Moyamoya Disease: Difference between revisions
Wendy Walker (talk | contribs) No edit summary |
Wendy Walker (talk | contribs) No edit summary |
||
| Line 6: | Line 6: | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
Moyamoya Disease is a disorder of some of the blood vessels in the brain: the internal carotid arteries, and the arteries which branch from them. It is a rare cause of Stroke and TIAs. | Moyamoya Disease [MMD] is a disorder of some of the blood vessels in the brain: the internal carotid arteries, and the arteries which branch from them, the Circle of Willis<ref>Scott R.M., Smith E.R. Moyamoya disease and moyamoya syndrome. N. Engl. J. Med. 2009;360(12):1226–1237.</ref>. It is a rare cause of Stroke and TIAs. | ||
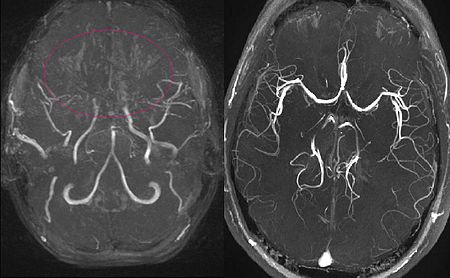
[[File:MRA Moya-moya-disease.JPG|alt=2 images, both MIP reconstructed MR angiographies; one is that of an 11 year old girl with Moyamoya Disease, which shows the characteristic occluded cranial arteries, and the other image shows a healthy subject for comparison.|The image on the left: MIP reconstructed MR angiography of a 11 year old girl with Moyamoya Disease. The image on the right: a healthy subject for comparison. |frame]] | [[File:MRA Moya-moya-disease.JPG|alt=2 images, both MIP reconstructed MR angiographies; one is that of an 11 year old girl with Moyamoya Disease, which shows the characteristic occluded cranial arteries, and the other image shows a healthy subject for comparison.|The image on the left: MIP reconstructed MR angiography of a 11 year old girl with Moyamoya Disease. The image on the right: a healthy subject for comparison. |frame]] | ||
It can also be referred to as Progressive Intracranial Occlusive Arteropathy, or Progressive Intracranial Arterial Occlusion. | It can also be referred to as Progressive Intracranial Occlusive Arteropathy, or Progressive Intracranial Arterial Occlusion. | ||
==== Incidence ==== | |||
The incidence of Moyamoya disease is higher in Asia than in Europe, America, Africa and Latin America, with Japan having the highest incidence<ref>Kuriyama S., Kusaka Y., Fujimura M., Wakai K., Tamakoshi A., Hashimoto S., Tsuji I., Inaba Y., Yoshimoto T. Prevalence and clinicoepidemiological features of moyamoya disease in Japan: Findings from a nationwide epidemiological survey. Stroke. 2008;39(1):42–47.</ref> followed by China and South Korea. | |||
== Mechanism of Injury / Pathological Process<br> == | == Mechanism of Injury / Pathological Process<br> == | ||
The affected arteries become increasingly constricted with time, and a collateral circulation develops around the constricted arteries to compensate for the blockages. The condition is | The affected arteries become increasingly constricted with time, and a collateral circulation develops around the constricted arteries to compensate for the blockages. The condition is a non-atherosclerotic progressive vaso-occlusive disease involving the terminal supraclinoid internal carotid arteries and circle of Willis. <br> | ||
== Clinical Presentation == | == Clinical Presentation == | ||
| Line 18: | Line 21: | ||
The patient often presents either: | The patient often presents either: | ||
* in | * in childhood (two-thirds of patients) OR | ||
* in adults in their 30s or 40s (one-third of patients) | * in adults in their 30s or 40s (one-third of patients) | ||
| Line 27: | Line 30: | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
< | Moyamoya Disease was named in 1969 by Suzuki and Takaku<ref>Suzuki J., Takaku A. Cerebrovascular “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch. Neurol. 1969;20(3):288–299.</ref> becuse the appearance on angiography is reminiscent of a "puff of smoke" (the Japanese word moyamoya is tranlated as "something hazy like a puff of smoke") due to the formation of the colateral vessels. | ||
== Outcome Measures == | == Outcome Measures == | ||
Revision as of 19:29, 18 April 2024
Clinically Relevant Anatomy[edit | edit source]
Moyamoya Disease [MMD] is a disorder of some of the blood vessels in the brain: the internal carotid arteries, and the arteries which branch from them, the Circle of Willis[1]. It is a rare cause of Stroke and TIAs.
It can also be referred to as Progressive Intracranial Occlusive Arteropathy, or Progressive Intracranial Arterial Occlusion.
Incidence[edit | edit source]
The incidence of Moyamoya disease is higher in Asia than in Europe, America, Africa and Latin America, with Japan having the highest incidence[2] followed by China and South Korea.
Mechanism of Injury / Pathological Process
[edit | edit source]
The affected arteries become increasingly constricted with time, and a collateral circulation develops around the constricted arteries to compensate for the blockages. The condition is a non-atherosclerotic progressive vaso-occlusive disease involving the terminal supraclinoid internal carotid arteries and circle of Willis.
Clinical Presentation[edit | edit source]
The patient often presents either:
- in childhood (two-thirds of patients) OR
- in adults in their 30s or 40s (one-third of patients)
In children, hemispheric ischaemic strokes are the most common presentation; in adults haemorrhage from the abnormal vessels is more common[3].
Stroke or Transient Ischaemic Attack are the most common presentations, although some patients present with headaches or seizures[4].
Diagnostic Procedures[edit | edit source]
Moyamoya Disease was named in 1969 by Suzuki and Takaku[5] becuse the appearance on angiography is reminiscent of a "puff of smoke" (the Japanese word moyamoya is tranlated as "something hazy like a puff of smoke") due to the formation of the colateral vessels.
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions
[edit | edit source]
add text here relating to management approaches to the condition
Differential Diagnosis
[edit | edit source]
add text here relating to the differential diagnosis of this condition
Resources
[edit | edit source]
add appropriate resources here
References[edit | edit source]
- ↑ Scott R.M., Smith E.R. Moyamoya disease and moyamoya syndrome. N. Engl. J. Med. 2009;360(12):1226–1237.
- ↑ Kuriyama S., Kusaka Y., Fujimura M., Wakai K., Tamakoshi A., Hashimoto S., Tsuji I., Inaba Y., Yoshimoto T. Prevalence and clinicoepidemiological features of moyamoya disease in Japan: Findings from a nationwide epidemiological survey. Stroke. 2008;39(1):42–47.
- ↑ Duan, Lian; Bao, Xiang-Yang; Yang, Wei-Zhong; Shi, Wan-Chao; Li, De-Sheng; Zhang, Zheng-Shan; Zong, Rui; Han, Cong; Zhao, Feng; Feng, Jie (2012). "Moyamoya Disease in China". Stroke. 43 (1): 56–60.
- ↑ Kleinloog, R (May 2012). "Regional differences in incidence and patient characteristics of moyamoya disease: a systematic review". J Neurol Neurosurg Psychiatry. 83 (5): 531–6.
- ↑ Suzuki J., Takaku A. Cerebrovascular “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch. Neurol. 1969;20(3):288–299.