Osteochondritis Dissecans of the Elbow: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox">'''Original Editor '''- [[User:Pamela Gonzalez|Pamela Gonzalez]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} </div> | <div class="editorbox">'''Original Editor '''- [[User:Pamela Gonzalez|Pamela Gonzalez]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} </div> | ||
== Search Strategy == Searched databases : PubMed, PEDRo, Web of Science, Cochrane<br>Search terms : Osteochondritis Dissecans elbow, Osteochondrosis, elbow injury, Osteochondritis physical therapy, Osteochondritis diagnose, Osteochondritis Dissecans capitellum, osteochondritis dissecans elbow physical therapy, osteochondrosis | == Search Strategy == | ||
Searched databases : PubMed, PEDRo, Web of Science, Cochrane<br>Search terms : Osteochondritis Dissecans elbow, Osteochondrosis, elbow injury, Osteochondritis physical therapy, Osteochondritis diagnose, Osteochondritis Dissecans capitellum, osteochondritis dissecans elbow physical therapy, osteochondrosis | |||
== Definition/Description == | |||
An increasingly recognised cause of elbow pain that affects subchondral bone and the overlying cartilage is called Osteochondritis Dissecans (OCD) of the elbow, also known as osteochondrosis of the elbow.<br>OCD can lead to subsequent degenerative arthritis or [http://www.physio-pedia.com/Osteoarthritis osteoarthritis.]<ref name="Steven">Steven A. Giuseffi et al. Osteochondritis dissecans of the elbow. Oper Tech Sport Med 2014; 22; 148-155 (Level of Evidence: 3A)</ref> Osteochondritis dissecans leads to fragmentation and separation of cartilage and underlying bone.<ref name="Champ">Champ L. Baker III et al. Osteochondritis dissecans of the capitellum. American Journal Of Sports Med; 38; 1917-1928 (Level of Evidence: 3A)</ref><br>Osteochondritis Dissecans (OCD) is defined as an inflammatory pathology of bone and cartilage resulting in localised necrosis and fragmentation of bone and cartilage. In the elbow, the most common area affected is the capitellum, although it has been reported in the olecranon and the trochlea.<ref name="Felix">Felix H. Savoie, III, MD; Oper Tech Sports Med 16:187-193 © 2008 Elsevier Inc (Level of Evidence: 2A)</ref> OCD summarised means that there are one or more flakes of articular cartilage that become separated. They will form loose bodies within the joint. The separated flakes stay alive (they are nourished by the synovial fluid) and the flakes often ossify.<ref name="Currey">H.L.F. Currey, Essentials of rheumatology, 1988,p166 (Level of Evidence: 5)</ref><br> [[Image:COCD.jpg|300px]]The cartilage is damaged and can form a loose body<ref name="Moon et al.">Young Lae Moon; Little league elbow; osteochondritis dissecans, 2012 (Level of Evidence : 5)</ref> [[Image:Foto met pijl.jpg]] On the anteroposterior digital radiograph you can see a faint, mobile, irregular, calcific opacity over the distal capitellum.<ref name="Currey" /><ref name="Folio et al.">Les Roger Folio et al., Loose Body in Elbow of a Baseball Player: Arthroscopic/Radiologic Correlation, Radiology case reports, 2006 (Level of Evidence : 3B)</ref> | |||
== Clinically Relevant Anatomy == | |||
Involved anatomy of this disorder includes the radial head or the central and/or lateral aspect of the capitellum. Most OCD lesions of the elbow involve the capitellum, typically the central or lateral portion, but also the radial head, the olecranon of the ulnae and the trochlea humeri.<ref name="Steven" /><br>Also increased activity, loss of motion, and swelling on the lateral side of the elbow comes with increased pain.<ref name="Steven" /><br> | |||
<br> | |||
== Epidemiology / Ethiology == | |||
<br>Ostechondrosis of the humeral capitellum is secondary to repetitive compressive forces between radial head and capitellum. This injury results in a loose body containing an osteochondral bone fragment that is detached from the articular surface. Causes of this pathology include injury or stress on the joint, lack of blood supply, and/or genetic makeup. <br>Repetitive high stress forces on the joint can result in a series of minor injuries on the elbow that can eventually lead to a fracture and ultimately detachment of the bony fragment from the bone.<br>Blockage of a small artery can also be a factor in this pathology. [http://www.physio-pedia.com/Avascular_Necrosis Avascular Necrosis] that leads to the lack of blood supply contributes to break down or death of bone tissue. Osteochondritis dissecans also has a genetic component allowing a predisposition to the pathology.<br> <br> Staging of osteochondritis dissecans is depicted below:<br> Staging of Osteochondritis Dissecans<ref>Champ L. Baker III et al. Osteochondritis dissecans of the capitellum. American Journal Of Sports Med; 38; 1917-1928 (Level of Evidence: 3A)</ref> | |||
Stage Appearance on MRI Stability of Lesion<br> | |||
I Thickening of cartilage and a stable lesion<br> low signal changes | |||
II Articular cartilage interrupted and a stable lesion<br> low signal rim behind fragment <br> showing that there is fibrous <br> attachment | |||
III Articular cartilage interuppted, Unstable<br> high signal changes behind <br> fragment and underlying <br> subchondral bone | |||
IV Loose body Unstable | |||
[[Image:Staging OCD.jpg|350x200px]]<br> <br> This figure shows the different stages of Osteochondritis Dissecans. These vary from stage I to IV as explained above this picture. From left to right we can examine stage I through stage IV. <ref name="Seattle">Seattle children’s hospital; 1995-2015 (Level of Evidence : 5)</ref> | |||
<br> Steven A. Giuseffi et al. believe the trigger is likely multifactorial. A couple of mechanisms that contribute to the development of OCD are: trauma, ischemia, disordered ossification and genetic abnormalities. But these mechanisms are momentarily not universally accepted but may be a contributing factor.<br>From another point of view vascular hypoperfusion and repeated microtrauma may also contribute to the development of OCD. Capillary blood supply is often limited to 1 or 2 end vessels with limited collateral flow. This leads to vascular hypoperfusion. Repeated microtrauma could lead to a production of a relatively avascular state in the vulnerable immature capitellar chondroepiphysis (Level of Evidence: 3A).<ref name="Steven" /><br> <br> | |||
== Characteristics/Clinical Presentation == | |||
<br>Presentation includes pain over the joint, stiffness, feeling of [http://www.physio-pedia.com/Postero-lateral_Elbow_Instability postero-lateral elbow instability] , and stiffness after resting. This commonly affects the knee in a teenager or young adult and the elbow. It presents characteristics of a loose body: locking, giving way and recurrent effusions. <ref name="Curry" /> Complaints of popping, clicking, or sudden “giving way,” are present especially with load bearing.<ref name="Felix" /> | |||
<br> | |||
== Differential Diagnosis == | |||
If there is no radiologic confirmation of Osteochondritis Dissecans, other diagnoses may include inflammatory arthritides inflammatory arthritis, osteoarthritis, bone cysts, and [http://www.physio-pedia.com/Septic_%28Infectious%29_Arthritis septic arthritis.]<br>A lot of other various conditions may seem to be Osteochondritis Dissecans (OCD). These are Panner’s disease, osteonecrosis, osteochondral fracture, hereditary epiphyseal dysplasia and Little Leaguer’s Elbow. <ref name="Steven" /> | |||
== <br>Diagnostic Procedures == | |||
Radiographs can detect any abnormalities on the surface of the joint. If the cartilage flake includes a piece of underlying bone, it can be seen on [http://www.physio-pedia.com/X-Rays X-ray].<ref name="Curry" /> [http://www.physio-pedia.com/MRI_Scans Magnetic Resonance Imaging] (MRI) will show any accumulation of fluid in the area and can detect any loose fragments. Computerized Tomography (CT) can detect any bony fragments, pinpoint their location and determine whether they have settled in the joint space.<br>[[Image:Elbow joint OCD lesion.jpg]] This figure shows an OCD lesion in the distal capitellum of the humeri. this figure shows a stage IV Osteochondritis Dissecans where a loose fragment of cartilage can be examined.<ref name="Curry" /><ref>Singapore Sports and Orthopaedic Clinic, 2014 (Level of Evidence 5)</ref><br> | |||
== <br>Outcome Measures == | |||
An outcome measure appropriate for this injury is the [http://www.physio-pedia.com/DASH_Outcome_Measure DASH questionnaire] which measures disabilities of the arm (under the term arm we can also understand elbow), , shoulder and hand as they relate to everyday function. A modified Andrews elbow scoring system (MAESS) is used to determine specific function of the elbow.<br> | |||
<br> | |||
== Examination == | |||
Physical examination is possible to find radiocapitellar tenderness. Crepitus, decreased elbow extension and an effusion could be occurring. As told above clicking, catching or locking could also occur. These suggest OCD fragment instability and the associated loose bodies. To help confirm the diagnosis of capitellar OCD we can use the active radiocapitellar compression test. The test goes as follows: the examiner places the elbow of the patient in full extension and then he lets the patient actively pronate and supinate the forearm. (Level of Evidence 3A) This test is positive if it results in a compression across the radiocapitellar joint and which evokes lateral joint pain.<ref name="Steven" /> | |||
<br> | |||
== Medical Management == | |||
Surgical management may be an option if conservative care fails or if the lesion is Grade III or higher.<br>Surgical interventions are aimed at:<br>Promoting re-vascularisation to the area<br>Debriding the area<br>Fragment stabilisation<br>Bone grafting if needed<br>Most of these procedures are done arthroscopically (minimally invasive via portal sites), although depending on the size of the loose fragments an open procedure may be required. | |||
<br> | |||
Operative Management<br>The mainstay of the operative management is the removal of the loose fragments and debridement of the base, also the arthroscopic evaluation of the lesion is a part of the treatment. Although most of the older literature was focused on an open management, most of the newest literature delineate the efficacy of arthroscopic surgery. The diagnostic arthroscopy of the anterior compartment of the elbow is the first step for the operative technique (Level of Evidence 2A). The most useful technique is to begin the arthroscopy with the anteromedial portal to visualise the radiocapitellar joint. The anterior part of the capitulum is mostly normal. If we notified a anterior lesion, we can use the 70° arthroscope to visualise the lesion and the lateral portal is used to treat the lesion. The anterior side of the elbow is then evaluated with a camera for loose bodies. If there are loose bodies, they are removed via an anterolateral portal. Also the fossa olecranon is evaluated for loose bodies. If there are loose bodies, they are removed via a posterior central or posterior lateral portal. The medial gutter is also evaluated for loose bodies and inflammation. If there is any inflammation or thickening of the posterolateral plica, they remove it via a posterolateral portal.<ref name="Felix" /> | |||
<br>Arthroscopic surgery can include debridement, fragment fixation, microfracturing and osteochondral autografting. Removing of the fragments alone is a minimally and common invasive procedure. The long-term results can be poor if a large osteochondral defect of the capitulum remains. An alternative procedure is the fragment fixation with a bone graft. It is difficult to fix a cartilaginous fragment securely in unhealthy subchondral bone (Level of Evidence 3A). Recurrent symptoms after a short time span can be expected in these patients. Research show us a gain in ROM about debridement, microfracturing, drilling and creating fibrocartilage. The hyaline cartilage can mostly not be restored with the techniques of treatment of capitellar OCD. The technique that can restore the hyaline cartilage is the osteochondral autografting technique. The negative point of osteochondral autografting is the need to expose the knee joint to fix the graft. But for the elbow the size of the defect is limited. <ref>Frank de Graaff et al., Arthroscopic Surgery in Athletes With Osteochondritis Dissecans of the Elbow, Artrhoscopy, 2011 (Level of Evidence : 3A)</ref><br> <br> | |||
<div><br></div> | |||
== <span> </span>Physical Therapy Management == | |||
Conservative care for this condition include physical therapy, use of non-steroidal anti-inflammatory drugs (NSAIDs), rest from sport for 6-8 weeks, and bracing.<br>Steven A. Giuseffi states that the non-operative treatment of Osteochondritis Dissecans of the elbow still remains controversial. Lesion stability, integrity of the overlying cartilage and status of the capitellar physis are key considerations in determining the appropriate management. Lesions with an intact cartilage surface, i.e. a stable lesion, but also non-displaced lesions with cartilage compromise can be treated using a non-operative management. If an open physis, relatively preserved elbow range of motion (ROM), 20° at most, localised flattening or lucency on radiographs without evidence of defect fragmentation or instability occurs a positive prognosis could be stated. <ref name="Steven" /> <br>This non-operative treatment consists of rest and activity modification, as such that sports and aggravating activities are ceased until symptoms resolve. This usually takes 3 to 12 weeks until the symptoms are resolved. | |||
Steven A. Giuseffi also recommends the use of a hinged brace during the passing time. This protects the elbow and helps correct a natural elbow valgus and will help offload the capitellum. When the patient’s symptoms improve, gentle physical therapy and ROM-exercises could be used. At first, the brace is set at the limits of pain-free range of motion, often as limited as 60 to 90°. The brace is loosened to allow full range of motion, as the inflammation in the plica decreases and pain-free motion increases (Level of Evidence 2A), <ref name="Felix" /> Within 2 weeks from the beginning of treatment, the patient is able to return to normal activities with the brace in place. <ref name="Felix" /> After 3 to 6 months (usually) athletes can return to their sports activities.The patient and family should be advised of potential long-term sequelae.<br>If the patient doesn’t have a stable lesion, operative treatment could be advised. If arthroscopic debridement and drilling was used, non-operative treatment could be used postoperative. The patient will be placed in a double-hinged elbow brace within a week and gentle ROM-exercises could be used. When pain and swelling disappear, the patient may gradually participate in athletic activities in the brace. Full return to athletics could be estimated after 3-4 months. (Level of Evidence 3A) As mentioned above patients and parents should be advised of potential sequelae. <ref name="Steven" /> | |||
The patient can be situated in three phases: acute, recovery and maintenance.<br>During the acute phase the physiotherapist should advise the patient, who have an intact humeral capitellum osteochondritis dissecans lesion, to rest and to limit their activities. He/she should also teach these patients how to apply ice on their elbow. If the patient experiences a lot of pain, the physiotherapist should consider using a hinge brace to relieve this pain and only for this use. Bracing during a long period of time is not indicated as these could increase the risk of flexion contractures. As referred before it’s very important to apply ice, as this relieves the pain. <ref name="Patel">Shital Patel. Humeral Capitellum Osteochondritis Dissecans Treatment &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Management, MedScape. (Level of evidence: 3A)</ref><br>When the patient could be located in the recovery phase, after an intervention, then the physiotherapist can start with passive range-of-motion (ROM) exercises. These can be follow by active ROM exercises, this to avoid contractures. Progressive resistance training should be used as the patient can tolerate more activity and gets stronger. It hasn’t been proven in CT’s (clinical trials) but electrical stimulation may also facilitate recovery. <ref name="Patel" /><br> | |||
The maintenance phase consists of continued use of strengthening and ROM exercises for the elbow. It is also important to prevent further injuries by taking measures protecting the elbow. The physiotherapist could advise patients of the significance of a wrist/finger program and a shoulder program. Strengthening and ROM exercises should also be the main focus during these programs. <ref name="Patel" /><br> | |||
Analytic physiotherapy consists of specific techniques. Those techniques could be used for traumatic osteoarticular pathologies, micro-traumas, functional or postural pathologies. This states that it could be used for inflammatory pathologies as osteochondritis.<br> | |||
The treatment starts with specific mobilisation meaning to release blocked and displaced joints. These mobilisations are calm and progressive. These movements are executed in the initial position, this to evade tension on soft tissue. Researchers express on the demanded cyclic force that should be given. The cyclic force will lead to a normal physiology of chondrocytes. Constant pressure will result in destruction of the cartilage. Switching up the contraction and relaxation of muscles during these techniques is also important. Following these steps will result in regeneration of the articular structures to an optimal state. <ref name="Haye">Michel Haye, La kinésithérapie analytique thérapie manuelle selon le concept de Sohier,Profession Kinésithérapeute, 2007 (Level of evidence: 3A)</ref><br><br> | |||
== Key Evidence == | |||
A study published in 2008 reports a favorable prognosis of up to 90% for patients who are treated conservatively in the stage I of this condition. Patients who were in stage II had about a 53% of a good prognosis with conservative treatment. Duration of this treatment was just under 15 months in the first stage and 13 months in the second stage. About 78% of stage I and 53% of stage II patients were able to return to competitive baseball. Mean ages for these groups were about 12 years in stage I and 14 years of age in stage II. This study is a level III study, and more research should be done to support these results.<br>Another study performed in 2006 looks at the surgical considerations for osteochondritis dissecans. The article looks at 15 patients with a mean age of 28 that underwent elbow arthroscopic debridement for this condition. These patients were classified using the Baumgarten system and were graded during arthroscopy. They looked at the patients about 4 years out of surgery and found a significant decrease in pain levels and function was improved from a “poor” to an “excellent” status per the modified Andrews elbow scoring system. About 80% of these patients were able to return to the same level of sport while all of the patients were able to return to work.<br>Factors that should be considered are age, activity level for the studies above. Clearly more research needs to be done to determine best practice when it comes to treatment of osteochondritis dissecans. | |||
== Resources == | |||
Resources we used for pictures:<br>Fig 1 : https://www.youtube.com/watch?v=sfAxCsv_Hes (12)<br>Fig. 2: http://radiology.casereports.net/index.php/rcr/article/view/18/161 (11)<br>Fig. 3: http://www.seattlechildrens.org/medical-conditions/bone-joint-muscle-conditions/cartilage-conditions/osteochondritis-dissecans/ (16)<br>Fig. 4: http://www.boneclinic.com.sg/patient-education/child-orthopaedics/adolescent-osteochondritis-dissecans/ (17)<br> | |||
Books:<br>H.L.F. Currey,Essentials of rheumatology, 1988, p166 [9]<br><br> | |||
== Clinical Bottom Line == | |||
Osteochondritis Dissecans <ref name="Steven" /> is, in adolescent athletes, an increasingly common cause of elbow dysfunction and elbow pain. [6] It can lead to additional conditions which lead to a complex situation. There are multiple mechanisms that lead to OCD: trauma, ischemia, disordered ossification and genetic abnormalities. What typically happens is that one or more flakes of articular cartilage separates and forms loose bodies within the joint. <ref name="Steven" /> The separated flakes remain alive and frequently ossify. <ref name="Patel" /> Most lesions involve the capitellum, typically the central or lateral portion, but also the radial head, the olecranon of the ulnae and the trochlea humeri. <ref name="Felix" /> OCD can also be caused by a vascular dysfunction or microtrauma. <ref name="Steven" /> Main characteristics of the illness that are commonly mentioned are locking, giving away and recurrent effusions. <ref name="Felix" /> As far as the differential diagnosis goes, we can quote Panner’s disease, osteonecrosis, osteochondral fracture, hereditary epiphyseal dysplasia and Little Leaguer’s Elbow. <ref name="Steven" /> Examination can be done using the active radiocapitellar compression test, in case of lateral joint pain evocation the test is considered positive. <ref name="Steven" /> For medical management, the use of arthroscopic surgery is one of the options. <ref name="Felix" /> As for the physical therapy management it still remains controversial, although there is a vast description of the possibilities described. <ref name="Steven" /> | |||
== Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | |||
<div class="researchbox"><rss>http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1d5iJ1ljAjCoAYm05e0slhzh1Ed8d7b15qso9aqZRVRnYQUAO|charset=UTF-8|short|max=10</rss> http://www.ncbi.nlm.nih.gov/pubmed/25953486<br>http://www.ncbi.nlm.nih.gov/pubmed/20188271<br>http://www.ncbi.nlm.nih.gov/pubmed/25264040<br>http://www.ncbi.nlm.nih.gov/pubmed/24698041<br>http://www.ncbi.nlm.nih.gov/pubmed/24698040<br> </div> | <div class="researchbox"><rss>http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1d5iJ1ljAjCoAYm05e0slhzh1Ed8d7b15qso9aqZRVRnYQUAO|charset=UTF-8|short|max=10</rss> http://www.ncbi.nlm.nih.gov/pubmed/25953486<br>http://www.ncbi.nlm.nih.gov/pubmed/20188271<br>http://www.ncbi.nlm.nih.gov/pubmed/25264040<br>http://www.ncbi.nlm.nih.gov/pubmed/24698041<br>http://www.ncbi.nlm.nih.gov/pubmed/24698040<br> </div> | ||
== References == References will automatically be added here, see [[Adding References|adding references tutorial]]. <ref>Mayo Clinic. Osteochondritis Dissecans. http://www.mayoclinic.com/health/osteochondritis-dissecans/DS00741 (accessed 6/13/09).</ref> <ref>Rahusen F Th G, et al. Results of arthroscopic debridement for osteochondritis dissecans of the elbow. B J Sports Med 2006;40:966-969. Abstract: http://bjsportmed.com/cgi/content/abstract/40/12/966 (accessed 6/25/09).</ref><ref>Matsuura T, et al. Conservative Treatment for Osteochondrosis of the Humeral Capitellum. Am J Sports Med. 2008;36(5): 868-872. Abstract: http://ajs.sagepub.com/content/36/5/868.abstract (accessed 6/18/09).</ref> <ref>O’Sullivan S, Siegelman R. National Physical Therapy Examination Review &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Study Guide. Evanston, IL: International Educational Resources Ltd, 2006.</ref> <ref>Patient UK. http://www.patient.co.uk/showdoc/40001133/ (accessed 6/13/09)</ref> <br> <references /> | == References == | ||
References will automatically be added here, see [[Adding References|adding references tutorial]]. <ref>Mayo Clinic. Osteochondritis Dissecans. http://www.mayoclinic.com/health/osteochondritis-dissecans/DS00741 (accessed 6/13/09).</ref> <ref>Rahusen F Th G, et al. Results of arthroscopic debridement for osteochondritis dissecans of the elbow. B J Sports Med 2006;40:966-969. Abstract: http://bjsportmed.com/cgi/content/abstract/40/12/966 (accessed 6/25/09).</ref><ref>Matsuura T, et al. Conservative Treatment for Osteochondrosis of the Humeral Capitellum. Am J Sports Med. 2008;36(5): 868-872. Abstract: http://ajs.sagepub.com/content/36/5/868.abstract (accessed 6/18/09).</ref> <ref>O’Sullivan S, Siegelman R. National Physical Therapy Examination Review &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Study Guide. Evanston, IL: International Educational Resources Ltd, 2006.</ref> <ref>Patient UK. http://www.patient.co.uk/showdoc/40001133/ (accessed 6/13/09)</ref> <br> <references /> | |||
[[Category:EIM_Residency_Project]] | [[Category:EIM_Residency_Project]] | ||
Revision as of 22:26, 2 June 2016
Search Strategy [edit | edit source]
Searched databases : PubMed, PEDRo, Web of Science, Cochrane
Search terms : Osteochondritis Dissecans elbow, Osteochondrosis, elbow injury, Osteochondritis physical therapy, Osteochondritis diagnose, Osteochondritis Dissecans capitellum, osteochondritis dissecans elbow physical therapy, osteochondrosis
Definition/Description [edit | edit source]
An increasingly recognised cause of elbow pain that affects subchondral bone and the overlying cartilage is called Osteochondritis Dissecans (OCD) of the elbow, also known as osteochondrosis of the elbow.
OCD can lead to subsequent degenerative arthritis or osteoarthritis.[1] Osteochondritis dissecans leads to fragmentation and separation of cartilage and underlying bone.[2]
Osteochondritis Dissecans (OCD) is defined as an inflammatory pathology of bone and cartilage resulting in localised necrosis and fragmentation of bone and cartilage. In the elbow, the most common area affected is the capitellum, although it has been reported in the olecranon and the trochlea.[3] OCD summarised means that there are one or more flakes of articular cartilage that become separated. They will form loose bodies within the joint. The separated flakes stay alive (they are nourished by the synovial fluid) and the flakes often ossify.[4]
 The cartilage is damaged and can form a loose body[5]
The cartilage is damaged and can form a loose body[5]  On the anteroposterior digital radiograph you can see a faint, mobile, irregular, calcific opacity over the distal capitellum.[4][6]
On the anteroposterior digital radiograph you can see a faint, mobile, irregular, calcific opacity over the distal capitellum.[4][6]
Clinically Relevant Anatomy[edit | edit source]
Involved anatomy of this disorder includes the radial head or the central and/or lateral aspect of the capitellum. Most OCD lesions of the elbow involve the capitellum, typically the central or lateral portion, but also the radial head, the olecranon of the ulnae and the trochlea humeri.[1]
Also increased activity, loss of motion, and swelling on the lateral side of the elbow comes with increased pain.[1]
Epidemiology / Ethiology[edit | edit source]
Ostechondrosis of the humeral capitellum is secondary to repetitive compressive forces between radial head and capitellum. This injury results in a loose body containing an osteochondral bone fragment that is detached from the articular surface. Causes of this pathology include injury or stress on the joint, lack of blood supply, and/or genetic makeup.
Repetitive high stress forces on the joint can result in a series of minor injuries on the elbow that can eventually lead to a fracture and ultimately detachment of the bony fragment from the bone.
Blockage of a small artery can also be a factor in this pathology. Avascular Necrosis that leads to the lack of blood supply contributes to break down or death of bone tissue. Osteochondritis dissecans also has a genetic component allowing a predisposition to the pathology.
Staging of osteochondritis dissecans is depicted below:
Staging of Osteochondritis Dissecans[7]
Stage Appearance on MRI Stability of Lesion
I Thickening of cartilage and a stable lesion
low signal changes
II Articular cartilage interrupted and a stable lesion
low signal rim behind fragment
showing that there is fibrous
attachment
III Articular cartilage interuppted, Unstable
high signal changes behind
fragment and underlying
subchondral bone
IV Loose body Unstable
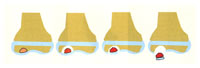
This figure shows the different stages of Osteochondritis Dissecans. These vary from stage I to IV as explained above this picture. From left to right we can examine stage I through stage IV. [8]
Steven A. Giuseffi et al. believe the trigger is likely multifactorial. A couple of mechanisms that contribute to the development of OCD are: trauma, ischemia, disordered ossification and genetic abnormalities. But these mechanisms are momentarily not universally accepted but may be a contributing factor.
From another point of view vascular hypoperfusion and repeated microtrauma may also contribute to the development of OCD. Capillary blood supply is often limited to 1 or 2 end vessels with limited collateral flow. This leads to vascular hypoperfusion. Repeated microtrauma could lead to a production of a relatively avascular state in the vulnerable immature capitellar chondroepiphysis (Level of Evidence: 3A).[1]
Characteristics/Clinical Presentation[edit | edit source]
Presentation includes pain over the joint, stiffness, feeling of postero-lateral elbow instability , and stiffness after resting. This commonly affects the knee in a teenager or young adult and the elbow. It presents characteristics of a loose body: locking, giving way and recurrent effusions. [9] Complaints of popping, clicking, or sudden “giving way,” are present especially with load bearing.[3]
Differential Diagnosis[edit | edit source]
If there is no radiologic confirmation of Osteochondritis Dissecans, other diagnoses may include inflammatory arthritides inflammatory arthritis, osteoarthritis, bone cysts, and septic arthritis.
A lot of other various conditions may seem to be Osteochondritis Dissecans (OCD). These are Panner’s disease, osteonecrosis, osteochondral fracture, hereditary epiphyseal dysplasia and Little Leaguer’s Elbow. [1]
Diagnostic Procedures [edit | edit source]
Radiographs can detect any abnormalities on the surface of the joint. If the cartilage flake includes a piece of underlying bone, it can be seen on X-ray.[9] Magnetic Resonance Imaging (MRI) will show any accumulation of fluid in the area and can detect any loose fragments. Computerized Tomography (CT) can detect any bony fragments, pinpoint their location and determine whether they have settled in the joint space.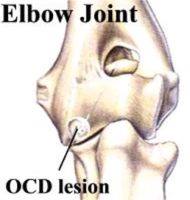 This figure shows an OCD lesion in the distal capitellum of the humeri. this figure shows a stage IV Osteochondritis Dissecans where a loose fragment of cartilage can be examined.[9][10]
This figure shows an OCD lesion in the distal capitellum of the humeri. this figure shows a stage IV Osteochondritis Dissecans where a loose fragment of cartilage can be examined.[9][10]
Outcome Measures [edit | edit source]
An outcome measure appropriate for this injury is the DASH questionnaire which measures disabilities of the arm (under the term arm we can also understand elbow), , shoulder and hand as they relate to everyday function. A modified Andrews elbow scoring system (MAESS) is used to determine specific function of the elbow.
Examination[edit | edit source]
Physical examination is possible to find radiocapitellar tenderness. Crepitus, decreased elbow extension and an effusion could be occurring. As told above clicking, catching or locking could also occur. These suggest OCD fragment instability and the associated loose bodies. To help confirm the diagnosis of capitellar OCD we can use the active radiocapitellar compression test. The test goes as follows: the examiner places the elbow of the patient in full extension and then he lets the patient actively pronate and supinate the forearm. (Level of Evidence 3A) This test is positive if it results in a compression across the radiocapitellar joint and which evokes lateral joint pain.[1]
Medical Management [edit | edit source]
Surgical management may be an option if conservative care fails or if the lesion is Grade III or higher.
Surgical interventions are aimed at:
Promoting re-vascularisation to the area
Debriding the area
Fragment stabilisation
Bone grafting if needed
Most of these procedures are done arthroscopically (minimally invasive via portal sites), although depending on the size of the loose fragments an open procedure may be required.
Operative Management
The mainstay of the operative management is the removal of the loose fragments and debridement of the base, also the arthroscopic evaluation of the lesion is a part of the treatment. Although most of the older literature was focused on an open management, most of the newest literature delineate the efficacy of arthroscopic surgery. The diagnostic arthroscopy of the anterior compartment of the elbow is the first step for the operative technique (Level of Evidence 2A). The most useful technique is to begin the arthroscopy with the anteromedial portal to visualise the radiocapitellar joint. The anterior part of the capitulum is mostly normal. If we notified a anterior lesion, we can use the 70° arthroscope to visualise the lesion and the lateral portal is used to treat the lesion. The anterior side of the elbow is then evaluated with a camera for loose bodies. If there are loose bodies, they are removed via an anterolateral portal. Also the fossa olecranon is evaluated for loose bodies. If there are loose bodies, they are removed via a posterior central or posterior lateral portal. The medial gutter is also evaluated for loose bodies and inflammation. If there is any inflammation or thickening of the posterolateral plica, they remove it via a posterolateral portal.[3]
Arthroscopic surgery can include debridement, fragment fixation, microfracturing and osteochondral autografting. Removing of the fragments alone is a minimally and common invasive procedure. The long-term results can be poor if a large osteochondral defect of the capitulum remains. An alternative procedure is the fragment fixation with a bone graft. It is difficult to fix a cartilaginous fragment securely in unhealthy subchondral bone (Level of Evidence 3A). Recurrent symptoms after a short time span can be expected in these patients. Research show us a gain in ROM about debridement, microfracturing, drilling and creating fibrocartilage. The hyaline cartilage can mostly not be restored with the techniques of treatment of capitellar OCD. The technique that can restore the hyaline cartilage is the osteochondral autografting technique. The negative point of osteochondral autografting is the need to expose the knee joint to fix the graft. But for the elbow the size of the defect is limited. [11]
Physical Therapy Management[edit | edit source]
Conservative care for this condition include physical therapy, use of non-steroidal anti-inflammatory drugs (NSAIDs), rest from sport for 6-8 weeks, and bracing.
Steven A. Giuseffi states that the non-operative treatment of Osteochondritis Dissecans of the elbow still remains controversial. Lesion stability, integrity of the overlying cartilage and status of the capitellar physis are key considerations in determining the appropriate management. Lesions with an intact cartilage surface, i.e. a stable lesion, but also non-displaced lesions with cartilage compromise can be treated using a non-operative management. If an open physis, relatively preserved elbow range of motion (ROM), 20° at most, localised flattening or lucency on radiographs without evidence of defect fragmentation or instability occurs a positive prognosis could be stated. [1]
This non-operative treatment consists of rest and activity modification, as such that sports and aggravating activities are ceased until symptoms resolve. This usually takes 3 to 12 weeks until the symptoms are resolved.
Steven A. Giuseffi also recommends the use of a hinged brace during the passing time. This protects the elbow and helps correct a natural elbow valgus and will help offload the capitellum. When the patient’s symptoms improve, gentle physical therapy and ROM-exercises could be used. At first, the brace is set at the limits of pain-free range of motion, often as limited as 60 to 90°. The brace is loosened to allow full range of motion, as the inflammation in the plica decreases and pain-free motion increases (Level of Evidence 2A), [3] Within 2 weeks from the beginning of treatment, the patient is able to return to normal activities with the brace in place. [3] After 3 to 6 months (usually) athletes can return to their sports activities.The patient and family should be advised of potential long-term sequelae.
If the patient doesn’t have a stable lesion, operative treatment could be advised. If arthroscopic debridement and drilling was used, non-operative treatment could be used postoperative. The patient will be placed in a double-hinged elbow brace within a week and gentle ROM-exercises could be used. When pain and swelling disappear, the patient may gradually participate in athletic activities in the brace. Full return to athletics could be estimated after 3-4 months. (Level of Evidence 3A) As mentioned above patients and parents should be advised of potential sequelae. [1]
The patient can be situated in three phases: acute, recovery and maintenance.
During the acute phase the physiotherapist should advise the patient, who have an intact humeral capitellum osteochondritis dissecans lesion, to rest and to limit their activities. He/she should also teach these patients how to apply ice on their elbow. If the patient experiences a lot of pain, the physiotherapist should consider using a hinge brace to relieve this pain and only for this use. Bracing during a long period of time is not indicated as these could increase the risk of flexion contractures. As referred before it’s very important to apply ice, as this relieves the pain. [12]
When the patient could be located in the recovery phase, after an intervention, then the physiotherapist can start with passive range-of-motion (ROM) exercises. These can be follow by active ROM exercises, this to avoid contractures. Progressive resistance training should be used as the patient can tolerate more activity and gets stronger. It hasn’t been proven in CT’s (clinical trials) but electrical stimulation may also facilitate recovery. [12]
The maintenance phase consists of continued use of strengthening and ROM exercises for the elbow. It is also important to prevent further injuries by taking measures protecting the elbow. The physiotherapist could advise patients of the significance of a wrist/finger program and a shoulder program. Strengthening and ROM exercises should also be the main focus during these programs. [12]
Analytic physiotherapy consists of specific techniques. Those techniques could be used for traumatic osteoarticular pathologies, micro-traumas, functional or postural pathologies. This states that it could be used for inflammatory pathologies as osteochondritis.
The treatment starts with specific mobilisation meaning to release blocked and displaced joints. These mobilisations are calm and progressive. These movements are executed in the initial position, this to evade tension on soft tissue. Researchers express on the demanded cyclic force that should be given. The cyclic force will lead to a normal physiology of chondrocytes. Constant pressure will result in destruction of the cartilage. Switching up the contraction and relaxation of muscles during these techniques is also important. Following these steps will result in regeneration of the articular structures to an optimal state. [13]
Key Evidence[edit | edit source]
A study published in 2008 reports a favorable prognosis of up to 90% for patients who are treated conservatively in the stage I of this condition. Patients who were in stage II had about a 53% of a good prognosis with conservative treatment. Duration of this treatment was just under 15 months in the first stage and 13 months in the second stage. About 78% of stage I and 53% of stage II patients were able to return to competitive baseball. Mean ages for these groups were about 12 years in stage I and 14 years of age in stage II. This study is a level III study, and more research should be done to support these results.
Another study performed in 2006 looks at the surgical considerations for osteochondritis dissecans. The article looks at 15 patients with a mean age of 28 that underwent elbow arthroscopic debridement for this condition. These patients were classified using the Baumgarten system and were graded during arthroscopy. They looked at the patients about 4 years out of surgery and found a significant decrease in pain levels and function was improved from a “poor” to an “excellent” status per the modified Andrews elbow scoring system. About 80% of these patients were able to return to the same level of sport while all of the patients were able to return to work.
Factors that should be considered are age, activity level for the studies above. Clearly more research needs to be done to determine best practice when it comes to treatment of osteochondritis dissecans.
Resources[edit | edit source]
Resources we used for pictures:
Fig 1 : https://www.youtube.com/watch?v=sfAxCsv_Hes (12)
Fig. 2: http://radiology.casereports.net/index.php/rcr/article/view/18/161 (11)
Fig. 3: http://www.seattlechildrens.org/medical-conditions/bone-joint-muscle-conditions/cartilage-conditions/osteochondritis-dissecans/ (16)
Fig. 4: http://www.boneclinic.com.sg/patient-education/child-orthopaedics/adolescent-osteochondritis-dissecans/ (17)
Books:
H.L.F. Currey,Essentials of rheumatology, 1988, p166 [9]
Clinical Bottom Line [edit | edit source]
Osteochondritis Dissecans [1] is, in adolescent athletes, an increasingly common cause of elbow dysfunction and elbow pain. [6] It can lead to additional conditions which lead to a complex situation. There are multiple mechanisms that lead to OCD: trauma, ischemia, disordered ossification and genetic abnormalities. What typically happens is that one or more flakes of articular cartilage separates and forms loose bodies within the joint. [1] The separated flakes remain alive and frequently ossify. [12] Most lesions involve the capitellum, typically the central or lateral portion, but also the radial head, the olecranon of the ulnae and the trochlea humeri. [3] OCD can also be caused by a vascular dysfunction or microtrauma. [1] Main characteristics of the illness that are commonly mentioned are locking, giving away and recurrent effusions. [3] As far as the differential diagnosis goes, we can quote Panner’s disease, osteonecrosis, osteochondral fracture, hereditary epiphyseal dysplasia and Little Leaguer’s Elbow. [1] Examination can be done using the active radiocapitellar compression test, in case of lateral joint pain evocation the test is considered positive. [1] For medical management, the use of arthroscopic surgery is one of the options. [3] As for the physical therapy management it still remains controversial, although there is a vast description of the possibilities described. [1]
Recent Related Research (from Pubmed)[edit | edit source]
http://www.ncbi.nlm.nih.gov/pubmed/20188271
http://www.ncbi.nlm.nih.gov/pubmed/25264040
http://www.ncbi.nlm.nih.gov/pubmed/24698041
http://www.ncbi.nlm.nih.gov/pubmed/24698040
References[edit | edit source]
References will automatically be added here, see adding references tutorial. [14] [15][16] [17] [18]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 Steven A. Giuseffi et al. Osteochondritis dissecans of the elbow. Oper Tech Sport Med 2014; 22; 148-155 (Level of Evidence: 3A)
- ↑ Champ L. Baker III et al. Osteochondritis dissecans of the capitellum. American Journal Of Sports Med; 38; 1917-1928 (Level of Evidence: 3A)
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 Felix H. Savoie, III, MD; Oper Tech Sports Med 16:187-193 © 2008 Elsevier Inc (Level of Evidence: 2A)
- ↑ 4.0 4.1 H.L.F. Currey, Essentials of rheumatology, 1988,p166 (Level of Evidence: 5)
- ↑ Young Lae Moon; Little league elbow; osteochondritis dissecans, 2012 (Level of Evidence : 5)
- ↑ Les Roger Folio et al., Loose Body in Elbow of a Baseball Player: Arthroscopic/Radiologic Correlation, Radiology case reports, 2006 (Level of Evidence : 3B)
- ↑ Champ L. Baker III et al. Osteochondritis dissecans of the capitellum. American Journal Of Sports Med; 38; 1917-1928 (Level of Evidence: 3A)
- ↑ Seattle children’s hospital; 1995-2015 (Level of Evidence : 5)
- ↑ 9.0 9.1 9.2 Cite error: Invalid
<ref>tag; no text was provided for refs namedCurry - ↑ Singapore Sports and Orthopaedic Clinic, 2014 (Level of Evidence 5)
- ↑ Frank de Graaff et al., Arthroscopic Surgery in Athletes With Osteochondritis Dissecans of the Elbow, Artrhoscopy, 2011 (Level of Evidence : 3A)
- ↑ 12.0 12.1 12.2 12.3 Shital Patel. Humeral Capitellum Osteochondritis Dissecans Treatment &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Management, MedScape. (Level of evidence: 3A)
- ↑ Michel Haye, La kinésithérapie analytique thérapie manuelle selon le concept de Sohier,Profession Kinésithérapeute, 2007 (Level of evidence: 3A)
- ↑ Mayo Clinic. Osteochondritis Dissecans. http://www.mayoclinic.com/health/osteochondritis-dissecans/DS00741 (accessed 6/13/09).
- ↑ Rahusen F Th G, et al. Results of arthroscopic debridement for osteochondritis dissecans of the elbow. B J Sports Med 2006;40:966-969. Abstract: http://bjsportmed.com/cgi/content/abstract/40/12/966 (accessed 6/25/09).
- ↑ Matsuura T, et al. Conservative Treatment for Osteochondrosis of the Humeral Capitellum. Am J Sports Med. 2008;36(5): 868-872. Abstract: http://ajs.sagepub.com/content/36/5/868.abstract (accessed 6/18/09).
- ↑ O’Sullivan S, Siegelman R. National Physical Therapy Examination Review &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Study Guide. Evanston, IL: International Educational Resources Ltd, 2006.
- ↑ Patient UK. http://www.patient.co.uk/showdoc/40001133/ (accessed 6/13/09)






