Plantar Grasp Reflex: Difference between revisions
No edit summary |
(added new information, references and images) |
||
| Line 1: | Line 1: | ||
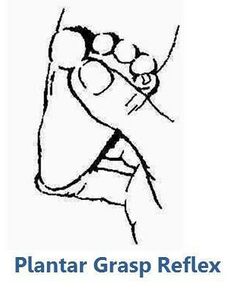
<div class="editorbox"> '''Original Editor '''- [[User:Ahmed Essam|Ahmed Essam]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | <div class="editorbox"> '''Original Editor '''- [[User:Ahmed Essam|Ahmed Essam]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}[[File:Plantar Grasp Reflex.jpg|right|frameless|209x209px]] | ||
== Introduction == | |||
[https://europepmc.org/books/NBK553125/figure/article-22413.image.f2/?report=objectonly][[File:Plantar Grasp Reflex.jpg|right|frameless|290x290px]] | |||
== Introduction == | |||
This reflex in human infants can be regarded as a rudiment of responses that were once essential for ape infants in arboreal life. The '''spinal center''' for this reflex is probably located at the '''L5-S2 levels''', which, however, are controlled by higher brain structures. Nonprimary motor areas may exert regulatory control of the spinal reflex mechanism through interneurons. In infants, this reflex can be elicited as the result of insufficient control of the spinal mechanism by the immature brain. In adults, lesions in nonprimary motor areas may cause a release of inhibitory control by spinal interneurons, leading to a reappearance of the reflex.<ref name=":0">Futagi Y, Suzuki Y. Neural mechanism and clinical significance of the plantar grasp reflex in infants. Pediatric neurology. 2010 Aug 1;43(2):81-6.</ref> | |||
</div> | |||
== Position == | == Position == | ||
Infant lying on a flat surface in the supine position while awake, head and arms at the neutral position. <ref name=":1">Futagi Y, Suzuki Y, Goto M. Clinical significance of plantar grasp response in infants. Pediatric Neurology. 1999 Feb 1;20(2):111-5.</ref><ref name=":2">Prechtl H, Beinthema D. Reflexes and responses: The neurological examination of the full-term newborn infant. Clin Dev Med. 1977;63:40-2.</ref><ref name=":3">Touwen B. Reactions and responses: neurological development in infancy. Clinics in Developmental Medicine. 1976;58:83-98.</ref><ref name=":4">Schott JM, Rossor MN. The grasp and other primitive reflexes. Journal of Neurology, Neurosurgery & Psychiatry. 2003 May 1;74(5):558-60.</ref><ref name=":0" /> | |||
Care should be taken to keep the subject’s head facing the midline, to avoid the influence of the asymmetric tonic neck reflex.<ref name=":0" /> | |||
== Stimulus == | == Stimulus == | ||
The | The plantar reflex is elicited:- | ||
# By pressing a thumb against the sole of the foot just behind the toes.<ref name=":0" /><ref name=":1" /><ref name=":2" /><ref name=":3" /><ref name=":4" /> OR | |||
# By stroking gently the plantar surface medially with a blunt object such as the handle of a reflex hammer.<ref name=":5">Walker HK. The suck, snout, palmomental, and grasp reflexes. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. 1990.</ref> | |||
== Response == | == Response == | ||
=== Normal Response === | |||
'''''In Infants'''''-The lateral surfaces of the foot bend as if to make a cup out of the plantar surface.<ref name=":5" /> It consists of the flexion and adduction of all toes as if the toes were firmly grasping the stimulating object<ref name=":6">BRAIN WR, CURRAN RD. The grasp-reflex of the foot. Brain. 1932 Sep 1;55(3):347-56.</ref>; there is hollowing of the sole with some wrinkling of the skin. If the toes also flex, this is called the tonic foot response.<ref name=":5" /> It is tonic in character, because the posture is often maintained for 15 or 30 seconds, or longer during early infancy<ref name=":6" /> | |||
'''''In adults'''''- no response - as it diminishes in later life. | |||
=== Abnormal Response === | |||
'''''In Infants-''''' No response means there is underlying pathology. | |||
'''''In adults-''''' If flexion or adduction of toes occurs it means there is underlying pathology. | |||
== Clinical significance == | |||
The plantar grasp reflex in infants is of high clinical significance. A negative or diminished reflex during early infancy is often a sensitive indicator of spasticity. Infants with athetoid type cerebral palsy exhibit extremely strong retention of the reflex, and infants with mental retardation also exhibit a tendency toward prolonged retention of the reflex.<ref name=":0" /> | |||
A reduced or negative plantar grasp reflex during early infancy can be a sensitive indicator of later development of spasticity.<ref name=":0" /> | |||
Reappearance in adults- More recent studies have implicated lesions of the medial frontal cortex anterior to the primary motor cortex, i.e., the supplementary motor area and cingulate motor cortex, as the etiology of the palmer grasp reflex.<ref name=":4" /><ref>Hashimoto R, Tanaka Y. Contribution of the supplementary motor area and anterior cingulate gyrus to pathological grasping phenomena. Eur Neurol 1998;40:151-8</ref><ref>Goldberger ME. Restitution of function in the CNS: The pathologic grasp in Macaca mulatta. Exp Brain Res 1972;15:79-96</ref><ref>Smith AM, Bourbonnais D, Blanchette G. Interaction between forced grasping and a learned precision grip after ablation of the supplementary motor area. Brain Res 1981;222:395-400</ref> | |||
== Duration == | == Duration == | ||
The plantar grasp reflex can be elicited in all normal infants from 25 weeks of postconceptional age until the end of 6 months of corrected age according to the expected birth date.<ref name=":0" /> | |||
{{#ev:youtube|Vy18c5oGLSk}}<ref>Nicole Edmonds. Available from:https://www.youtube.com/watch?v=Vy18c5oGLSk </ref> | {{#ev:youtube|Vy18c5oGLSk}}<ref>Nicole Edmonds. Available from:https://www.youtube.com/watch?v=Vy18c5oGLSk </ref> | ||
Revision as of 14:55, 13 April 2022
Introduction[edit | edit source]
[1]Introduction[edit | edit source]
This reflex in human infants can be regarded as a rudiment of responses that were once essential for ape infants in arboreal life. The spinal center for this reflex is probably located at the L5-S2 levels, which, however, are controlled by higher brain structures. Nonprimary motor areas may exert regulatory control of the spinal reflex mechanism through interneurons. In infants, this reflex can be elicited as the result of insufficient control of the spinal mechanism by the immature brain. In adults, lesions in nonprimary motor areas may cause a release of inhibitory control by spinal interneurons, leading to a reappearance of the reflex.[1]
Position[edit | edit source]
Infant lying on a flat surface in the supine position while awake, head and arms at the neutral position. [2][3][4][5][1]
Care should be taken to keep the subject’s head facing the midline, to avoid the influence of the asymmetric tonic neck reflex.[1]
Stimulus[edit | edit source]
The plantar reflex is elicited:-
- By pressing a thumb against the sole of the foot just behind the toes.[1][2][3][4][5] OR
- By stroking gently the plantar surface medially with a blunt object such as the handle of a reflex hammer.[6]
Response[edit | edit source]
Normal Response[edit | edit source]
In Infants-The lateral surfaces of the foot bend as if to make a cup out of the plantar surface.[6] It consists of the flexion and adduction of all toes as if the toes were firmly grasping the stimulating object[7]; there is hollowing of the sole with some wrinkling of the skin. If the toes also flex, this is called the tonic foot response.[6] It is tonic in character, because the posture is often maintained for 15 or 30 seconds, or longer during early infancy[7]
In adults- no response - as it diminishes in later life.
Abnormal Response[edit | edit source]
In Infants- No response means there is underlying pathology.
In adults- If flexion or adduction of toes occurs it means there is underlying pathology.
Clinical significance[edit | edit source]
The plantar grasp reflex in infants is of high clinical significance. A negative or diminished reflex during early infancy is often a sensitive indicator of spasticity. Infants with athetoid type cerebral palsy exhibit extremely strong retention of the reflex, and infants with mental retardation also exhibit a tendency toward prolonged retention of the reflex.[1]
A reduced or negative plantar grasp reflex during early infancy can be a sensitive indicator of later development of spasticity.[1]
Reappearance in adults- More recent studies have implicated lesions of the medial frontal cortex anterior to the primary motor cortex, i.e., the supplementary motor area and cingulate motor cortex, as the etiology of the palmer grasp reflex.[5][8][9][10]
Duration[edit | edit source]
The plantar grasp reflex can be elicited in all normal infants from 25 weeks of postconceptional age until the end of 6 months of corrected age according to the expected birth date.[1]
Reference[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Futagi Y, Suzuki Y. Neural mechanism and clinical significance of the plantar grasp reflex in infants. Pediatric neurology. 2010 Aug 1;43(2):81-6.
- ↑ 2.0 2.1 Futagi Y, Suzuki Y, Goto M. Clinical significance of plantar grasp response in infants. Pediatric Neurology. 1999 Feb 1;20(2):111-5.
- ↑ 3.0 3.1 Prechtl H, Beinthema D. Reflexes and responses: The neurological examination of the full-term newborn infant. Clin Dev Med. 1977;63:40-2.
- ↑ 4.0 4.1 Touwen B. Reactions and responses: neurological development in infancy. Clinics in Developmental Medicine. 1976;58:83-98.
- ↑ 5.0 5.1 5.2 Schott JM, Rossor MN. The grasp and other primitive reflexes. Journal of Neurology, Neurosurgery & Psychiatry. 2003 May 1;74(5):558-60.
- ↑ 6.0 6.1 6.2 Walker HK. The suck, snout, palmomental, and grasp reflexes. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. 1990.
- ↑ 7.0 7.1 BRAIN WR, CURRAN RD. The grasp-reflex of the foot. Brain. 1932 Sep 1;55(3):347-56.
- ↑ Hashimoto R, Tanaka Y. Contribution of the supplementary motor area and anterior cingulate gyrus to pathological grasping phenomena. Eur Neurol 1998;40:151-8
- ↑ Goldberger ME. Restitution of function in the CNS: The pathologic grasp in Macaca mulatta. Exp Brain Res 1972;15:79-96
- ↑ Smith AM, Bourbonnais D, Blanchette G. Interaction between forced grasping and a learned precision grip after ablation of the supplementary motor area. Brain Res 1981;222:395-400
- ↑ Nicole Edmonds. Available from:https://www.youtube.com/watch?v=Vy18c5oGLSk