font-family: arial" lang="EN-US">2)Flexion and forced flexion </span><br> Position: patient lies on his back.<br> OA: Flexion is limited.<br> | |||
<span style="font-family: arial" lang="EN-US">3) Extension </span>Position: Patient in prone. <br> Physiotherapist stabilizes the pelvis and raises the leg. <br> OA: Amplitude is limited.<br> | |||
<span style="font-family: arial" lang="EN-US">4) Abduction and adduction </span><br> Position: Patient lies on his back. Physiotherapist stabilizes the pelvis and performs abduction and adduction. <br> OA: abduction is limited, adduction keeps normal amplitude. | |||
== Medical Management <br> == | == Medical Management <br> == | ||
add text here <br> | add text here <br> | ||
== Physical Therapy Management <br> == | == Physical Therapy Management <br> == | ||
<span style="font-family: arial" lang="EN-US">Treatment goals: improve strength, coordination, mobility, balance, stand, stability, flexibility. Reduce pain. </span> | |||
''' | '''<u>USUAL CARE</u> <br>'''<u></u> | ||
<u | <u>Activation of the circulatory:<ref name="Crieland">Book: CRIELAND J.M., DEQUEKER J., FAMAEY J.P., FRANCHIMONG P., GRITTEN Ch., HUAUX J.P. et al. ‘Osteoartrose’. Brussel, België: drukkerij Lichtert; maart 1985.</ref></u> (Level of evidence: A1) | ||
Massage and heat therapy (radioation, conductien or conversion) can cause a better blood circulation near the skin, subcutaneous, muscles, tendons, capsules and ligaments. | |||
<u></u> | |||
<u>Passive exercises<ref name="Bennell et. al">) Kim L Bennell, Thorlene Egerton, Yong-Hao Pua, J Haxby Abbott, Kevin Sims, Ben Metcalf, Fiona McManus, Tim V Wrigley, Andrew Forbes, Anthony Harris, Rachelle Buchbinder, “EFFICACY OF A MULTIMODAL PHYSIOTHERAPY TREATMENT PROGRAM FOR HIP OSTEOARTHRITIS: A RANDOMISED PLACEBO-CONTROLLED TRIAL PROTOCOL”, 2010, BMC musculoskeletal disorder.</ref></u> | |||
< | <br> | ||
*<span style="font-family: arial" lang="EN-US">Positions patient: supine, hip in 15-30° flexion, 15-30° AB, slight ER</span> | *<span style="font-family: arial" lang="EN-US">Positions patient: supine, hip in 15-30° flexion, 15-30° AB, slight ER</span> | ||
<span style="font-family: arial" lang="EN-US"> Physiotherapist: perform 3-6 thrusts at the beginning of the first set then perform oscillations. </span> | <span style="font-family: arial" lang="EN-US"> Physiotherapist: perform 3-6 thrusts at the beginning of the first set then perform oscillations. </span> | ||
*<span style="font-family: arial" lang="EN-US">Positions patient: supine with hip flexed</span> | *<span style="font-family: arial" lang="EN-US">Positions patient: supine with hip flexed</span> | ||
<span style="font-family: arial" lang="EN-US"> Physiotherapist: oscillatory passive mobilizations, applied caudally or laterally to the proximal thigh </span> | <span style="font-family: arial" lang="EN-US"> Physiotherapist: oscillatory passive mobilizations, applied caudally or laterally to the proximal thigh </span> | ||
*<span style="font-family: arial" lang="EN-US">Position patient: Prone with knee flexed.</span> | *<span style="font-family: arial" lang="EN-US">Position patient: Prone with knee flexed.</span> | ||
<span style="font-family: arial" lang="EN-US"> Physiotherapist: IR until contralateral pelvis rises, apply oscillatory force downwards to contralateral pelvis</span><br> | <span style="font-family: arial" lang="EN-US"> Physiotherapist: IR until contralateral pelvis rises, apply oscillatory force downwards to contralateral pelvis</span><br> | ||
*<span style="font-family: arial" lang="EN-US">Firm effleurage stroke, deep frictions or sustained pressure trigger </span>point release with the muscle on stretch.<br><span style="font-family: arial" lang="EN-US">Position patient: Prone. The hip is in 10-15 ° AB. </span> | *<span style="font-family: arial" lang="EN-US">Firm effleurage stroke, deep frictions or sustained pressure trigger </span>point release with the muscle on stretch.<br><span style="font-family: arial" lang="EN-US">Position patient: Prone. The hip is in 10-15 ° AB. </span> | ||
| Line 121: | Line 109: | ||
*<span style="font-family: arial" lang="EN-US">Position patient: Supine with hip in flexion and adduction. </span> | *<span style="font-family: arial" lang="EN-US">Position patient: Supine with hip in flexion and adduction. </span> | ||
<span style="font-family: arial" lang="EN-US"> Physiotherapist: Use body weight to impart passive oscillations to the postero-lateral hip capsule through the long axis | <span style="font-family: arial" lang="EN-US"> Physiotherapist: Use body weight to impart passive oscillations to the postero-lateral hip capsule through the long axis of the femur. Add more flexion, adduction, and/or internal rotation to progress. </span><br> | ||
*<span style="font-family: arial" lang="EN-US">Massage of quads, hamstrings, psoas, adductors, abductors, </span>gluteus-muscles | *<span style="font-family: arial" lang="EN-US">Massage of quads, hamstrings, psoas, adductors, abductors, </span>gluteus-muscles | ||
<br> | <br> | ||
<u><span style="font-family: arial" lang="EN-US">Active exercises</span></u> | <u><span style="font-family: arial" lang="EN-US">Active exercises</span></u> | ||
| Line 135: | Line 123: | ||
*<span style="font-family: arial" lang="EN-US">Balance exercises <ref name="Bennell et. al">) Kim L Bennell, Thorlene Egerton, Yong-Hao Pua, J Haxby Abbott, Kevin Sims, Ben Metcalf, Fiona McManus, Tim V Wrigley, Andrew Forbes, Anthony Harris, Rachelle Buchbinder, “EFFICACY OF A MULTIMODAL PHYSIOTHERAPY TREATMENT PROGRAM FOR HIP OSTEOARTHRITIS: A RANDOMISED PLACEBO-CONTROLLED TRIAL PROTOCOL”, 2010, BMC musculoskeletal disorder.</ref></span><br><span style="font-family: arial" lang="EN-US">( Standing weight shifting forwards/ lateral, Standing in double leg stance on foam, Shuttle walking, Stairs) </span> | *<span style="font-family: arial" lang="EN-US">Balance exercises <ref name="Bennell et. al">) Kim L Bennell, Thorlene Egerton, Yong-Hao Pua, J Haxby Abbott, Kevin Sims, Ben Metcalf, Fiona McManus, Tim V Wrigley, Andrew Forbes, Anthony Harris, Rachelle Buchbinder, “EFFICACY OF A MULTIMODAL PHYSIOTHERAPY TREATMENT PROGRAM FOR HIP OSTEOARTHRITIS: A RANDOMISED PLACEBO-CONTROLLED TRIAL PROTOCOL”, 2010, BMC musculoskeletal disorder.</ref></span><br><span style="font-family: arial" lang="EN-US">( Standing weight shifting forwards/ lateral, Standing in double leg stance on foam, Shuttle walking, Stairs) </span> | ||
* | *<u></u><span style="font-family: arial" lang="EN-US">Endurance exercises </span><br><span style="font-family: arial" lang="EN-US">Walk, cycle, swim </span> | ||
<br> | <br> | ||
<u><span style="font-family: arial" lang="EN-US">Aquatherapy<ref name="Crieland" /> </span></u><span style="font-family: arial" lang="EN-US"> (Level of evidence: A1)</span> | <u><span style="font-family: arial" lang="EN-US">Aquatherapy<ref name="Crieland" /> </span></u><span style="font-family: arial" lang="EN-US"> (Level of evidence: A1)</span> | ||
| Line 147: | Line 135: | ||
<u><span style="font-family: arial" lang="EN-US">Advice and education</span></u> | <u><span style="font-family: arial" lang="EN-US">Advice and education</span></u> | ||
<span style="font-family: arial" lang="EN-US">In the treatment it is very important to tell the patient about his condition. Why does it occur? What's the treatment? What's the importance of exercise? </span> | <span style="font-family: arial" lang="EN-US">In the treatment it is very important to tell the patient about his condition. Why does it occur? What's the treatment? What's the importance of exercise? </span> | ||
This will make the patient have a clear understanding in his condition and will improve the healing.<ref name="Bennell et. al">) Kim L Bennell, Thorlene Egerton, Yong-Hao Pua, J Haxby Abbott, Kevin Sims, Ben Metcalf, Fiona McManus, Tim V Wrigley, Andrew Forbes, Anthony Harris, Rachelle Buchbinder, “EFFICACY OF A MULTIMODAL PHYSIOTHERAPY TREATMENT PROGRAM FOR HIP OSTEOARTHRITIS: A RANDOMISED PLACEBO-CONTROLLED TRIAL PROTOCOL”, 2010, BMC musculoskeletal disorder.</ref> | This will make the patient have a clear understanding in his condition and will improve the healing.<ref name="Bennell et. al">) Kim L Bennell, Thorlene Egerton, Yong-Hao Pua, J Haxby Abbott, Kevin Sims, Ben Metcalf, Fiona McManus, Tim V Wrigley, Andrew Forbes, Anthony Harris, Rachelle Buchbinder, “EFFICACY OF A MULTIMODAL PHYSIOTHERAPY TREATMENT PROGRAM FOR HIP OSTEOARTHRITIS: A RANDOMISED PLACEBO-CONTROLLED TRIAL PROTOCOL”, 2010, BMC musculoskeletal disorder.</ref> | ||
| Line 153: | Line 141: | ||
It’s also very important to tell the patient what he can and can not do. | It’s also very important to tell the patient what he can and can not do. | ||
<br> | <br> | ||
<u><span style="font-family: arial" lang="EN-US">BGA</span></u> | <u><span style="font-family: arial" lang="EN-US">BGA</span></u> | ||
<span style="font-family: arial" lang="EN-US">Behavioral graded activities is an kind of treatment that contains normal exercise therapy comprising booster sessions. </span> | <span style="font-family: arial" lang="EN-US">Behavioral graded activities is an kind of treatment that contains normal exercise therapy comprising booster sessions. </span> | ||
The long term effectiveness have been showed, but it is never proved that this treatment has a better efficacy than usual care.<ref name="Vaenhof et. al">cindy veenhof, albère j. a. köke, joost dekker, rob a. oostendorp, johannes w. j. bijlsma, maurits w. van tulder, and cornelia h. m. van den ende, "EFFECTIVENESS OF BEHAVIORAL GRADED ACTIVITY IN PATIENTS WITH OSTEOARTHRITIS OF THE HIP AND/OR KNEE: A RANDOMIZED CLINICAL TRIAL", 2006, Arthritis &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Rheumatism</ref> | The long term effectiveness have been showed, but it is never proved that this treatment has a better efficacy than usual care.<ref name="Vaenhof et. al">cindy veenhof, albère j. a. köke, joost dekker, rob a. oostendorp, johannes w. j. bijlsma, maurits w. van tulder, and cornelia h. m. van den ende, "EFFECTIVENESS OF BEHAVIORAL GRADED ACTIVITY IN PATIENTS WITH OSTEOARTHRITIS OF THE HIP AND/OR KNEE: A RANDOMIZED CLINICAL TRIAL", 2006, Arthritis &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Rheumatism</ref> | ||
BGA intervention consists of 3 phases:<ref name="Pister et. al">M.F. Pister, C. Veenhof, F.G. Schellevis, D.H. De Bakker, J. Dekker, "LONG-TERM EFFECTIVENESS OF EXERCISE THERAPY IN PATIENTS WITH OSTEOARTHRITIS OF THE HIP OR KNEE: A RANDOMIZED CONTROLLED TRIAL COMPARING TWO DIFFERENT PHYSICAL THERAPY INTERVENTIONS", Osteoarthritis and Cartilage, 2010</ref> | BGA intervention consists of 3 phases:<ref name="Pister et. al">M.F. Pister, C. Veenhof, F.G. Schellevis, D.H. De Bakker, J. Dekker, "LONG-TERM EFFECTIVENESS OF EXERCISE THERAPY IN PATIENTS WITH OSTEOARTHRITIS OF THE HIP OR KNEE: A RANDOMIZED CONTROLLED TRIAL COMPARING TWO DIFFERENT PHYSICAL THERAPY INTERVENTIONS", Osteoarthritis and Cartilage, 2010</ref> | ||
1) Starting phase: The physiotherapist will educate the patient about his condition. <br>And there will be made a list of treatment goals and problematic activities. | |||
<span style="font-family: arial" lang="EN-US"> </span>2) Treatment phase: increasingly difficult exercises. | |||
<span style="font-family: arial" lang="EN-US"> </span>3) Integration phase: The physiotherapist will support and integrate behavioral changes. | |||
== Key Research == | == Key Research == | ||
add links and reviews of high quality evidence here (case studies should be added on new pages using the [[Template:Case Study|case study template]])<br> | add links and reviews of high quality evidence here (case studies should be added on new pages using the [[Template:Case Study|case study template]])<br> | ||
== Resources <br> == | == Resources <br> == | ||
add appropriate resources here <br> | add appropriate resources here <br> | ||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
add text here <br> | add text here <br> | ||
== Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed])<br> == | |||
<div class="researchbox"><rss>http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=12qsGRxYSRWCvW-2s8h--v97pPBoMGMpmU4-a64BPBka_87suP|short|max=10</rss></div> | <div class="researchbox"><rss>http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=12qsGRxYSRWCvW-2s8h--v97pPBoMGMpmU4-a64BPBka_87suP|short|max=10</rss></div> | ||
== References == | == References == | ||
<references /> | <references /> | ||
see [[Adding References|adding references tutorial]]. <references /></div> | see [[Adding References|adding references tutorial]]. <references /></div> | ||
[[Category:Vrije_Universiteit_Brussel_Project|Template:VUB]] | [[Category:Vrije_Universiteit_Brussel_Project|Template:VUB]] | ||
Revision as of 20:52, 1 June 2013
Original Editors - Eric Robertson, Kim Presiaux
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.Definition/Description[edit | edit source]
Hip osteoarthritis is a common type of osteoarthritis. Since the hip is a weight-bearing joint, osteoarthritis can cause significant problems.
Hip osteoarthritis is caused by deterioration of articular cartilage of the hip joint.
There are several risk factors[1]: (Level of evidence: A1)
- Previous hip injury
- Previous fracture, which changes hip alignment
- Genetics
- Congenital and developmental hip disease
- Subchondral bone that is too soft or too hard
- Overweight
- Occupation
- Age
- Gender
- Sport
Clinically Relevant Anatomy[edit | edit source]
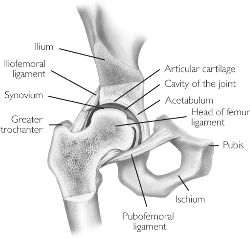
The hip joint is a synovial ball and socket joint, with the convex femoral head articulating with the concave acetabulum. Stability of the joint is achieved through a combination of muscle action and several ligaments forming a loose, but strong joint capsule. Ligaments like the iliofemoral ligament, the ischialfemoral ligament and the pubofemoral ligament keep the femoral head had at his place, in the acetabulum. Another ligament, the ligamentum teres, does not provide stability to the hip but offers a portion of blood supply to the femoral head in some individuals.
The femoral head and acetablum are covered by smooth hyaline cartilage, and the acetabulum contains a labrum, which functions to facilitate movement and support the forces passed through the joint.
The hip, despite the requirement to support the weight of the body, has the second largest exursion of motion of any joint in the body.
External Link: [Hip Anatomy Video]
Characteristics/Clinical Presentation[edit | edit source]
The most important characteristic of hip osteoarthritis is that there’s damage to or loss of the articular cartilage.[2] Another typical characteristic is pain, especially pain that starts when the patient start moving. These pain decreases when the patient keeps on moving or increases when he loads the joint for too long or the wrong way. Later on, they complain of a continuous pain and night pain.[3] (Level of evidence: A1)
Differential Diagnosis[edit | edit source]
add text here
Diagnostic Procedures[edit | edit source]
Altman et al. have established guidelines by which clinical diagnosis of hip osteoarthritis can be made. The guidelines, established in 1991, present a 3 pronged approach to diagnosis of hip osteoarthritis including clinical, radiological, and laboratory findings. According to these guidlelines, a patient was considered to have osteoarthritis if they presented with:
- Hip Pain
AND - Hip Internal Rotation ≤ 15 °
Hip Flexion ≤ 115°
OR:
Hip pain and:
- Hip Rotation ≥ 15°
Or : - Pain with Hip Internal Rotation
Or: - Hip stiffness in the AM ≤ 60 minutes
Or: - Age > 50 years
More recently, Sutlive et al.[4] have proposed a clinical prediction rule to identify individuals with hip osteoarthritis presenting with unilateral hip pain. (Level of evidence: A2) This clinical prediction rule is to detect OA in patients with unilateral hip pain.By this way, it assists clinicians in determining which patients require further testing and evaluation, and when to initiate early management, which may minimize the deleterious effects of hip OA and maximize function. This clinical prediction rule is based on 5 predictor variables. If a subject exhibited only 1 or 2 of the predictor variables, the posttest probability of having hip OA only increased from 29% to 33% and 46%, respectively.However, if a subject had at least 3 predictors present, the likelihood of having
hip OA increased from 29% to 68%. If a subject exhibited at least 4 of the 5 predictors, the posttest probability increased further to 91%.
The five predictor variables are:
- Flexion (involved side)
- Internal rotation (involved side)
- Scour test (involved side)
- Patrick’s test (involved side)
- Hip flexion test (involved side)
Outcome Measures[edit | edit source]
Hip Disability and Osteoarthritis Outcome Score
Examination[edit | edit source]
The beginning of OA is characterized by limited abduction and rotation in the hip joint. Later on flexion, extension, adduction,.. will become more difficult.
Physiotherapeutic examination [5]
1) Palpation of M. gluteus medius.
Position: patient lies on his side. Upper leg in adduction and flexion
OA: Zone of greater Trochanter is sensitive and painful.
2)Flexion and forced flexion
Position: patient lies on his back.
OA: Flexion is limited.
3) Extension Position: Patient in prone.
Physiotherapist stabilizes the pelvis and raises the leg.
OA: Amplitude is limited.
4) Abduction and adduction
Position: Patient lies on his back. Physiotherapist stabilizes the pelvis and performs abduction and adduction.
OA: abduction is limited, adduction keeps normal amplitude.
Medical Management
[edit | edit source]
add text here
Physical Therapy Management
[edit | edit source]
Treatment goals: improve strength, coordination, mobility, balance, stand, stability, flexibility. Reduce pain.
USUAL CARE
Activation of the circulatory:[5] (Level of evidence: A1)
Massage and heat therapy (radioation, conductien or conversion) can cause a better blood circulation near the skin, subcutaneous, muscles, tendons, capsules and ligaments.
Passive exercises[6]
- Positions patient: supine, hip in 15-30° flexion, 15-30° AB, slight ER
Physiotherapist: perform 3-6 thrusts at the beginning of the first set then perform oscillations.
- Positions patient: supine with hip flexed
Physiotherapist: oscillatory passive mobilizations, applied caudally or laterally to the proximal thigh
- Position patient: Prone with knee flexed.
Physiotherapist: IR until contralateral pelvis rises, apply oscillatory force downwards to contralateral pelvis
- Firm effleurage stroke, deep frictions or sustained pressure trigger point release with the muscle on stretch.
Position patient: Prone. The hip is in 10-15 ° AB.
Physiotherapist: Perform caudally directed oscillations. May perform 3-6 thrusts at the beginning of the first set.
- Position patient: Supine with hip in flexion and adduction.
Physiotherapist: Use body weight to impart passive oscillations to the postero-lateral hip capsule through the long axis of the femur. Add more flexion, adduction, and/or internal rotation to progress.
- Massage of quads, hamstrings, psoas, adductors, abductors, gluteus-muscles
Active exercises
- Knee to chest exercise (strengthens the abdominal muscles and improves the flexibility of the hip, back and neck) Patient lies on the floor with left leg straight and right foot flat on the floor. Grabs his knee and bring it toward to his chest, holds for 30seconds and switches legs.
- Bridging exercise ( strengthens buttock abdominal and hamstrings muscles) Patient lies on his back with knees bent and feet flat on the floor. While tightening abdominal muscles he lifts his pelvis slightly upwards. Hold for 15-20 seconds. Repeat 8-12 times.
- Balance exercises [6]
( Standing weight shifting forwards/ lateral, Standing in double leg stance on foam, Shuttle walking, Stairs)
- Endurance exercises
Walk, cycle, swim
Aquatherapy[5] (Level of evidence: A1)
Passive and active mobilization could be done in water as well, by an indifferent temperature (35 degrees), in order to facilitaite recovery of the motorfuntion. In this situation, gravity is greatly reduced thus the burdensome weight and tension at the height of the effected joint will be reduced as well.
Advice and education
In the treatment it is very important to tell the patient about his condition. Why does it occur? What's the treatment? What's the importance of exercise?
This will make the patient have a clear understanding in his condition and will improve the healing.[6]
It’s also very important to tell the patient what he can and can not do.
BGA
Behavioral graded activities is an kind of treatment that contains normal exercise therapy comprising booster sessions.
The long term effectiveness have been showed, but it is never proved that this treatment has a better efficacy than usual care.[7]
BGA intervention consists of 3 phases:[8]
1) Starting phase: The physiotherapist will educate the patient about his condition.
And there will be made a list of treatment goals and problematic activities.
2) Treatment phase: increasingly difficult exercises.
3) Integration phase: The physiotherapist will support and integrate behavioral changes.
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
add appropriate resources here
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)
[edit | edit source]
References[edit | edit source]
- ↑ Book: REGINSTER et al. 'Osteoarthritis. Clinical and Experimental Aspects'. Springer, Verlag Berlin Heiderlberg, 1999.
- ↑ Book: CRIELAARD J.M., DEQUEKER J., FAMAEY J.P., FRANCHIMONG P., GRITTEN Ch., HUAUX J.P. et al. ‘Osteoartrose’. Brussel, België: drukkerij Lichtert; maart 1985.
- ↑ Book: CRIELAARD J.M., DEQUEKER J., FAMAEY J.P., FRANCHIMONG P., GRITTEN Ch., HUAUX J.P. et al. ‘Osteoartrose’. Brussel, België: drukkerij Lichtert; maart 1985.
- ↑ SUTLIVE et al. 'Development of a Clinical Prediction Rule for Diagnosing Hip Osteoarthritis in Individuals With Unilateral Hip Pain'. J Orthop Sports Phys Ther.: September 2008;38(9):542-50.
- ↑ 5.0 5.1 5.2 CRIELAND, e.a., Osteoartrose, Lichtert, Brussel, 1985 Cite error: Invalid
<ref>tag; name "Crieland" defined multiple times with different content - ↑ 6.0 6.1 6.2 ) Kim L Bennell, Thorlene Egerton, Yong-Hao Pua, J Haxby Abbott, Kevin Sims, Ben Metcalf, Fiona McManus, Tim V Wrigley, Andrew Forbes, Anthony Harris, Rachelle Buchbinder, “EFFICACY OF A MULTIMODAL PHYSIOTHERAPY TREATMENT PROGRAM FOR HIP OSTEOARTHRITIS: A RANDOMISED PLACEBO-CONTROLLED TRIAL PROTOCOL”, 2010, BMC musculoskeletal disorder.
- ↑ cindy veenhof, albère j. a. köke, joost dekker, rob a. oostendorp, johannes w. j. bijlsma, maurits w. van tulder, and cornelia h. m. van den ende, "EFFECTIVENESS OF BEHAVIORAL GRADED ACTIVITY IN PATIENTS WITH OSTEOARTHRITIS OF THE HIP AND/OR KNEE: A RANDOMIZED CLINICAL TRIAL", 2006, Arthritis &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Rheumatism
- ↑ M.F. Pister, C. Veenhof, F.G. Schellevis, D.H. De Bakker, J. Dekker, "LONG-TERM EFFECTIVENESS OF EXERCISE THERAPY IN PATIENTS WITH OSTEOARTHRITIS OF THE HIP OR KNEE: A RANDOMIZED CONTROLLED TRIAL COMPARING TWO DIFFERENT PHYSICAL THERAPY INTERVENTIONS", Osteoarthritis and Cartilage, 2010
see adding references tutorial. </div>