STarT Back Approach: Difference between revisions
(Created page with "== Introduction == The STarT Back approach uses a simple tool to match patients to treatment packages appropriate for them. This has been shown to: #Significantly decreas...") |
No edit summary |
||
| Line 15: | Line 15: | ||
There are now several different versions of the Keele STarT Back screening tool: | There are now several different versions of the Keele STarT Back screening tool: | ||
=== 9-item tool: for all clinicians including GPs === | === 9-item tool: for all clinicians including GPs === | ||
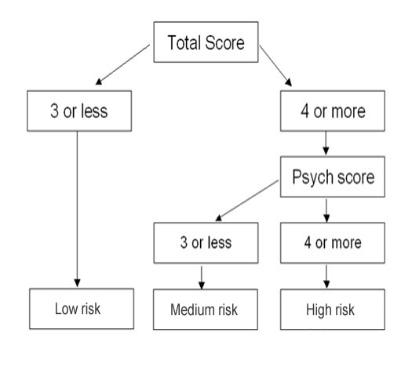
The [http://www.keele.ac.uk/media/keeleuniversity/group/startback/Keele_STarT_Back9_item-7.pdf SBST 9 item tool] has 9 questions about predictors for persistent disabling back pain. They include radiating leg pain, pain elsewhere, disability (2 items), fear, anxiety, pessimistic patient expectations, and low mood and how much the patient is bothered by their pain. All 9-items use a response format of ‘agree' or ‘disagree', with exception to the bothersomeness item, which uses a Likert scale. The Keele SBST produces two scores: overall and distress (psych) subscale. These are used to stratify patients into low, medium and high risk groups which have their respective matched treatment packages. | |||
[[Image: | [[Image:STarT Back Calculator.jpg|center]] | ||
=== Clinical measurement tool: monitor change === | |||
The 9-item [http://www.keele.ac.uk/media/keeleuniversity/group/startback/Keele_STarT_Back_Clinical-3.pdf SBST Clinical Measurement Tool] is designed to help clinicians objectively measure the severity of the domains screened by the 9-item tool. When repeated measures are used this enables an objective marker of change over time to be made for individual items.<br>Cut-offs have been established for each item - to enable those using this tool to subgroup patients in the same way as the 9-item screening tool. The cut-off points that equate to an agree/positive score on the clinical measurement tool for subgrouping are: | |||
*Leg pain - 'moderately' or more | |||
*Shoulder/neck - slightly or more | |||
*Dressing - 5 or more | |||
*Walking - 5 or more | |||
*Fear - 7 or more | |||
*Worry - 3 or more | |||
*Catastrophising - 6 or more | |||
*Mood - 7 or more | |||
*Bothersomeness - 'very' or more | |||
Its very easy to produce an acetate using these cut-offs that you place over the questionnaire to quickly enable you to score the clinical measurement tool for subgrouping purposes. | |||
== Matched Treatments == | |||
The STarT Back approach uses the STarT Back tool to stratify patients with back pain into low, medium and high risk groups for ongoing disability. For each group there is a different treatment package matched to their level of risk. | |||
=== Low Risk === | |||
The patients in the low risk category are very likely to improve. The aims of this package are to support and enable self-management. The key factors are to address patient concerns and to provide information. | |||
*One-off consultation with clinician (doctor, physiotherapist or nurse) sufficient for most patients | |||
*Assessment to include medical issues but also patient worries, concerns and social impact | |||
*Brief physical assessment as appropriate. Examination helps with patient confidence | |||
*Medication review and advice | |||
*Address specific patient issues from the assessment | |||
*Seek to encourage activity and self-management | |||
*Avoid unhelpful labels and medicalisation | |||
*Provide oral and written information | |||
*Explain outlook is good but can re-consult if necessary | |||
=== Medium Risk === | |||
This builds on the assessment from the low risk package. The main aims are to restore function (including work), minimise disability even if pain is unchanged and to support appropriate self-management. | |||
*Similar to low risk, elicit concerns and adequate physical examination | |||
*Tailored treatment according to physical findings and specific needs / worries of the individual patient | |||
*Course of physiotherapy, which for some patients may only be brief | |||
*Specific physiotherapy interventions when clear specific findings from physical assessment (i.e. manual therapy, specific exercises). | |||
*General functional activities when no strong relationship between physical findings and back pain complaint | |||
*Treatment objectives should be specific and have an end time point. All specific treatment effects should ‘translate’ into functional improvements and reduced disability | |||
*Some patients will need onward referral to specialist services (i.e. secondary care spinal services, ortho, pain clinic) | |||
=== High Risk === | |||
This again builds on the low and medium risk packages. The aims are to reduce pain, reduce disability and improve psychological functioning. The physiotherapists delivering the high risk package have additional training, mentorship and ongoing professional support to enable them to elicit and address more complex issues in patients who often have additional psycho-social barriers to recovery. It is important to emphasis that the physiotherapists also provided physical treatments to these patients as required. | |||
*6 individual (45-60 min) physiotherapy appointments over 3 months using a combined physical & cognitive-behavioural approach | |||
*Enable patients to manage on-going and/or future episodes of low back pain | |||
*Specific focus on cognitive, emotional and behavioural responses to pain and their impact on function | |||
*Identification of potential obstacles to rehabilitation (e.g. Yellow & Blue Flags) | |||
*Identification of possible targets for intervention<br><br> | |||
Revision as of 14:23, 24 October 2015
Introduction[edit | edit source]
The STarT Back approach uses a simple tool to match patients to treatment packages appropriate for them. This has been shown to:
- Significantly decrease disability from back pain
- Reduce time off work
- Save money by making better use of health resources
Taking the concept further it has been shown in the IMPaCT study that this approach can be successfully embedded into normal primary care[1]. The STarT Back approach continues to be adopted across the UK and Internationally.
The STarT Back Screening Tool[edit | edit source]
The Keele STarT Back Screening Tool (SBST) is a simple prognostic questionnaire that helps clinicians identify modifiable risk factors (biomedical, psychological and social) for back pain disability. The resulting score stratifies patients into low, medium or high risk categories. For each category there is a matched treatment package.
There are now several different versions of the Keele STarT Back screening tool:
9-item tool: for all clinicians including GPs[edit | edit source]
The SBST 9 item tool has 9 questions about predictors for persistent disabling back pain. They include radiating leg pain, pain elsewhere, disability (2 items), fear, anxiety, pessimistic patient expectations, and low mood and how much the patient is bothered by their pain. All 9-items use a response format of ‘agree' or ‘disagree', with exception to the bothersomeness item, which uses a Likert scale. The Keele SBST produces two scores: overall and distress (psych) subscale. These are used to stratify patients into low, medium and high risk groups which have their respective matched treatment packages.
Clinical measurement tool: monitor change[edit | edit source]
The 9-item SBST Clinical Measurement Tool is designed to help clinicians objectively measure the severity of the domains screened by the 9-item tool. When repeated measures are used this enables an objective marker of change over time to be made for individual items.
Cut-offs have been established for each item - to enable those using this tool to subgroup patients in the same way as the 9-item screening tool. The cut-off points that equate to an agree/positive score on the clinical measurement tool for subgrouping are:
- Leg pain - 'moderately' or more
- Shoulder/neck - slightly or more
- Dressing - 5 or more
- Walking - 5 or more
- Fear - 7 or more
- Worry - 3 or more
- Catastrophising - 6 or more
- Mood - 7 or more
- Bothersomeness - 'very' or more
Its very easy to produce an acetate using these cut-offs that you place over the questionnaire to quickly enable you to score the clinical measurement tool for subgrouping purposes.
Matched Treatments[edit | edit source]
The STarT Back approach uses the STarT Back tool to stratify patients with back pain into low, medium and high risk groups for ongoing disability. For each group there is a different treatment package matched to their level of risk.
Low Risk[edit | edit source]
The patients in the low risk category are very likely to improve. The aims of this package are to support and enable self-management. The key factors are to address patient concerns and to provide information.
- One-off consultation with clinician (doctor, physiotherapist or nurse) sufficient for most patients
- Assessment to include medical issues but also patient worries, concerns and social impact
- Brief physical assessment as appropriate. Examination helps with patient confidence
- Medication review and advice
- Address specific patient issues from the assessment
- Seek to encourage activity and self-management
- Avoid unhelpful labels and medicalisation
- Provide oral and written information
- Explain outlook is good but can re-consult if necessary
Medium Risk[edit | edit source]
This builds on the assessment from the low risk package. The main aims are to restore function (including work), minimise disability even if pain is unchanged and to support appropriate self-management.
- Similar to low risk, elicit concerns and adequate physical examination
- Tailored treatment according to physical findings and specific needs / worries of the individual patient
- Course of physiotherapy, which for some patients may only be brief
- Specific physiotherapy interventions when clear specific findings from physical assessment (i.e. manual therapy, specific exercises).
- General functional activities when no strong relationship between physical findings and back pain complaint
- Treatment objectives should be specific and have an end time point. All specific treatment effects should ‘translate’ into functional improvements and reduced disability
- Some patients will need onward referral to specialist services (i.e. secondary care spinal services, ortho, pain clinic)
High Risk[edit | edit source]
This again builds on the low and medium risk packages. The aims are to reduce pain, reduce disability and improve psychological functioning. The physiotherapists delivering the high risk package have additional training, mentorship and ongoing professional support to enable them to elicit and address more complex issues in patients who often have additional psycho-social barriers to recovery. It is important to emphasis that the physiotherapists also provided physical treatments to these patients as required.
- 6 individual (45-60 min) physiotherapy appointments over 3 months using a combined physical & cognitive-behavioural approach
- Enable patients to manage on-going and/or future episodes of low back pain
- Specific focus on cognitive, emotional and behavioural responses to pain and their impact on function
- Identification of potential obstacles to rehabilitation (e.g. Yellow & Blue Flags)
- Identification of possible targets for intervention
- ↑ Nadine E. Foster, Ricky Mullis, Jonathan C. Hill, Martyn Lewis, David G. T. Whitehurst, Carol Doyle, Kika Konstantinou, Chris Main, Simon Somerville, Gail Sowden, Simon Wathall, Julie Young, Elaine M. Hay. Effect of Stratified Care for Low Back Pain in Family Practice (IMPaCT Back): A Prospective Population-Based Sequential Comparison. Ann Fam Med. 2014 March; 12(2): 102–111. doi: 10.1370/afm.1625