Meniscal Repair
Original Editor - Rachael Lowe, Jennifer Uytterhaegen
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Definition/Description[edit | edit source]
| [1] |
An arthroscopic meniscectomy is a surgical procedure to remove a part or the complete medial or lateral meniscus of the knee joint using arthroscopic or keyhole surgery. In a complete meniscectomy the meniscus including the meniscal rim is removed. Partial meniscectomy is a procedure where the meniscus is partially removed. This may vary from minor trimming of a frayed edge to anything short of removing the rim. This is a minimally invasive procedure often undergone as an outpatient in a one-day clinic [2]
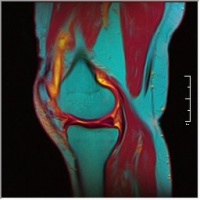
Clinically Relevant Anatomy[edit | edit source]
Anatomical description shows a difference between the medial and the lateral meniscus [3]:
- The medial meniscus is larger than the lateral meniscus and has a C shape. It will combine with the medial collateral ligament [4]
- The lateral meniscus is smaller than the medial meniscus and has an O-shape. This is more mobile than the medial meniscus and will combine with the popliteus muscle. [4]
- When the patient performs flexion of the knee, the menisci move posteriorly to the tibial plateau. By extension, the original position taken
- When the patient performs internal rotation, the medial meniscus but slightly forward while the lateral is moved slightly to the dorsal. In external rotation is the inverse [4]
- Both menisci are composed of cartilage and Type I collagen.[3]
Indication for Procedure
[edit | edit source]
Meniscal tears that are not suitable for meniscal repair.[2]
Clinical Presentation[edit | edit source]
- joint line tenderness and effusion
- symptoms are frequently worsened by flexing and loading the knee, activities such as squatting and kneeling are poorly tolerated.
- complaints of 'clicking', 'locking' and 'giving way' are common
- functionally unstable knee [3]
- symptoms are frequently worsened by flexing and loading the knee, activities such as squatting and kneeling are poorly tolerated because of stiffness and pain [2]
Diagnostic Tests[edit | edit source]
- Joint line tenderness has been reported to be the best common test for meniscal injury [2]
- McMurray's test positive if a pop or a snap at the joint line occurs while flexing and rotating the patient's knee.
- Apley's test performed with the patient prone, and with the examiner hyperflexing the knee and rotating the tibial plateau on the femoral condyles.
- Steinman's test performed on a supine patient by bringing the knee into flexion and rotating.
- Ege's Test is performed with the patient squatting, an audible and palpable click is heard/felt over the area of the meniscus tear. The patient's feet are turned outwards to detect a medial meniscus tear, and turned inwards to detect a lateral meniscus tear.
- MRI: The demonstration of meniscal lesions by MRI has a crucial role in patients with combined injuries as the menisci. The main challenge for MRI is the assessment of the meniscal surfaces. MRI signs of abnormal findings [5]:
- Grade I: discrete central degeneration: an intrameniscal lesion of increased signal without connection to articular surface [5]
- Grade II: Extensive central degeneration: larger intrameniscal area of increased signal intensity, may be horizontal in orientation or lineair, again without connection to articular surface [5]
- Grade III: menisci tear: increased intrameniscal signal intensity with contour disruption of articular surface, may be associated with displacement of meniscal fragments or superficial step formation [5]
- Grade IV: complex meniscal tear: multiple disruption of meniscal surfaces
The difference of tears in the red and in the white zone of the meniscus is important since reattachment of meniscal fragments is promising only in the vascularized zone. [5]
Medical Management
[edit | edit source]
add text here
Physical Therapy Management
[edit | edit source]
Pre-Op
add text here relating to the pre-operative advice
Post-Op
The goal of rehabilitation is to restore patient function based on individual needs. It is important to consider:
- the type of surgical procedure
- the post-surgical protocol determined by the surgeon
[6] - which meniscus was repaired
- the type of meniscal tear
- preoperative knee status (including time between injury and surgery)
- decreased range of motion or strength
- the patient's age
- the presence of coexisting knee pathology (particularly ligamentous laxity or articular cartilage degeneration)
- the patient's functional and/or athletic expectations and motivations
- Control the pain, swelling and inflammation by using: cryotherapy, analgaesics, NSAIDs. [5]
- As rehabilitation progresses, continued use of modalities may be required to control residual pain and swelling. [7]
- Restore range of motion using exercises within the limits that the surgeon has specified [5]
- If a meniscal repair has been performed, extreme flexion and rotation should be limited until the wound in the meniscus has had time to heal (8 to 12 weeks).
- Restore muscle function using specific strengthening exercises including quadriceps, hamstrings, hip. Examples: [5]
- for quadriceps: squads
- for hamstrings: leg curl with resistance (eg resistance band)
- for hip: bridging
- Strengthening around the knee is crucial but it may also be necessary to strengthen the adjacent joints if weight-bearing was restricted pre- or post-operatively.
- While strong muscles around the joint are critical, flexibility exercises of the same muscle groups must be considered and should be included throughout the period of strengthening.
- Optimize neuromuscular coordination and proprioceptive re-education. [5]
- The patient, physical therapist and surgeon will determine the extent of these exercises. [7]
- Progress weight-bearing: weight-bearing and joint stress are necessary to enhance the functionality of the meniscal repair and should be progressed as indicated by the surgeon.[5]
Some indications:
- Full weight bearing or bearing weight as tolerated immediately after the meniscectomy.
- Passive and active range-of-motion exercises begin immediately postoperatively and quadriceps strengthening exercises.
- Crutches are usually required for 2-5 days until the patient is able to fully put his/her body weight on the knee without discomfort.
- Return to full daily activity usually at 4-6 weeks, only if there is full range of motion and what about strength
- Sporters are allowed to return to full athletic activities when their quadriceps muscle tone is returned (how do you evaluate this?) and they have painless range of motion.
--> EMG-B (electromyography-biofeedback) is an effective treatment in improving quadriceps muscle strength after arthroscopic meniscectomy surgery [4]
Type of exercises [4]:
- Stability exercises, then coordination and finally strength exercises. Training of the quadriceps amd hamstrings is highly important.[4]
- At first closed chain exercises are advised and compressive joint load for less drive strength in the joint. Example of exercises are cycling, leg press. For coordination squat and lunges can be given as exercises. [4]
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
add appropriate resources here
Timothy Brindle,John Nyland and Darren L. Johnson (2001) The Meniscus: Review of Basic Principles With Application to Surgery and Rehabilitation. Journal of Athletic Training, 36(2), 160–169.
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=10EkZzEWYAt7Fa9CcceouCmgTc149l7sGxhrWlCq5g6yslvMJl|charset=UTF-8|short|max=10: Error parsing XML for RSS
References
[edit | edit source]
- ↑ BJC Houston. Arthroscopic Partial Meniscectomy. Available from: http://www.youtube.com/watch?v=VElp9SpGS-Q&feature=player_embedded [last accessed 18/08/12]
- ↑ 2.0 2.1 2.2 2.3 Meserve BB, Cleland JA, Boucher TR. A meta-analysis examining clinical test utilities for assessing meniscal injury. Clinical Rehabilitation; 2008: 22(2), 143-61.
- ↑ 3.0 3.1 3.2 McKeon B, Bono J, Richmond J. Knee Arthroscopy. Springer; 2009: 202 (1, 2, 12, 43)
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Atkinson H., Laver J., Sharp E. Physiotherapy and Rehabilitation following arthroscopic menisectomy.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 5.9 Teller P. MRI atlas of orthopedics and traumatology of the knee. Springer: 2003: 291 (131 – 132)
- ↑ Kohn, D., et al. "Postoperative Follow-up and Rehabilitation after Meniscus Replacement." Scandinavian Journal of Medicine and Science in Sports 9 3 (1999): 177-180. National Center for Biotechnology Information. National Library of Medicine. 24 Nov. 2004
- ↑ 7.0 7.1 Thomson, L. C., et al. "Physiotherapist-led Programmes and Interventions for Rehabilitation of Anterior Cruciate Ligament, Medial Collateral Ligament and Meniscal Injuries of the Knee in Adults." Cochrane Database System Review 2 (2002): CD001354. National Center for Biotechnology Information. National Library of Medicine. 24 Nov. 2004