Specific Low Back Pain: Difference between revisions
Allan D'Hose (talk | contribs) No edit summary |
Allan D'Hose (talk | contribs) No edit summary |
||
| Line 426: | Line 426: | ||
<br> | <br> | ||
'''VAS: Visual Analog Scale '''([http://www.physio-pedia.com/Visual_Analogue_Scale www.physio-pedia.com/Visual_Analogue_Scale]) | '''VAS: Visual Analog Scale '''([http://www.physio-pedia.com/Visual_Analogue_Scale www.physio-pedia.com/Visual_Analogue_Scale]) | ||
= Examination = | |||
Revision as of 14:34, 4 February 2017
Search Strategy[edit | edit source]
We used databases such as Pubmed and ResearchGate, VUBBIBLIO, GoogleScholar, to find scientific articles. We also used a few books to achieve some information as well as related physiopedia pages related to our topic.
Our keywords consisted of “specific low back pain” wether or not combined with “description”, “symptoms”, “diagnosis”, “treatment”, “measurement”, “examination”, “physical therapy” and so on. We also used specific diagnosis like “scheuermanns disease, scoliosis and other to look for very specific information about diagnosis whom are included within the broad term “specific low back pain”.
We only used articles of which the full text was available.
Definition/Description
[edit | edit source]
Low back pain is a considerable health problem in all developed countries and is most commonly treated in primary healthcare settings. It is usually defined as pain, muscle tension, or stiffness localized below the costal margin and above the inferior gluteal folds, with or without leg pain (sciatica). The most important symptoms of low back pain are pain and disability..
About 90% of all patients with low back pain will have non-specific low back pain, which, in essence, is a diagnosis based on exclusion of specific pathology [1]. Those specific pathologies can be defined as:
- Radicular syndrom (www.physio-pedia.com/Lumbar_Radiculopathy)
- Discus problems (protrusion, prolapse ...) (www.physio-pedia.com/Disc_Herniation)
- Spinal canal stenose (www.physio-pedia.com/Lumbar_spinal_stenosis)
- Spondylolisthesis (www.physio-pedia.com/Spondylolisthesis)
- Ankylosing spondylitis (www.physio-pedia.com/Ankylosing_Spondylitis)
- Osteoporosis/osteoartritis (www.physio-pedia.com/Osteoporosis)
- Traumatic fractures (www.physio-pedia.com/Lumbar_Spine_Fracture)
- Metastases (www.physio-pedia.com/Skeletal_Metastases)
- Cauda equina (www.physio-pedia.com/Cauda_Equina_Syndrome)
- Scheuermans Disease (www.physio-pedia.com/Scheuermanns_Disease)
- Scoliosis (www.physio-pedia.com/Scoliosis)
Clinically Relevant Anatomy[edit | edit source]
The human spine is a self-supporting construction of skeleton, cartilage, ligaments and muscles. Erect, there are four sagittal curves, which are the result of man’s evolution from quadruped to biped. The four curves resulted: cervical lordosis, thoracic kyphosis, lumbar lordosis and sacrococcygeal kyphosis. This S form seems to be a compromise between the static and the dynamic qualities of the spine; theoretical considerations suggest that the S form is the shape an elastic bar adopts when it is subjected to axial compression.
Vertebral bodies
Each vertebral body is more or less a cylinder with a thin cortical shell, which surrounds cancellous bone. From L1 to L5, the posterior aspect changes from slightly concave to slightly convex, and the diameter of the cylinder increases gradually because of the increasing loads each body has to carry. At the upper and lower surfaces, two distinct areas can be seen: each is a peripheral ring of compact bone – surrounding and slightly above the level of the flat and rough central zone – which originates from the apophysis and fuses with the vertebral body at the age of about 16. The central zone – the bony endplate – shows many perforations, through which blood vessels can reach the disc. A layer of cartilage covers this central zone, which is limited by the peripheral ring. This is the cartilaginous endplate, forming the transition between the cortical bone and the rest of the intervertebral disc. A sagittal cut through the vertebral body shows the endplates to be slightly concave, which consequently gives the disc a convex form.
Pedicles
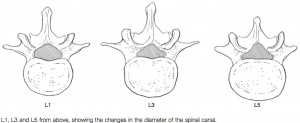
The two pedicles originate posteriorly and attach to the cranial half of the body. Together with the broad and flat lamina, they form the vertebral arch. From L1 to L5, the pedicles become shorter and broader, and are more lateral. This narrows the anteroposterior
diameter and widens the transverse diameter of the vertebral canal from above downwards. Together with the increasing convexity of the posterior aspect of the vertebral body, these changes in the position of the pedicles alter the shape of the normal bony spinal canal from an ellipse at L1 to a triangle at L3 and more or less a trefoil at L5 (Fig. 1).
Laminae
Each lamina is flat and broad, blending in centrally with the similarly configured spinal process, which projects directly backwards from the lamina. The two transverse processes project laterally and slightly dorsally from the pediculolaminar junction. The superior and inferior articular processes originate directly from the lamina.
The part of the lamina between the superior and inferior articular processes is called the ‘pars interlaminaris’. It runs obliquely from the lateral border of the lamina to its upper medial border. This portion of the lamina is subjected to considerable bending forces, as it lies at the junction between the vertically oriented lamina and the horizontally oriented pedicle. This ‘interlaminar part’ will therefore be susceptible to fatigue fractures or stress fractures (spondylolysis).
Intervertebral discs
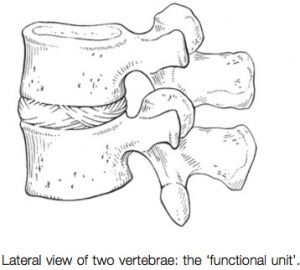
Two adjacent vertebral bodies are linked by an intervertebral disc. Together with the corresponding facet joints, they form the ‘functional unit of Junghans’n (Fig. 2).
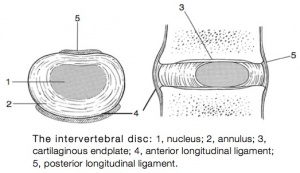
The disc consists of an annulus fibrosus, a nucleus pulposus and two cartilaginous endplates. The distinction between annulus and nucleus can only be made in youth, because the consistency of the disc becomes more uniform in the elderly. For this reason, nuclear disc protrusions are rare after the age of 70. From a clinical point of view, it is important to consider the disc as one integrated unit, the normal function of which depends largely on the integrity of all the elements. That means that damage to one component will create adverse reactions in the others.
Endplates
An upper and a lower cartilaginous endplate (each about 0.6– 1 mm thick) cover the superior and inferior aspects of the disc. They are plates of cartilage that bind the disc to their respective vertebral bodies. Each endplate covers almost the entire surface of the adjacent vertebral body; only a narrow rim of bone, called the ring apophysis, around the perimeter of the vertebral body is left uncovered by cartilage. That portion of the vertebral body to which the cartilaginous endplate is applied is referred to as the vertebral endplate. The endplate covers the nucleus pulposus in its entirety; peripherally it fails to cover the entire extent of the annulus fibrosus. The collagen fibrils of the inner lamellae of the annulus enter the endplate and merge with it, resulting in all aspects of the nucleus being enclosed by a fibrous capsule.
The endplate permits diffusion and provides the main source of nutrition for the disc. The hyaline endplate is also the last part of the disc to wear through during severe disc degeneration.
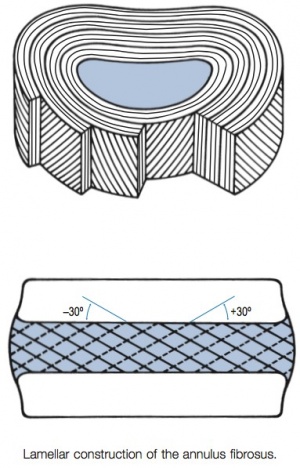
This is made up of 15–25 concentric fibrocartilaginous sheets or ‘lamellae’ (Fig. 3), each formed by parallel fibres, running obliquely at a 30° angle between the vertebral bodies. Because the fibers of two consecutive layers are oriented in opposite directions, they cross each other at an angle of approximately 120°. This arrangement of the annular fibers gives the normal disc great strength against shearing and rotational stresses, while angular movements remain perfectly possible. The outermost fibers are attached directly to bone, around the ring apophysis, and for that reason they are referred to as the ligamentous portion of the annulus fibrosis. The inner third merges with the cartilaginous endplate and is referred to as the capsular portion of the annulus fibrosis (Fig. 4).
Nucleus pulposus
This consists of a gelatinous substance, made of a meshwork of collagen fibrils suspended in a mucoprotein base, which contains mucopolysaccharides and water.
As the anterior part of the vertebral body grows faster than the posterior part, the nucleus comes to lie more posteriorly. Consequently, the anterior part of the annulus will have thicker and stronger fibres, which means that the annulus gives better protection against anterior than posterior displacements of the nucleus; this is disadvantageous with respect to the contiguous nerve roots and dura.
Functions of the disc
The primary function of the disc is to join the vertebrae and allow movement between them. The other functions are typical of the erect spine: a shock absorber; a load distributor; and a separator of the posterior facets to maintain the size of the intervertebral foramen.
The weak zone of the disc
Several anatomical, biochemical and biomechanical properties make the posterior aspect of the disc the most critical and vulnerable part of the whole intervertebral joint.
• The posterior annular fibers are sparser and thinner than the anterior.
• Because the area available for diffusion is smaller posteriorly than anteriorly, the posterior part of the nuclear–annular boundary receives less nutrition and again the posterior part of the disc is the most strained part.
• The posterior longitudinal ligament affords only weak reinforcement, whereas the anterior fibers are strengthened by the powerful anterior longitudinal ligament.
• Because of the special mechanical arrangements of the annular fibers, the tangential tensile strain on the posterior annular fibers is 4–5 times the applied external load.
All these elements explain the predominance of the posterior part of the disc in the development of weakening, radiating ruptures and posterior nuclear displacements. This is unfortunate, because most nociceptive tissues responsible for backache and sciatica (nerve roots and dura mater) emerge just beyond the posterior aspect of the disc.
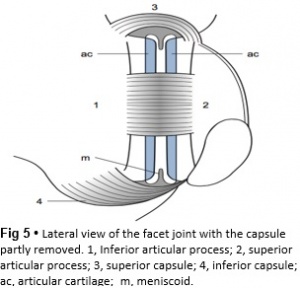
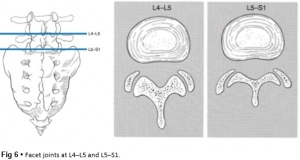
The joints between the lower and upper articular processes are called zygapophyseal joints, apophyseal joints or ‘facet’ joints. They are true synovial joints, comprised of cartilaginous articular surfaces, synovial fluid, synovial tissue and a joint capsule (Fig. 5).
The superior articular surface is slightly concave and faces medially and posteriorly. The convex inferior articular surface points laterally and slightly anteriorly. In general terms, there is a change from a relatively sagittal orientation at L1–L3, to a more coronal orientation at L5 and S1 (Fig. 6).
Unlike the disc, the facet joints normally do not bear weight and during normal loads they are not subjected to compression strain. In degenerative fragmentation of the disc, however, intervertebral height diminishes and the articular surfaces are subjected to abnormal loading, setting up spondylarthrosis. The main function of the facet joints is to guide lumbar movements and keep the vertebrae in line during flexion–extension and lateral flexion. Because of the more sagittal slope of the articular surfaces, very little rotation takes place at the four upper lumbar levels. More distally, at the lumbosacral level, the joint line has a more coronal plane, which makes rotational movements potentially possible, but these are limited by the iliolumbar ligaments. The total range of rotation in the lumbar spine is therefore very limited, although not completely zero. Fibers of the medial branch of the dorsal root innervate the facet joints. The same nerve supplies the inferior aspect of the capsule and the superior aspect of the joint below.
Ligaments
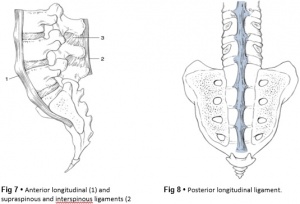
The broad, thick anterior longitudinal ligament (Fig. 7) originates from the anterior and basilar aspect of the occiput and ends at the upper and anterior part of the sacrum. It consists of fibers of different lengths: some extend over 4–5 vertebral bodies; the short fibers attach firmly to the fibers of the outermost annular layers and the periosteum of two adjacent vertebrae.
The posterior longitudinal ligament (Fig. 8) is smaller and thinner than its anterior counterpart: 1.4 cm wide (versus 2 cm in the anterior ligament) and 1.3 mm thick (versus 2 mm). The posterior longitudinal ligament is narrow at the level of the vertebral bodies, and gives lateral expansions to the annulus fibrosis at the level of the disc, which bestow on it a denticulated appearance.
Although the posterior ligament is rather narrow, it is important in preventing disc protrusion. Its resistance is the main factor in restricting posterior prolapse and accounts for the regular occurrence of spontaneous reduction in lumbago. This characteristic is also exploited in manipulative reduction, when a small central disc displacement is moved anteriorly when the ligament is tightened.
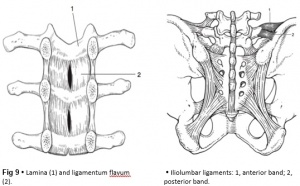
The ligamentum flavum (Fig. 9) connects two consecutive laminae and has a very elastic structure with an elastin content of more than 80%. The lateral extensions form the anterior capsule of the facet joints and run further laterally to connect the posterior and inferior borders of the pedicle above with the posterior and superior borders of the pedicle below. These lateral fibers form a portion of the foraminal ring and the lateral recess.
The interspinous ligament (Fig.7) lies deeply between two consecutive spinal processes. Unlike the longitudinal ligaments, it is not a continuous fibrous band but consists of loose tissue, with the fibers running obliquely from posterosuperior to anteroinferior. This particular direction may give the ligament a function over a larger range of intervertebral motion than if the fibers were vertical. The ligament is also bifid, which allows the fibers to buckle laterally to both sides when the spinous processes approach each other during extension.
The supraspinous ligament is broad, thick and cord-like. It joins the tips of two adjacent spinous processes, and merges with the insertions of the lumbodorsal muscles. Some authors consider the supraspinous ligament as not being a true ligament, as it seems to consist largely of tendinous fibers, derived from the back muscles. The effect of the supraspinous ligaments on the stability of the lumbar spine should not be underestimated. Because the ligament is positioned further away from the axis of rotation and due to its attachments to the thoracolumbar fascia, it will have more effect in resisting flexion than all the other dorsal ligaments.
The intertransverse ligaments are thin membraneous structures joining two adjacent transverse processes. They are intimately connected to the deep musculature of the back.
Theiliolumbar ligaments (Fig. 9) are thought to be related to the upright posture. They do not exist at birth but develop gradually from the epimysium of the quadratus lumborum muscle in the first decade of life to attain full differentiation only in the second decade. The ligament consists of an anterior and a posterior part. The anterior band of the iliolumbar ligament is a well-developed, broad band.
The iliolumbar ligaments play an important role in the stability of the lumbosacral junction by restricting both side flexion and rotational movement at the L5–S1 joint and forward sliding of L5 on the sacrum.
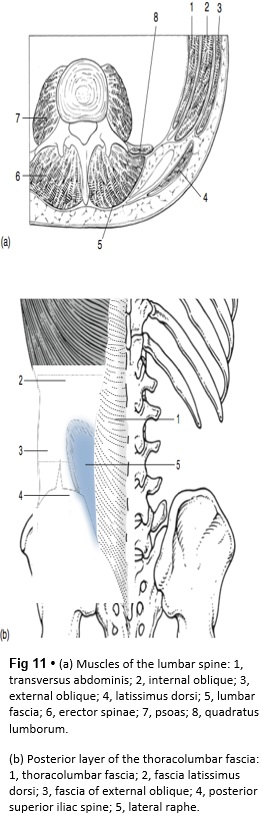
The spine is unstable without the support of the muscles that power the trunk and position the spinal segments. Back muscles can be divided in four functional groups: flexors, extensors, lateral flexors and rotators (Fig. 11).
The extensors are arranged in three layers: the most superficial is the strong erector spinae or sacrospinalis muscle. Its origin is in the erector spinae aponeurosis, a broad sheet of tendinous fibers attached to the iliac crest, the median and lateral sacral crests and the spinous processes of the sacrum and lumbar spine. The middle layer is the multifidus. The fibers of the multifidus are centered on each of the lumbar spinous processes. From each spinal process, fibers radiate inferiorly to insert on the lamina, one, two or three levels below. The arrangement of the fibers is such that it pulls down- wards on each spinal process, thereby causing the vertebra of origin to extend. The third layer is made up of small muscles arranged from level to level, which not only have an extension function but also are also rotators and lateral flexors.
The flexors of the lumbar spine consist of an intrinsic (psoas and iliacus) and an extrinsic group (abdominal wall muscles). Lateral flexors and rotators are the internal and external oblique, the intertransverse and quadratus lumborum muscles. It is important to remember that pure lateral flexion is brought about only by the quadratus lumborum.
Spinal canal
The spinal canal is made up of the canals of individual vertebrae so that bony segments alternate with intervertebral and articular segments. The shape of the transverse section changes from round at L1 to triangular at L3 and slightly trefoil at L5 (Fig. 1). An anterior wall and a posterior wall, connected through pedicles and intervertebral foramina, form the margins of the canal.
The anterior wall consists of the alternating posterior aspects of the vertebral bodies and the annulus of the intervertebral discs. In the midline these structures are covered by the posterior longitudinal ligament, which widens over each intervertebral disc.
The posterior wall is formed by the uppermost portions of the laminae and the ligamenta flava. Because the superoinferior dimensions of the laminae tend to decrease at the L4 and L5 levels, the ligamenta flava consequently occupy a greater percentage of the posterior wall at these levels. The spinal canal contains the dural tube, the spinal nerves and the epidural tissue.
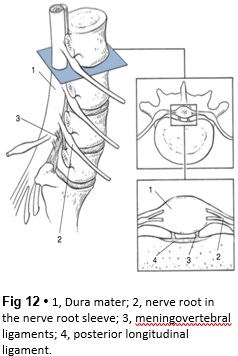
The dura mater is a thick membranous sac, attached cranially around the greater foramen of the occiput, where its fibers blend with the inner periosteum of the skull, and anchored distally to the dorsal surface of the distal sacrum by the filum terminale.
At the lumbar level, the dura contains the distal end of the spinal cord (conus medullaris, ending at L1), the cauda equina and the spinal nerves, all floating and buffered in the cerebrospinal fluid. The lumbar roots have an intra- and extrathecal course. Emerging in pairs from the spinal cord, they pass freely through the subarachnoid space before leaving the dura mater. In their extrathecal course and down to the intervertebral foramen, they remain covered by a dural investment. At the L1 and L2 levels, the nerves exit from the dural sac almost at a right angle and pass across the lower border of the vertebra to reach the intervertebral foramen above the disc. From L2 downwards, the nerves leave the dura slightly more proximally than the foramen through which they will pass, thus having a more and more oblique direction and an increasing length within the spinal canal.
The dura mater has two characteristics that are of cardinal clinical importance: mobility and sensitivity.
Nerve roots
The radicular canal contains the intraspinal extrathecal nerve root. The nerve root consists of a sheath (dural sleeve) and fibres. Each structure has a specific behaviour and function, responsible for typical symptoms and clinical signs. This has some clinical consequences: slight pressure and inflam- mation only involve the sleeve and provoke pain and impaired mobility. More substantial compression of the root will also affect the nerve fibres, which leads to paraesthesia and loss of function.
Epidemiology/Etiology[edit | edit source]
Low back pain is a symptom, not a disease, and has many causes. It is generally described as pain between the costal margin and the gluteal folds. It is extremely common. About 40% of people say that they have had low back pain within the past 6 months. Onset usually begins in the teens to early 40s. A small percentage of low back pain becomes chronic[2,3]. Low back pain is considered acute if its onset occurred less than 1 month ago. The symptoms of chronic low back pain have lasted 2 months or longer. Both acute and chronic low back pain may be further classified as non-specific or specific/radicular[4].
Characteristics/ Clinical Presentation[edit | edit source]
Scoliosis [5]
- Not much pain
- Sideways curvature of the spine
- Muscle strains
- Antalgic posture
- Sideways body posture
- One shoulder raised higher than the other
- Local muscular aches
- Local ligament pain
Scheuermann [6,7,8] :
- History of deformity because of structural kyphosis in adolescence
- In the lumbar spine, hyperlordosis can occur
- Strong correlation between Scheuermann’s disease and scoliosis
- Hamstring thightness
- Back pain, located distal to the apex of the deformity
- Activity related to pain
- Fatigue
- Muscle stiffness (especially at the end of the day)
- Neurological symptoms
- In severe cases: heart and lung function cab be impaired. Other secondary changes are Schmorl nodes, irregular vertebral endplates and dics space narrowing
- Muscle spasms or muscle cramps
- Diffuculty exercising
- Limited flexibility
- Tight hamstrings
Ankylosing spondylitis (Bechterew) [9,10] :
5 phases:
- Acute inflammation
- Damage to the cartilage because of repeatedly acute inflammations
- Damaged cartilage does not heal and is replaced by bone tissue
- Joint loses his flexibility
- Components of the joint grow towards each other and form 1 piece
Important symptoms
- Iridocyclitis or uveïtis (inflammation of the iris)
- Nerve pain in the chest, abdomen of legs
- Morning stiffness lasting greater than 30 minutes and waking up in the second half of the night
- Pain and stiffness increase with inactivity and improve with exercise
- Respiratory complaints
- Inflammation of achilles tendons
- Psoriasis (abnormity of the skin)
- Intestinal problems (Crohn disease)
- Peripheral joints, eyes, skin and the cardiac and intestinal systems problems
- The hips, shoulder and knees are the most commonly and most severely affected of the extremity joints
- Complaints of intermittent breathing difficulties because of a decrease in chest expansion
- Also fatigue, weight loss and fever are indirect effects of inflammation processes. This can lead to severe psychological issues such as depression
Hernia [17] :
Herniated disc not pressing on the nerve:
- No pain
Herniated disc is pressing on the nerve(s):
- Stiffness
- Harp pain
- Tingling and weakness
- Referred pain in legs
- Paralysis
The severity of the complaints depends on the strength of compressive from the hernia on surrounding components.
Radicular syndrome [11,12] :
- Sharp, dull, piercing, throbbing, stabbing, shooting or burning pain
- Numbness, tingling and weakness in the arms or legs
- Radicular pain in one leg
- Neurological loss of function
- Unilateral pain radiating to foot or toes
- Numbness and paraesthesia in the same distribution
- Paravertebral pressure above the nerve root causes pain in the periphery
- Failure of the sensible dermatome
- Nerve root entrapment such as sensory deficits, reflex changes or muscle weakness
Spinal canal stenose [13,14,15] :
- Persisting and heavy pain in the low back
- Referred pain in legs
- Symptoms increase when standing straight
- Laying down/ sitting down/ bending forward decreases the pain
- Areas off the body who are not in pain, can feel itchy and inflamed
- Muscle tension in spine
- Sensibility disorders
- Sleeping disorders
- Incontinence problems
- Sexual dysfunctions
- Immobility of low back
- Pain and/or weakness in legs and buttocks
- Neurogenic intermittent claudication
Spondylolisthesis[16] :
- Instability
- Low back pain
- Stiffness in low back
- Pain in extension
- Referred pain in upper leg
- Immobility low back
- Resting decreases pain
- Trophic changes
- Atrophy of the muscles
- Tense hamstrings
- Disturbance in patterns
- Diminished ROM (spine)
- Disturbances in coordination and balance
- Neurological symptoms (possible evolution towards cauda equina syndrome)
Metastasen [18] :
- Pain increases at night and in rest
- Paralysis
- Compression on the spinal cord resulting in numbness or tingling in the abdomen and legs, bowel and bladder problems, difficulty walking
Cauda equina [19] :
- Difficulties to urinate
- Decrease of sensibility in legs
- Low back pain
- Referred pain in legs
- Sensibility disorders of genital organs
- Difficulty walking
Differential Diagnosis[edit | edit source]
Some conditions can present with similar impairments and should be included in the clinician’s differential diagnosis[20].
Mechanical
- Lumbar muscular strain/sprain
- Compression fracture (www.physio-pedia.com/Lumbar_compression_fracture)
Systemic
- Vertebral discitis/ osteomyelitis (www.physio-pedia.com/Osteomyelitis)
- Connective tissue disease (www.physio-pedia.com/Dermatomyositis)
Referred
- Aortic Abdominal aneurysm (www.physiopedia.com/Abdominal_Aortic_Aneurysm)
- Pancreatitis (www.physio-pedia.com/Pancreatitis)
- Nephrolithiasis (www.physio-pedia.com/Nephrolithiasis_(Kidney_Stones))
Diagnostic Procedures[edit | edit source]
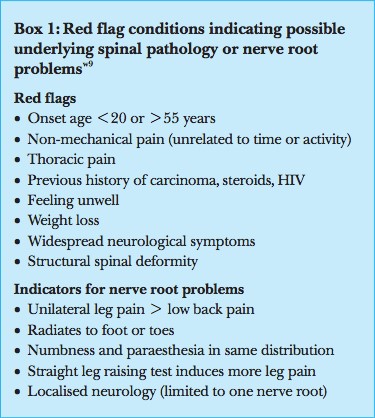
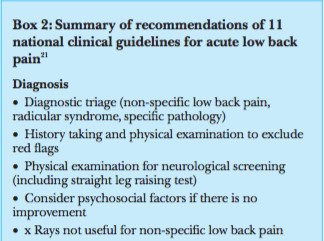
In clinical practice, the triage is focused on identification of “red flags” (see box 1/2) as indicators of possible underlying pathology, including nerve root problems. When red flags are not present, the patient is considered as having non-specific low back pain. Besides those red flags there are yellow flags. Besides the red flags we have to take another kind of flags in consideration, “Yellow flags” have been developed for the identification of patients at risk of chronic pain and disability. A screening instrument based on these yellow flags has been validated for use in clinical practice [21]. The predictive value of the yellow flags and the screening instrument need to be further evaluated in clinical practice and research.
Abnormalities in x-ray and magnetic resonance imaging and the occurrence of non-specific low back pain seem not to be strongly associated [22]. Abnormalities found when imaging people without back pain are just as prevalent as those found in patients with back pain. Van Tulder and Roland reported radiological abnormalities varying from 40% to 50% for degeneration and spondylosis in people without low back pain. They said that radiologists should include this epidemiological data when reporting the findings of a radiological investigation[23]. Many people with low back pain show no abnormalities. In clinical guidelines these findings have led to the recommendation to be restrictive in referral for imaging in patients with non-specific low back pain. Only in cases with red flag conditions might imaging be indicated. Jarvik et al showed that computed tomography and magnetic resonance imaging are equally accurate for diagnosing lumbar disc herniation and stenosis—both conditions that can easily be separated from non-specific low back pain by the appearance of red flags. Magnetic resonance imaging is probably more accurate than other types of imaging for diagnosing infections and malignancies [24], but the prevalence of these specific pathologies is low.
Outcome Measures[edit | edit source]
The following list contains commonly used low back pain outcome measures. But these questionnaires are complete and not patient specific. Often medical imaging has to be done to include specific low back pain disorders but your own clinical judgment will be necessary to determine the most useful measure in your clinical setting.
We found that the ‘Back Illness Pain and Disability 9-item Scale, Quebec Back Pain Disability Index and Roland & Morris Disability Questionnaire’ had a goodfactor of reliability.
The ‘Back Pain Functional scale, Back Pain Interference Scales, Clinical Back Pain Questionnaire, Dallas Pain Questionnaire, Hannover Functional Ability Questionnaire, Oswestry Disability Index, Outcome Measure for lumbar spinal stenosis, Resumption of Activities of Daily Living Scale and Waddell Disability Index’ scored acceptable.(LE: 1B)26(LE:1A)27
Quebec Back Pain Disability Scale (www.physio-pedia.com/Quebec_Back_Pain_Disability_Scale)
Is a condition–specific questionnaire developed to measure the level of functional disability for patients with low back pain. Intended for those who suffer diseases such as acute LBP, chronic pain, lumbar spinal stenosis, posterior surgical decompression.
Oswestry Disability Index [25] (www.physio-pedia.com/Oswestry_Disability_Index)
Patient-completed questionnaire which gives a subjective percentage of level of function (disability) in activities of daily living in those rehabilitation from low back pain. In acute or chronic low back pain.
Roland-Morris Disability Questionnaire (www.physio-pedia.com/Roland%E2%80%90Morris_Disability_Questionnaire
The patient is asked to tick off different statements when it is applied to him, that specific time. It is most sensitive for patients with mild to moderate disability.
Back Pain Functional Scale (www.physio-pedia.com/Back_Pain_Functional_Scale)
Is a self-report measure that evaluates functional ability that is intended for people who are suffering from back pain. It consists of 12 items.
VAS: Visual Analog Scale (www.physio-pedia.com/Visual_Analogue_Scale)