Pain Neuroscience Education (PNE): Difference between revisions
Becky Mead (talk | contribs) No edit summary |
Becky Mead (talk | contribs) No edit summary |
||
| Line 129: | Line 129: | ||
<br> | <br> | ||
==== | ==== Patient's experiences of Low Back Pain ==== | ||
{{#ev:youtube|a9f6VJtls2E}}<br> | {{#ev:youtube|a9f6VJtls2E}}<br> | ||
==== Diagram of alarm systems (can be a hand drawn and in a simple video format with narration or just images with text) ==== | ==== Diagram of alarm systems (can be a hand drawn and in a simple video format with narration or just images with text) ==== | ||
Revision as of 23:11, 14 January 2016
What is Pain Neuroscience Education (PNE)?[edit | edit source]
Pain Neuroscience education (PNE) consists of educational sessions for patients describing in detail the neurobiology and neurophysiology of pain and pain processing by the nervous system (Louw et al., 2011). This educational approach has been used by physiotherapists therapeutically since 2002 in various countries including the UK, US and Australia and differs considerably from traditional education strategies such as back school and biomechanical models (find reference). This is due to how likelihood of pain chronicity (e.g. for an MSK condition) may not likely be caused by unhealthy or dysfunctional tissues but brain plasticity leading to hyper-excitability of the central nervous system, known as central sensitisation (Nijs et al., 2015). Therefore, a deeper level reasoning and treatments beyond a medical model is required.
Initially, PNE changes a patient’s perception of pain. For example, a patient may have believed that damaged tissues were the main cause for their pain, and by receiving education about pain neurophysiology the patient understands that pain may not correctly represent the health of the tissue, but may be due to extra-sensitive nerves. As a result, patients have been found to have a reduction in fear avoidance behaviours and are more able and willing to move. PNE can be used with a combination of treatments, including exercise therapy that can be used to break down movement-related pain memories with graded exposure to exercise and decrease sensitivity of the nervous system (Nijs et al., 2015).
What does PNE consist of / involve?[edit | edit source]
PNE first of all puts the complex process of describing the nerves and brain into a format that is easy to understand for everyone; no matter whether the target audience is of a particular age, educational level or ethnic group. This is made possible by using simplified scientific language used with additional methods of presenting information that may include the use of:
• Simple pictures
• Examples
• Booklets
• Metaphors
• Drawings
• Workbook with reading/question-answer assignments
• Neurophysiology Pain Questionnaires
Methods of PNE delivery vary but can typically involve around 4 hours of teaching that is provided to a group or individually, either in single or multiple sessions (Clarke et al., 2011).
(Louw et al., 2011) states the content of PNE education sessions with patients in 4 studies consisted of:
• Neurophysiology of pain
• Nociception and nociceptive pathways
• Neurons
• Synapses
• Action potential
• Spinal inhibition and facilitation
• Peripheral sensitization
• Central sensitization
• Plasticity of the nervous system
How is PNE used in clinical practice?[edit | edit source]
Below is an example of how a story / metaphor used by Louw et al., 2011 is used in clinical practice to teach patients about complex pain physiology including extra-sensitive nerves, inflammation, injury and made how pain is created in the brain. It is such an example that helps patient to break away from a view of a particular tissue being the issue (e.g. generative disc) and helps the patient think towards the problem being related to pain and a sensitive nervous system (Louw et al., 2011). Therefore, Instead of pain following spinal surgery being seen as the ‘problem has not resolved’ or ‘there is something still wrong with the disc’, PNE would explain pain is sensitive to act as a protector which is perfectly normal after surgery.
Scenario of PNE used in clinical practice:
Suzy is experiencing pain and believes her pain is due to a bad disc. However, the pain has been there for 10 years. It is well established that discs reabsorb between 7-9 months and completely heal. So, why would it still hurt? She believes (as she has been told by clinicians) that her pain is caused by a bad disc. Now, we start explaining complex pain issues via a story/metaphor with the aim to change her beliefs, and then we set a treatment plan in place based on the new, more accurate neuroscience view of pain.
Therapist: “If you stepped on a rusted nail right now, would you want to know about it?”
Patient: “Of course.”
Therapist: “Why?”
Patient: “Well; to take the nail out of my foot and get a tetanus shot.”
Therapist: “Exactly. Now, how do you know there’s a nail in your foot? How does the nail get your attention?”
Therapist: “The human body contains over 400 nerves that, if strung together, would stretch 45 miles. All of these nerves have a little bit of electricity in them. This shows you’re alive. Does this make sense?”
Patient: “Yes.”
Therapist: “The nerves in your foot are always buzzing with a little bit of electricity in them. This is normal and shows….?”
Patient: “I’m alive.”
Therapist: “Yes. Now, once you step on the nail, the alarm system is activated. Once the alarm’s threshold is met, the alarm goes off, sending a danger message from your foot to your spinal cord and then on to the brain. Once the brain gets the danger message, the brain may produce pain. The pain stops you in your tracks, and you look at your foot to take care of the issue. Does this sound right?”
Patient: “Yes.”
Therapist: “Once we remove the nail, the alarm system should…?”
Patient: “Go down.”
Therapist: “Exactly. Over the next few days, the alarm system will calm down to its original level, so you will still feel your foot for a day or two. This is normal and expected."
Therapist: “Here’s the important part. In one in four people, the alarm system will activate after an injury or stressful time, but never calm down to the original resting level. It remains extra sensitive. With the alarm system extra sensitive and close to the “firing level,” it does not take a lot of movement, stress or activity to activate the alarm system. When this happens, surely you think something MUST be wrong. Based on your examination today, I believe a large part of your pain is due to an extra-sensitive alarm system. So, instead of focusing of fixing tissues, we will work on a variety of strategies to help calm down your alarm system, which will steadily help you move more, experience less pain and return to previous function."
Indicators for the use of PNE[edit | edit source]
Low Back Pain
Low back pain (LBP) is currently considered to be the most common cause of disability and time off work in the over 45 age group, with it being reported that 84% people will experience LBP at some point during their life (Balagué et al., 2012). Whilst LBP is generally considered a self-limiting condition it can have severe implications to the patient’s psychological and physical health. Results from a UK survey, analysing the consultation prevalence for LBP showed that 417 per 10 000 registered patients sought medical help for their LBP, with the highest numbers being seen in the 45- 64 age group (536 per 10 000) (Jordan et al., 2010). Furthermore an Australian cohort study discovered whilst most patient’s recovered 1/3 had not fully recovered after 1 year (Henschke et al., 2008). LBP is clearly a substantial problem for both the health system and the socioeconomic environment, thus effective management is critical.
Updated NICE guidelines for Chronic LBP states that information and self-care advice should be provided to patients to promote self-management by fostering a positive attitude and providing realistic expectations to patients. However the type, duration, frequency and content of this advice was not reported on (NICE, 2015).
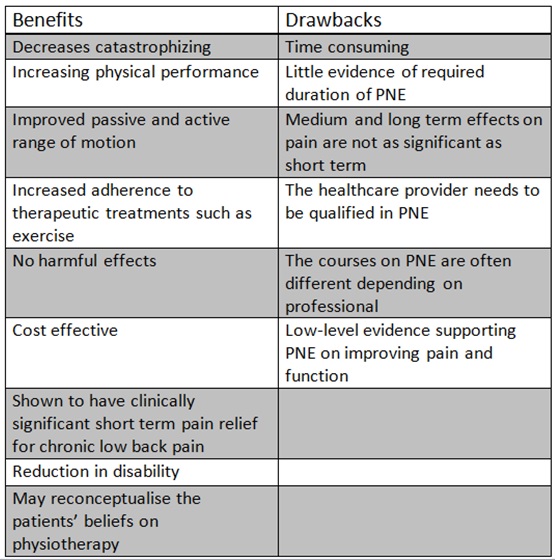
The benefits and drawbacks of PNE[edit | edit source]
Brain activity clinical imaging of PNE effect[edit | edit source]
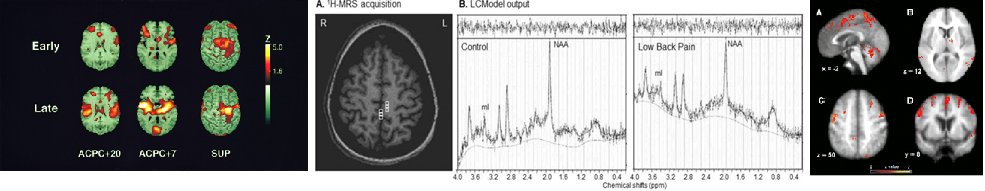
There are various types of brain imaging including those pictured below:
Figure ?. Pictured left to right are Positron emission tomography (PET), magnetic resonance spectroscopy (MRS) and functional magnetic resonance imaging (fMRI) of pain. (Sharma, Brooks, Popescu et al., 2012; Cole, Farrell, Duff et al., 2006; Casey, Morrow, Lorenz et al., 2001).
Effects of therapeutic neuroscience education
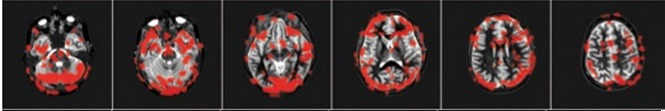
By teaching a patient more about how pain works with reassurance that pain doesn’t always mean tissue damage, their pain eases considerably and they experience other benefits including increased movement, better function and reduced fear avoidance. These effects are measurable via brain imaging as demonstrated below:
A high-level dancer experiencing significant back pain for almost two years who was scheduled for back surgery in two days was scanned using fMRI. Areas of brain activity related to pain are demarcated in red.
Row 1: Patient relaxing. Note no red areas. 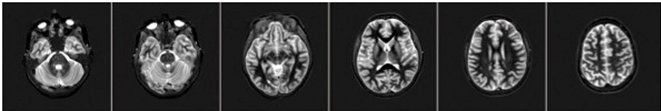
Row 2: Patient was asked her to move her painful back while in scanner. These images demonstrated brain activity related to pain whereby larger areas of red signifies more pain.
Row 3: After initial scans the patient taken out of the scanner and provided with a teaching session of 20-25 minutes about pain. The scan of the patient was immediately repeated doing the same painful task as performed in Row 2. Note this time, however, there is significantly less activity (fewer red areas), while doing the same painful task as before.
(Louw A, et. al 2014 – submitted for publication)
There is an obvious link in attention to pain that when negatively perceived, impacts on the experience of pain being greater. One study by Cole, Farrell and Duff et al., (2006) demonstrated that pain related brain activity was greater in pts with Alzheimer’s, than age matched healthy controls. However, in this population there is less reporting of pain and analgesic use. Is this due to difficulty to communicate pain or due to reduced attention to pain?
Training / education of therapists to use it[edit | edit source]
History of pain models and devlopment of PNE[edit | edit source]
Where has PNE developed from?
The biomedical model is most commonly used by physiotherapists and other medical health professionals for the management of pain (Louw, 2014 & Linton, 2005). The model follows that pain and injury interrelated, thus an increase in pain means further tissue damage have occurred (Louw, 2014) and vice-versa. This model, called the Cartesian model, is over 450 years old, and many argue inaccurate and significantly outdated (Louw, 2014).
Cartesian Model
Why is the model considered outdated?
Descartes model continues to be used in current medical practice and influences the perception that all pain is a result of injury and tissue damage (Linton, 2005). Clinicians frequently use the biological model to explain patient’s pain, describing pain as being due to either disc, joint or abnormal movement pattern (Louw, 2014). The resulting treatment is therefore focused on addressing the abnormal movement pattern or faulty tissue, and the pain goes away. However research has shown that education using words such as “bulging”, “herniated” and “ruptured” actually increases patient's levels of fear and anxiety, resulting in protected movements and lack of exercise compliance (Louw, 2014).
However Descartes biomedical model has been questioned in recent years, with critics arguing that it fails to consider the perception of pain from the nervous system, as well as the psychological and social factors that may influence recovery (Linton, 2005). Furthermore both psychiatrists and behavioural scientists have highlighted specific medical examples to further question the validity of Descartes model. The examples below suggest that pain may potentially be a phenomenon more than just nociception, and may have a neurological element:
- Pain was not expressed by a soldier injured in war until reaching the hospital (Goldberg, 2008)
- Similar injuries in different patients caused substantially different pain responses (Goldberg, 2008)
- An incision to the skin twice as deep as that of another, does not hurt twice as much (Goldberg, 2008)
- Why 40% of people with horrific injuries felt either no or a low intensity of pain (Melzack, Wall & Ty. 1982)
- Why up to 70% of people's do not report pain or associated symptoms consistent with their X-ray/ MRI finding (Bhattacharyya et al., 2003; Boden et al., 1990)
- Why 51% of amputees reported phantom pain and 76% phantom sensations including: cold, electric sensations and movement in the phantom limb (Kooijmana, 2000).
Furthermore in Beecher’s (1956) comparison study of 150 male civilian patients in contrast to wartime casualties, it was discovered that 83% in the civilian group requested narcotics, whilst only 32% of military patients with the same extent of tissue damage asked for them; thereby suggesting the level of pain experienced is patient dependant. In this example it was proposed the patient's emotions, beliefs and experiences of pain altered the brains interpretation of the pain, resulting in different intensities of pain being experienced.
The Pain-neuroscience education model
In the last century Descartes biomedical model has been replaced by the biopsychosocial model of chronic pain (Goldberg, 2008), in which pain is classified as being due to increased sensitivity of the nervous system rather than further injury (Louw, 2014). In layman’s terms, pain persists after tissue healing, due to the fact that the body’s alarm system remains activated, and are stimulated by a much lower intensity of stimulus (Louw, 2014); i.e. a much lower degree of movement provocation causes pain.
How does this affect clinicians in practice?
Investigations by the Therapeutic Neuroscience research team at the ‘International Spine and Pain Institute’ has discovered that people in pain are interested in pain and more specifically the mechanisms of pain (Louw, Louw & Crous, 2009). Thus current treatment for patients with chronic pain should have a greater focus on educating patients about the neuroscience of their pain, rather than classifying their pain as being due to faulty movement patterns or damaged tissues.
Section 1 – Scenarios to aid learning and clinical relevance:[edit | edit source]
Patient's experiences of Low Back Pain[edit | edit source]
Diagram of alarm systems (can be a hand drawn and in a simple video format with narration or just images with text)[edit | edit source]
[edit | edit source]
Section 3 – Evidence[edit | edit source]
[edit | edit source]
Paper 1:
A recent systematic review investigating the effects of pain neuroscience education (PNE) on pain, disability and anxiety, discovered that PNE was an effective therapeutic tool for patients with chronic musculoskeletal pain. Although the review searched all major databases over a 10 year period, only 8 studies (6 RCT’s, 1 pseudo-RCT and 1 comparative study) satisfied the inclusion criteria and were included in the review. The methodological quality of these studies was assessed using the Critical Review Form–Quantitative Studies criteria and the CONSORT checklist, with all included studies deemed to have either good, very good or excellent quality. The review included 401 patients, finding that PNE was significantly more effective at decreasing pain (P<0.01), pain catastrophization (P< 0.001) and perceived disability (P<0.01) compared to the control group (receiving only ongoing medical care), in both the short-term and long-term. Furthermore both one-on-one and group sessions significantly decreased pain and disability (P<0.05), however one-to-one sessions were found to be the more favourable delivery method (P<0.004). Nevertheless results from the review failed to discover the most effective frequency and duration of PNE sessions, with RCT’s reporting sessions lasting for 30minutes to 4 hours, with either a single sessions or multiple sessions being reported effective by clinicians. Moreover the review considered all types of chronic musculoskeletal pain including: Whiplash, Chronic Fatigue syndrome, widespread pain and Chronic Low Back Pain (LBP), thus may lack the generalisability to this article considering PNE for the treatment of LBP.
Paper 2:
Compared to the previous systematic review’s poor generalisability of PNE for a range of chronic pain conditions, researchers in this multi-centred randomised control trial focused solely on Preoperative Pain Neuroscience Education for Lumbar Radiculopathy by Louw et al., (2014).
This study involved 7 sites in the United States (US) and a sample of patients awaiting lumbar surgery for radiculopathy with follow-up over a year. An exclusion criteria was justified to avoid variables in the population (e.g. other chronic pain conditions). Primary outcomes consisted of pain, leg pain and function. Secondary outcomes comprised of experience of lumbar surgery (5 x 1 – 10 Likert scale questions) and health utilisation (questionnaire). 67 patients were randomised to one of two groups: usual care (preoperative education) and experimental group (usual care and PNE preoperatively). Results found that at 1-year follow-up there were no statistical differences in primary outcomes. However, there were significant statistical differences in favour of the PNE group across all secondary outcomes; with patients feeling better prepared for surgery (p<0.001), preoperative session preparing them for surgery (p<0.001) and surgery meeting their expectations (P<0.021). Also, reduced health utilisation in PNE group (p=0.007), resulting in 45% less health expenditure compared to usual care group.
The internal validity of the study is positive with measures in place to reduce risk of bias where possible. Methodological quality could have only improved through blinding but is not appropriate for the groups. The study scored a Pedro scale of 8/11. The secondary outcomes improving patient experiences after surgery and health utilisation are hugely clinically relevant, especially in relation to the financial challenges of National Health Service (NHS) in the UK. Any reduction in services post-surgery and thus reducing costs, whilst additionally improving patient experiences with minimal cost to implement cannot be overlooked. However, the UK’s NHS and health insurance systems in the US will differ dramatically in relation to resources available and how often treatments can be accessed. Subsequently, this study did not control the amount of rehabilitation patients were allowed to access, which could further skew results of outcomes, especially compared to the UK where amount of rehabilitation will be determined by post-operative protocol. Finally, the generalisability of the findings to another type of surgery, e.g. spinal fusion, must be applied with caution despite promising outcomes due to the specificity of the results to surgery for radiculopathy.
Paper 3:
With regard to the concerns of generalising the results from the previous RCT to non-specific low back pain patients, a systematic review and meta-analysis by Clarke, Ryan and Martin 2011, investigated the impact of PNE, specifically on that management of patients with chronic low back pain.
Outcome measures included pain, physical-function, psychological function and social function. The characteristics of the subjects were adults (≥ 18 year) in which at least 50% of the patients had non-specific CLBP. Trials with possible serious spinal pathology were excluded. Two moderate quality RCT’s were included. The meta-analysis found PNE produced statistically significant but clinically small improvements in short-term pain. The reviewers found improvements in all other outcomes but they were not clinically significant, so therefore, due to this and the small number of studies, clinical recommendations cannot be made until further research
The limitations of this review, as critically appraised using the JBI checklist, were the small number of studies included in the review and furthermore, both studies included were published by one of the co-authors of the PNE manual, so there is a potential conflict of interest. There also could have been a wider range of resources used to search for studies as only 3 databases were observed.
However, the critical appraisal of the papers selected was independently assessed by 2 reviewers, minimising bias and each RCT was assessed using the Cochrane back review group (CBRG) guidelines.Contrary to the previous systematic review by Louw and Butler 2011 which focused on a range of chronic conditions, this review is specific to CLBP which make it more generalizable. Lastly the implications for practice and research were based primarily on the reported data.
Paper 4:
Clinical bottom line:[edit | edit source]
==== Referances: ==== 1. Beecher HK. (1956). The frequency of pain severe enough to require a narcotic was studied in 150 male civilian patients and contrasted with similar data from a study of wartime casualties. Efforts were made to have the. Journal of the American Medical Association. 161 (17), 1609-13.
2. Bhattacharyya T, Gale D, Dewire P, Totterman S, Gale ME, McLaughlin S, Einhorn TA, Felson DT. (2003). The clinical importance of meniscal tears demonstrated by magnetic resonance imaging in osteoarthritis of the knee. Journal of Bone and Joint Surgery American volume. 85-A (1), 4-9.
3. Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. (1990). Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation.. Journal of Bone and Joint Surgery American volume. 72 (3), 403-8.
4. Goldberg JS. (2008). Revisiting the Cartesian model of pain. Medical Hypotheses. 70 (5), 1029–1033.
5. Keller T and Krames ES. (2009). “On the Shoulders of Giants”: A History of the Understandings of Pain, Leading to the Understandings of Neuromodulation. Neuromodulation. 12 (2), 77-84.
6. Kooijmana CM, Dijkstraa PU, Geertzena JHB, Elzingad A, van der Schansa CP . (2000). Phantom pain and phantom sensations in upper limb amputees: an epidemiological study. Pain. 87 (1), 33–41.
7. Linton SJ. (2005). Models of pain perception. Understanding Pain for Better Clinical Practice: A Psychological Perspective. Elsevier . 9-18.
8. Louw A, Louw Q & Crous LC. (2009). Preoperative education for lumbar surgery for radiculopathy. South African Journal of Physiotherapy, 65(2), 3-8.
9. Louw A. (2014). Therapeutic Neuroscience Education: Teaching People About Pain. Available: http://www.instituteforchronicpain.org/treating-common-pain/what-is-pain-management/therapeutic-neuroscience-education. Last accessed 6th Janurary 2016.
10. Melzack R, Wall PD & Ty TC. (1982). Acute pain in an emergency clinic: latency of onset and descriptor patterns related to different injuries..Pain. 14 (1), 33-43.
11. Jordan KP, Kadam UT, Hayward R, Porcheret M, Young C, Croft P. (2010). Annual consultation prevalence of regional musculoskeletal problems in primary care: an observational study. BMC Musculoskeletal disorders. 11 (144).
12. Balagué F, Mannion AF, Pellisé F, Cedraschi C. (2012). Non-specific low back pain. The Lancet. 4 (379), 482-91.
13. Henschke N, Maher CG, Refshauge KM, Herbert RD, Cumming RG, Bleasel J, York J, Das A, McAuley JH. (2008). Prognosis in patients with recent onset low back pain in Australian primary care: inception cohort study. BMJ. 337 (a171).
14. National Institute for Health and Clinical Excellence (2015) Back pain - low (without radiculopathy). Clinical Knowledge Summary. London: NICE.
*Summary:
*Concise summary or key points of the page.
*Resources and useful links: #Podcasts Chews health podcast SESSION 4 – KNOW PAIN: METAPHORIC EXPRESSION WITH MIKE STEWART – PART 1, PART 2 Know Pain course: A Practical guide for Therapeutic Neuroscience Education, course provider discussion #Youtube videos Lorimer Moseley Pain - How to Explain Pain to Patients youtube video #Books #Research #Website #Other Membership required. Link: www.csp.org.uk/icsp/topics/neuroscience-based-pain-education-resounding-success-or-damp-squib Know Pain course: A Practical guide for Therapeutic Neuroscience Education, course provider discussion (transcription) Explain Pain – Patient Leaflet
*Conclusion of entire page.
*Resources
*References: