Template:Condition: Difference between revisions
No edit summary |
m (Reverted edits by Amanda E Davidson (Talk); changed back to last version by Colby Boers) |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- | '''Original Editor '''- Your name will be added here if you created the original content for this page. | ||
'''Lead Editors''' - Your name will be added here if you are a lead editor on this page. [[Physiopedia:Editors|Read more.]] | '''Lead Editors''' - Your name will be added here if you are a lead editor on this page. [[Physiopedia:Editors|Read more.]] | ||
| Line 13: | Line 13: | ||
Early dysfunction is the classifed as the beginning of degenerative changes which can occur as early as 20 years. Intermediate instability is classified by a loosening of the annulus fibrosis, which can cause back pain. Fibrosis to the posterior structure and formation of osteophytes denotes the final stabilization classification. Pain decreases, but there is less motion. .<ref> Dutton M. Orthopaedic Examination, Evaluation, and Intervention. 2nd ed. New York, NY: McGraw-Hll; 2008.</ref> <br> | Early dysfunction is the classifed as the beginning of degenerative changes which can occur as early as 20 years. Intermediate instability is classified by a loosening of the annulus fibrosis, which can cause back pain. Fibrosis to the posterior structure and formation of osteophytes denotes the final stabilization classification. Pain decreases, but there is less motion. .<ref> Dutton M. Orthopaedic Examination, Evaluation, and Intervention. 2nd ed. New York, NY: McGraw-Hll; 2008.</ref> <br> | ||
== Mechanism of Injury / Pathological Process<br> == | == Mechanism of Injury / Pathological Process<br> == | ||
| Line 65: | Line 63: | ||
== Management / Interventions<br> == | == Management / Interventions<br> == | ||
add text here relating to management approaches to the condition<br> | |||
== Differential Diagnosis<br> == | == Differential Diagnosis<br> == | ||
Revision as of 21:39, 2 June 2009
Original Editor - Your name will be added here if you created the original content for this page.
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
[edit source]
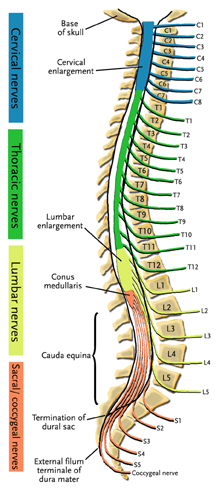
Clinically Relevant Anatomy
[edit source]
Dengenerative Disc Disease (DDD) is thought to begin with changes to the annulus fibrosis, intervertebral disc, and subchondral bone. The process of degeneration is divided into three classifications including: early dysfunction, intermediate instability, and final stabilization.
Early dysfunction is the classifed as the beginning of degenerative changes which can occur as early as 20 years. Intermediate instability is classified by a loosening of the annulus fibrosis, which can cause back pain. Fibrosis to the posterior structure and formation of osteophytes denotes the final stabilization classification. Pain decreases, but there is less motion. .[1]
Mechanism of Injury / Pathological Process
[edit source]
Degenerative disc disease refers to a condition in which the involved disc causes LBP. Lumbar degenerative disc disease is usually the result of a twisting injury to the lower back, such as when a person swings a golf club or rotates to put an object on a surface to the side of or behind them. [2]
The pain is also frequently caused by simple wear and tear on the spine and comes with the general aging process.
Degenerative disc disease is fairly common, and it is estimated that at least 30% of people aged 30-50 years old will have some degree of disc space degeneration, although not all will have pain or ever receive a formal diagnosis. [3]
The process that leads to DDD begins with structural changes. The annulus fibrosis (outer portion of the disc) loses water content over time which will make it increasingly unyielding toward everyday stress and strain on the spine. The loss of compliance in the discs contributes to forces being redirected from the anterior and middle portions of the facets to the posterior aspect, thus causing facet arthritis. Another result is hypertrophy of the vertebral bodies adjacent to the degenerating disc. The overgrowths are known as bony spurs (or osteophytes.)
Clinical Presentation[edit source]
People with DDD will have low back pain; however there are varying levels of severity. Pain is often chronic, but one with DDD can experience varying episodes of exacerbation where pain levels are elevated [4]
DDD commonly occurs with other diagnoses such as:
- idiopathic low-back pain
- lumbar radiculopathy
- myelopathy
- lumbar stenosis
- spondylosis
- osteoarthritis
- zygapophydeal joint degeneration
[5]
Activities that typically increase pain include:
- Sitting for extended periods of time
- Rotating, bending, or lifting
Activities that typically decrease pain include:
- Changing positions often
- Lying down
- Staying active;[6]
Diagnostic Procedures[edit source]
Patients may present with a history of Chronic LBP, and can experience symptoms into the buttock. They may also state a history of spine stiffness that gets worse with activity and tenderness with palpation over involved area. [7]
Xray findings are used to diagnose DDD. Anterior-Posterior and lateral views are taken; presence of osteophytes, narrowing of the disc joint space, or a “vacuum sign” is noted. [8]
Management / Interventions
[edit source]
add text here relating to management approaches to the condition
Differential Diagnosis
[edit source]
Key Evidence[edit source]
add text here relating to key evidence with regards to any of the above headings
Resources
[edit source]
Case Studies[edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Recent Related Research (from Pubmed)[edit source]
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit source]
References will automatically be added here, see adding references tutorial.
- ↑ Dutton M. Orthopaedic Examination, Evaluation, and Intervention. 2nd ed. New York, NY: McGraw-Hll; 2008.
- ↑ Ullrich, P. F. (2006 11 6). Lumbar Degenerative Disc Disease. Retrieved 06 02, 2009, from Degenerative Disc Disease: http://www.spine-health.com/conditions/degenerative-disc-disease/lumbar-degenerative-disc-disease
- ↑ Ullrich, P. F. (2006 11 6). Lumbar Degenerative Disc Disease. Retrieved 06 02, 2009, from Degenerative Disc Disease: http://www.spine-health.com/conditions/degenerative-disc-disease/lumbar-degenerative-disc-disease
- ↑ Ulrich, P. F. (2005, 11 29). Common Symptoms of Degenerative Disc Disease. Retrieved 06 02, 2009, from Degenerative Disc Disease: http://www.spine-health.com/conditions/degenerative-disc-disease/common-symptoms-degenerative-disc-disease
- ↑ Dutton M. Orthopaedic Examination, Evaluation, and Intervention. 2nd ed. New York, NY: McGraw-Hll; 2008.
- ↑ Ulrich, P. F. (2005, 11 29). Common Symptoms of Degenerative Disc Disease. Retrieved 06 02, 2009, from Degenerative Disc Disease: http://www.spine-health.com/conditions/degenerative-disc-disease/common-symptoms-degenerative-disc-disease
- ↑ Thompson, J.C. MD. Netter's Concise Atlas of Orthopaedic Anatomy. (2002) Saunders Elsevier. p.36-7
- ↑ Thompson, J.C. MD. Netter's Concise Atlas of Orthopaedic Anatomy. (2002) Saunders Elsevier. p.36-7