Hip Pain and Mobility Deficits
Original Editors - Tyler Shultz
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Discussion & Background[edit | edit source]
The purpose of this clinical guideline is to describe the evidence based physical therapy practice including diagnosis, prognosis, intervention and assessment of outcome for musculoskeletal disorders related to hip osteoarthritis that are commonly managed with orthopaedic physical therapy techniques.
More specifically, in the paragraphs that follow, there will be a review of recommendations related to: diagnosis and classification, examination, and treatment/interventions. These recommendations will be supported with a grade of evidence based on Guyatt et al[1], as modified by MacDermid.In this modified system, the typical A, B, C, and D grades of evidence have been modified to include the role of consensus expert opinion and basic research to demonstrate baseic biological or biomechanical plausibility.[2]
All information presented on this page is adapted from:
Diagnosis & Classification Recommendations[edit | edit source]
Diagnosis/Classification (Grade: A)
Moderate lateral or anterior hip pain during weight bearing, in adults over the age of 50 years, with morning stiffness less than 1 hour, with limited hip interanl rotation and hip flexion by more than 15 degrees when comparing the painful to the nonpainful side are useful clinical findings to classify a patient with hip pain into the International Statistical Classification of Diseases and Related Health Problems (ICD) category of unilateral coxarthrosis and the associated International Classification of Functioning, Disability, and Health (ICF) impairment based category of hip pain and mobility deficits.
Risk Factors (Grade: A)
Clinicians should consider age, hip developmental disorders, and previous hip injury as risk factors for hip osteoarthritis.
Pathoanatomical Features (Grade: B)
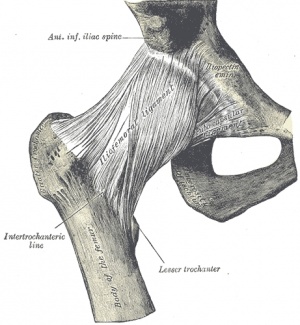
Clinicians should assess for impairments in mobility of the hip joint and strength of the surrounding muscles, especially the hip abductor muscles, when a patient present with hip pain.
Differential Diagnosis (Grade: E)
Clinicians should consider diagnostic classifications other than osteoarthritis of the hip when the patient's history, reported activity limitations, or impairments of body function and structure are not consistent with those presented in this guideline --or-- when the patient's symptoms are not diminishing with interventions aimed at normalization of the patient's impairment of body function.
Examination Recommendations[edit | edit source]
Intervention & Treatment Recommendations[edit | edit source]
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: LINK|charset=UTF-8|short|max=10References
[edit | edit source]
- ↑ Guyatt G, Sackett D, Sinclair J, Hayward R, Cook D, Cook R. Users' guides to the medical literature. IX. A method for grading health care recommendations. Evidence-Based Medicine Working Group. JAMA. 1995;274:1800-1804.
- ↑ Cibulka MT, White DM, Woehrle J, et al. Hip pain and mobility deficits--hip osteoarthritis: clinical practice guidelines linked to the international classification of functioning, disability, and health from the orthopaedic section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2009;39(4):A1-25.