Sinuvertebral Nerve: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
<div class = "noeditbox"> | |||
== Description == | == Description == | ||
'''The sinuvertebral nerve''' (or '''Luschka nerve''') is a recurrent nerve that originates from the [https://en.wikipedia.org/wiki/Ventral_ramus_of_spinal_nerve ventral ramus], re-entering the spinal canal via the [https://en.wikipedia.org/wiki/Intervertebral_foramen intervertebral foramina] to innervate the [[Intervertebral disc|anulus fibrosus of the intervertebral disc]], [[Facet Joints|the facet joints]], the ligaments and periosteum of the spinal canal. Its complex anatomy and relationship to discogenic pain have warranted great interest among clinical anatomists owing to its sympathetic contribution to the lumbar spine. Knowledge of the nerve has been used to design a variety of diagnostic and treatment procedures for chronic [[Lumbar Discogenic Pain|discogenic pain]] [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6624329/#B20]. | '''The sinuvertebral nerve''' (or '''Luschka nerve''') is a recurrent nerve that originates from the [https://en.wikipedia.org/wiki/Ventral_ramus_of_spinal_nerve ventral ramus], re-entering the spinal canal via the [https://en.wikipedia.org/wiki/Intervertebral_foramen intervertebral foramina] to innervate the [[Intervertebral disc|anulus fibrosus of the intervertebral disc]], [[Facet Joints|the facet joints]], the ligaments and periosteum of the spinal canal. Its complex anatomy and relationship to discogenic pain have warranted great interest among clinical anatomists owing to its sympathetic contribution to the lumbar spine. Knowledge of the nerve has been used to design a variety of diagnostic and treatment procedures for chronic [[Lumbar Discogenic Pain|discogenic pain]] <ref name=":0">Shayota B, Wong TL, Fru D, et al. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6624329/#B20 A comprehensive review of the sinuvertebral nerve with clinical applications]. ''Anat Cell Biol''. 2019;52(2):128-133. doi:10.5115/acb.2019.52.2.128</ref>. | ||
=== Root === | |||
=== Branches === | |||
== Function == | |||
=== Motor === | |||
=== Sensory === | |||
== Clinical relevance == | |||
== Assessment == | |||
== Treatment == | |||
== References == | |||
== Anatomy == | == Anatomy == | ||
| Line 6: | Line 25: | ||
The sinuvertebral nerve arises bilaterally from the ventral ramus of each [https://en.wikipedia.org/wiki/Spinal_nerve spinal nerve] just distal to the dorsal root ganglia, supplying both proprioceptive and nociceptive fibers. Upon separation from the ventral ramus, it travels medially for 2–3 mm to be joined by a branch from the grey ramus communicans. This branch contributes sympathetic neurons to the sinuvertebral nerve. The nerve then takes a recurrent course and re-enters the spinal canal through the intervertebral foramen, more specifically through the osteofibrous foramen formed by the deep anterior intraforaminal ligament, just caudal to the pedicle. Although it passes through the intervertebral foramen, it is unlikely to be compressed during disc herniation because it is located alongside the pedicle, cranial to the corresponding disc. At the point of entrance, the composite nerve is about 0.5–1.0 mm in diameter. | The sinuvertebral nerve arises bilaterally from the ventral ramus of each [https://en.wikipedia.org/wiki/Spinal_nerve spinal nerve] just distal to the dorsal root ganglia, supplying both proprioceptive and nociceptive fibers. Upon separation from the ventral ramus, it travels medially for 2–3 mm to be joined by a branch from the grey ramus communicans. This branch contributes sympathetic neurons to the sinuvertebral nerve. The nerve then takes a recurrent course and re-enters the spinal canal through the intervertebral foramen, more specifically through the osteofibrous foramen formed by the deep anterior intraforaminal ligament, just caudal to the pedicle. Although it passes through the intervertebral foramen, it is unlikely to be compressed during disc herniation because it is located alongside the pedicle, cranial to the corresponding disc. At the point of entrance, the composite nerve is about 0.5–1.0 mm in diameter. | ||
The sinuvertebral nerve is formed by the union of a somatic root from the ventral ramus and an autonomic root provided by the grey ramus [[:File:Sinuvertebral nerve.jpg|(Fig. 1)]]. Among the cervical levels, the grey rami give rise to the autonomic roots to form the vertebral nerve, whereas the thoracic and lumbar levels receive somatic roots from the ventral rami and autonomic contributions from grey rami communicans of the sympathetic trunk. This mixture of somatosensory and sympathetic fibers has traditionally been portrayed as a single nerve, but more accurately it comprises a series of fine filaments of which one to four larger trunks can be evident [https://onlinelibrary.wiley.com/doi/abs/10.1002/aja.1001880307]. | The sinuvertebral nerve is formed by the union of a somatic root from the ventral ramus and an autonomic root provided by the grey ramus [[:File:Sinuvertebral nerve.jpg|(Fig. 1)]]. Among the cervical levels, the grey rami give rise to the autonomic roots to form the vertebral nerve, whereas the thoracic and lumbar levels receive somatic roots from the ventral rami and autonomic contributions from grey rami communicans of the sympathetic trunk. This mixture of somatosensory and sympathetic fibers has traditionally been portrayed as a single nerve, but more accurately it comprises a series of fine filaments of which one to four larger trunks can be evident <ref>Groen GJ, Baljet B, Drukker J. [https://onlinelibrary.wiley.com/doi/abs/10.1002/aja.1001880307 Nerves and nerve plexuses of the human vertebral column]. Am J Anat. 1990;188:282–296.</ref>. | ||
== History == | == History == | ||
First described by the German anatomist Hubert von Luschka in 1850, the sinuvertebral nerve has since acquired many other names including the recurrent nerve of Luschka, recurrent meningeal nerve, ramus meningeus, and meningeal branch of the spinal nerve. Luschka described the sinuvertebral nerve's derivation from the spinal nerve and its connection to the sympathetic nervous system. Furthermore, he indicated that there could be intersegmental anastomoses among its branches, but was unable to demonstrate them. His account was maintained for nearly a century until illustrations by other scientists showed that the nerve's distribution extended as far as the posterior anulus fibrosus [https://online.boneandjoint.org.uk/doi/full/10.1302/0301-620X.89B9.18939]. | First described by the German anatomist Hubert von Luschka in 1850, the sinuvertebral nerve has since acquired many other names including the recurrent nerve of Luschka, recurrent meningeal nerve, ramus meningeus, and meningeal branch of the spinal nerve. Luschka described the sinuvertebral nerve's derivation from the spinal nerve and its connection to the sympathetic nervous system. Furthermore, he indicated that there could be intersegmental anastomoses among its branches, but was unable to demonstrate them. His account was maintained for nearly a century until illustrations by other scientists showed that the nerve's distribution extended as far as the posterior anulus fibrosus <ref>Edgar MA. [https://online.boneandjoint.org.uk/doi/full/10.1302/0301-620X.89B9.18939 The nerve supply of the lumbar intervertebral disc.] J Bone Joint Surg Br. 2007;89:1135–1139.</ref>. | ||
== Role in discogenic pain == | == Role in discogenic pain == | ||
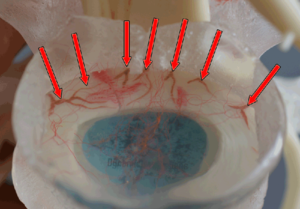
[[File:Sinuvertebral nerve 2.png|thumb|The synvertebral nerve (red arrows) may grow deep into the disc]] | [[File:Sinuvertebral nerve 2.png|thumb|The synvertebral nerve (red arrows) may grow deep into the disc]] | ||
Associated with the discogenic type low back pain (pain from an injured vertebral disc), accounts for approximately 26%–39% of patients with [[Low Back Pain|low back pain]] [https://www.painphysicianjournal.com/linkout?issn=1533-3159&vol=4&page=308]. This pain travels through the rami communicantes down to L2 where it joins the sympathetic ganglion and then travels to the skin at lower levels. | Associated with the discogenic type low back pain (pain from an injured vertebral disc), accounts for approximately 26%–39% of patients with [[Low Back Pain|low back pain]] <ref>Manchikanti L, Singh V, Pampati V, Damron KS, Barnhill RC, Beyer C, Cash KA. [https://www.painphysicianjournal.com/linkout?issn=1533-3159&vol=4&page=308 Evaluation of the relative contributions of various structures in chronic low back pain.] Pain Physician. 2001;4:308–316.</ref>. This pain travels through the rami communicantes down to L2 where it joins the sympathetic ganglion and then travels to the skin at lower levels. | ||
Although the sinuvertebral nerve fibers are said to terminate in the outer anulus, it is now widely accepted that this end point is not permanent. Studies of healthy patients normally show neural penetration of the anulus at about 3 mm [https://www.tandfonline.com/doi/abs/10.3109/17453679408994620], corresponding to the three outer lamellae. However, degenerative discs have shown penetration of nerve fibers as far as the inner one third in one study [https://journals.lww.com/spinejournal/Abstract/1991/06000/Immunohistochemical_Demonstration_of_Sensory_Nerve.10.aspx], and into the nucleus pulposus in another <ref>Peng B, Wu W, Hou S, Li P, Zhang C, Yang Y. The pathogenesis of discogenic low back pain. ''J Bone Joint Surg Br''. 2005;87(1):62-67.</ref>. | Although the sinuvertebral nerve fibers are said to terminate in the outer anulus, it is now widely accepted that this end point is not permanent. Studies of healthy patients normally show neural penetration of the anulus at about 3 mm <ref>Ashton IK, Walsh DA, Polak JM, Eisenstein SM. [https://www.tandfonline.com/doi/abs/10.3109/17453679408994620 Substance P in intervertebral discs: binding sites on vascular endothelium of the human annulus fibrosus]. Acta Orthop Scand. 1994;65:635–639.</ref>, corresponding to the three outer lamellae. However, degenerative discs have shown penetration of nerve fibers as far as the inner one third in one study <ref>McCARTHY, P. W., PhD; CARRUTHERS, B., MSc; MARTIN, D.; PETTS, P. FILMS, DC [https://journals.lww.com/spinejournal/Abstract/1991/06000/Immunohistochemical_Demonstration_of_Sensory_Nerve.10.aspx Immunohistochemical Demonstration of Sensory Nerve Fibers and Endings in Lumbar Intervertebral Discs of the Rat], Spine: June 1991 - Volume 16 - Issue 6 - p 653-655</ref>, and into the nucleus pulposus in another <ref>Peng B, Wu W, Hou S, Li P, Zhang C, Yang Y. [https://pubmed.ncbi.nlm.nih.gov/15686239/ The pathogenesis of discogenic low back pain]. ''J Bone Joint Surg Br''. 2005;87(1):62-67.</ref>. | ||
== Diagnostics == | == Diagnostics == | ||
'''Provocative discography''' is the gold standard for back pain related to intervertebral disc pathology. The procedure involves the injection of contrast medium into the disc with concomitant assessment of the patient's pain response. If a particular disc is painful, then stressing it should reproduce the patient's usual pain. If the disc is not the source of a patient's pain, then stressing it should either not be painful or produce pain to which the patient is not accustomed. Thus, patients who suffer from severe back or neck pain of unknown etiology are often recommended for provocation discography. If the intervertebral disc is implicated, the excessive pain felt during injection is transmitted via the sinuvertebral nerve. Discography has proved significantly more effective for diagnosing degenerative disc disease than magnetic resonance imaging | '''Provocative discography''' is the gold standard for back pain related to intervertebral disc pathology. The procedure involves the injection of contrast medium into the disc with concomitant assessment of the patient's pain response. If a particular disc is painful, then stressing it should reproduce the patient's usual pain. If the disc is not the source of a patient's pain, then stressing it should either not be painful or produce pain to which the patient is not accustomed. Thus, patients who suffer from severe back or neck pain of unknown etiology are often recommended for provocation discography. If the intervertebral disc is implicated, the excessive pain felt during injection is transmitted via the sinuvertebral nerve. Discography has proved significantly more effective for diagnosing degenerative disc disease than magnetic resonance imaging <ref name=":0" /><ref>Choi SH, Adsul N, Kim HS, Jang JS, Jang IT, Oh SH. [https://www.sciencedirect.com/science/article/abs/pii/S1878875017320831?via%3Dihub Magnetic resonance imaging undetectable epiduroscopic hotspot in chronic diskogenic back pain: does sinuvertebral neuropathy actually exist?] World Neurosurg. 2018;110:354–358</ref>. | ||
== See also == | == See also == | ||
| Line 27: | Line 46: | ||
[[Category:Anatomy]] | [[Category:Anatomy]] | ||
[[Category:Nerves]] | [[Category:Nerves]] | ||
<references /> | |||
Revision as of 19:02, 18 September 2020
Description[edit | edit source]
The sinuvertebral nerve (or Luschka nerve) is a recurrent nerve that originates from the ventral ramus, re-entering the spinal canal via the intervertebral foramina to innervate the anulus fibrosus of the intervertebral disc, the facet joints, the ligaments and periosteum of the spinal canal. Its complex anatomy and relationship to discogenic pain have warranted great interest among clinical anatomists owing to its sympathetic contribution to the lumbar spine. Knowledge of the nerve has been used to design a variety of diagnostic and treatment procedures for chronic discogenic pain [1].
Root[edit | edit source]
Branches[edit | edit source]
Function[edit | edit source]
Motor[edit | edit source]
Sensory[edit | edit source]
Clinical relevance[edit | edit source]
Assessment[edit | edit source]
Treatment[edit | edit source]
References[edit | edit source]
Anatomy[edit | edit source]
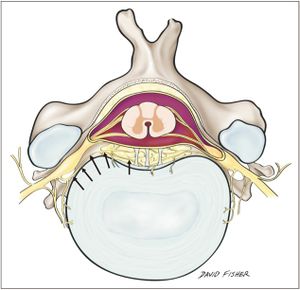
The sinuvertebral nerve arises bilaterally from the ventral ramus of each spinal nerve just distal to the dorsal root ganglia, supplying both proprioceptive and nociceptive fibers. Upon separation from the ventral ramus, it travels medially for 2–3 mm to be joined by a branch from the grey ramus communicans. This branch contributes sympathetic neurons to the sinuvertebral nerve. The nerve then takes a recurrent course and re-enters the spinal canal through the intervertebral foramen, more specifically through the osteofibrous foramen formed by the deep anterior intraforaminal ligament, just caudal to the pedicle. Although it passes through the intervertebral foramen, it is unlikely to be compressed during disc herniation because it is located alongside the pedicle, cranial to the corresponding disc. At the point of entrance, the composite nerve is about 0.5–1.0 mm in diameter.
The sinuvertebral nerve is formed by the union of a somatic root from the ventral ramus and an autonomic root provided by the grey ramus (Fig. 1). Among the cervical levels, the grey rami give rise to the autonomic roots to form the vertebral nerve, whereas the thoracic and lumbar levels receive somatic roots from the ventral rami and autonomic contributions from grey rami communicans of the sympathetic trunk. This mixture of somatosensory and sympathetic fibers has traditionally been portrayed as a single nerve, but more accurately it comprises a series of fine filaments of which one to four larger trunks can be evident [2].
History[edit | edit source]
First described by the German anatomist Hubert von Luschka in 1850, the sinuvertebral nerve has since acquired many other names including the recurrent nerve of Luschka, recurrent meningeal nerve, ramus meningeus, and meningeal branch of the spinal nerve. Luschka described the sinuvertebral nerve's derivation from the spinal nerve and its connection to the sympathetic nervous system. Furthermore, he indicated that there could be intersegmental anastomoses among its branches, but was unable to demonstrate them. His account was maintained for nearly a century until illustrations by other scientists showed that the nerve's distribution extended as far as the posterior anulus fibrosus [3].
Role in discogenic pain[edit | edit source]
Associated with the discogenic type low back pain (pain from an injured vertebral disc), accounts for approximately 26%–39% of patients with low back pain [4]. This pain travels through the rami communicantes down to L2 where it joins the sympathetic ganglion and then travels to the skin at lower levels.
Although the sinuvertebral nerve fibers are said to terminate in the outer anulus, it is now widely accepted that this end point is not permanent. Studies of healthy patients normally show neural penetration of the anulus at about 3 mm [5], corresponding to the three outer lamellae. However, degenerative discs have shown penetration of nerve fibers as far as the inner one third in one study [6], and into the nucleus pulposus in another [7].
Diagnostics[edit | edit source]
Provocative discography is the gold standard for back pain related to intervertebral disc pathology. The procedure involves the injection of contrast medium into the disc with concomitant assessment of the patient's pain response. If a particular disc is painful, then stressing it should reproduce the patient's usual pain. If the disc is not the source of a patient's pain, then stressing it should either not be painful or produce pain to which the patient is not accustomed. Thus, patients who suffer from severe back or neck pain of unknown etiology are often recommended for provocation discography. If the intervertebral disc is implicated, the excessive pain felt during injection is transmitted via the sinuvertebral nerve. Discography has proved significantly more effective for diagnosing degenerative disc disease than magnetic resonance imaging [1][8].
See also[edit | edit source]
- ↑ 1.0 1.1 Shayota B, Wong TL, Fru D, et al. A comprehensive review of the sinuvertebral nerve with clinical applications. Anat Cell Biol. 2019;52(2):128-133. doi:10.5115/acb.2019.52.2.128
- ↑ Groen GJ, Baljet B, Drukker J. Nerves and nerve plexuses of the human vertebral column. Am J Anat. 1990;188:282–296.
- ↑ Edgar MA. The nerve supply of the lumbar intervertebral disc. J Bone Joint Surg Br. 2007;89:1135–1139.
- ↑ Manchikanti L, Singh V, Pampati V, Damron KS, Barnhill RC, Beyer C, Cash KA. Evaluation of the relative contributions of various structures in chronic low back pain. Pain Physician. 2001;4:308–316.
- ↑ Ashton IK, Walsh DA, Polak JM, Eisenstein SM. Substance P in intervertebral discs: binding sites on vascular endothelium of the human annulus fibrosus. Acta Orthop Scand. 1994;65:635–639.
- ↑ McCARTHY, P. W., PhD; CARRUTHERS, B., MSc; MARTIN, D.; PETTS, P. FILMS, DC Immunohistochemical Demonstration of Sensory Nerve Fibers and Endings in Lumbar Intervertebral Discs of the Rat, Spine: June 1991 - Volume 16 - Issue 6 - p 653-655
- ↑ Peng B, Wu W, Hou S, Li P, Zhang C, Yang Y. The pathogenesis of discogenic low back pain. J Bone Joint Surg Br. 2005;87(1):62-67.
- ↑ Choi SH, Adsul N, Kim HS, Jang JS, Jang IT, Oh SH. Magnetic resonance imaging undetectable epiduroscopic hotspot in chronic diskogenic back pain: does sinuvertebral neuropathy actually exist? World Neurosurg. 2018;110:354–358