Modic Changes
Original Editor - Your name will be added here if you created the original content for this page.
Lead Editors
Clinically Relevant Anatomy may[edit | edit source]
Modic changes (MC) are bone marrow lesions seen within a vertebral body on magnetic resonance imaging (MRI), suggestive of being associated with low back pain (LBP). [1] Their presence in clients receiving physiotherapy for low back pain may be of significance when discussing prognosis and benefits of exercise therapy.
Mechanism of Injury / Pathological Process
[edit | edit source]
Research on the subject has been published since 1988 when MC were first identified by Dr. Michael Modic. Subsequent publications on the subject provided incremental gains in understanding of this new diagnostic entity. Though causes and mechanisms responsible for formation of MC are still poorly understood, progress is being made in linking his spinal phenotype with disc degeneration and LBP. This is significant because currently the value MRI in management of LBP remains low due to lack of phenotypical features strongly correlating with clinical symptoms.
Modic changes classification consists of 4 types. Type 0- normal disc and vertebral body appearance, MC type I characterized by presence of bone marrow edema within vertebral body and hyper-vascularization, type II features fatty replacements of the red bone marrow within vertebral body and type III marked by subchondral bone sclerosis. [2] Same authors postulated that the types form a continuum along which stages will progress. Estimate of 18-24 months was provided for transition form type I to type II though others feel that much larger longitudinal studies are required to support this idea.
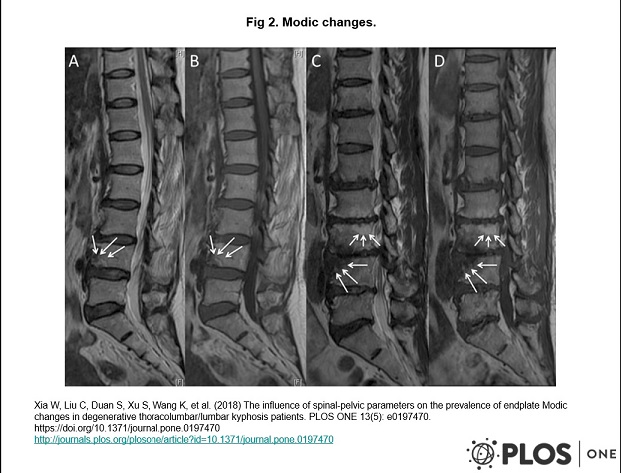
Fig 1. Modic changes.
Modic type I change: hyperintense on T2WI (A↘), hypointense on T1WI (B↘) at inferior endplate of L4. Modic type II change: hyperintense on T2WI (C upper↘), hyperintense on T1WI (D upper↘) at superior endplate of L3. Modic type III change: hypointense on T2WI (C inferior↘), hypointense on T1WI (D inferior↘) at superior endplate of L4.[3]
Clinical Presentation[edit | edit source]
The subgroup of LBP clients with MC seeking physiotherapy care may more often report:
- constant and nocturnal pain
- higher level of functional impairment
- lack of improvement at week 4 since onset or later.
- failed exercise therapy attempts
Proposed risk factors for developing MC include:
Physical examination findings may not be useful for differentiating between clients with and without MC and characteristic of degenerative disk disease.
Diagnostic Procedures[edit | edit source]
MRI
Management / Interventions
[edit | edit source]
A single randomized controlled trial[5] evaluated comparative effects of rest and exercise in treatment off LPB with MC concluding that here was no statistically significant difference between groups on following outcome measures:
- The numerical rating scale [27] (NRS) measures current back pain on a 0 to10 scale.
- The Roland Morris Disability Questionnaire [28] (RMQ) is a 23-item disability questionnaire with a 0 to 23 scale, measuring activity limitation.
- EuroQol [29,30] (EQ-5D) is a standardized instrument measuring health status-related quality of life consisting of a health status index (EQindex 0 to 1 scale) and a visual analogue scale (EQVAS 0 to 100 scale).
- The global assessment transition questionnaire measures the patients' perceptions of the overall change in their back pain since the beginning of the study on a 7-point Likert scale
- days lost from work due to pain
Resources
[edit | edit source]
add appropriate resources here
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Mok FP, Samartzis D, Karppinen J, Fong DY, Luk KD, Cheung KM. Modic changes of the lumbar spine: prevalence, risk factors, and association with disc degeneration and low back pain in a large-scale population-based cohort. The Spine Journal. 2016 Jan 1;16(1):32-41.
- ↑ Modic MT, Masaryk TJ, Ross JS, Carter JR. Imaging of degenerative disk disease. Radiology. 1988 Jul;168(1):177-86.
- ↑ 3.0 3.1 3.2 Xia W, Liu C, Duan S, Xu S, Wang K, Zhu Z, Liu H. The influence of spinal-pelvic parameters on the prevalence of endplate Modic changes in degenerative thoracolumbar/lumbar kyphosis patients. PloS one. 2018 May 15;13(5):e0197470.
- ↑ 4.0 4.1 Määttä JH, Wadge S, MacGregor A, Karppinen J, Williams FM. ISSLS prize winner: vertebral endplate (Modic) change is an independent risk factor for episodes of severe and disabling low back pain. Spine. 2015 Aug 1;40(15):1187-93.
- ↑ Jensen RK, Leboeuf-Yde C, Wedderkopp N, Sorensen JS, Manniche C. Rest versus exercise as treatment for patients with low back pain and Modic changes. A randomized controlled clinical trial. BMC medicine. 2012 Dec;10(1):22.