The Role of Hip Surveillance in Cerebral Palsy: Difference between revisions
(references links) |
Amrita Patro (talk | contribs) No edit summary |
||
| Line 1: | Line 1: | ||
== Introduction | == Introduction == | ||
In Cerebral Palsy (CP), the original brain lesion is non-progressive. Unfortunately even though the original brain lesion does not worsen, the children’s musculo-skeletal (muscles and bone) functions deteriorate as they get older and grow into adulthood. Hence one of the greatest practical challenges in CP is maintaining and improving musculo-skeletal function. The hip joint is a common site of musculo-skeletal problems.<br>Hip displacements is related directly to gross motor function as determined by the Gross Motor Function Classification System (Soo et al, 2006, Hagglund et al 2007, Connelly et al 2009, Kentish et al, 2011)<br>Spastic hip displacement is the second most common deformity seen in children with Cerebral Palsy (CP) <ref name="Shore">Shore B, Spence D, Graham H. The role for hip surveillance in children with cerebral palsy. Curr Rev Musculoskelet Med. 2012;5(2):126-134.</ref><br>Hip displacement in CP often occurs already at 2–3 years of age. <ref name="Hägglund">Hägglund G. Characteristics of children with hip displacement in cerebral palsy. BMC musculoskeletal disorders. 2007;8:101-101.</ref> <br>The reported rates of hip displacement and hip dislocation in CP children vary widely and have been reported from 2% to 75% (Bagg et al, 1993)<br>A user-friendly hip surveillance programme that allows for early identification and monitoring is the keystone of management.<br>Hip Surveillance is the process of identifying and monitoring the critical early indicators of progressive hip displacement <ref name="Wynter">Wynter M, Gibson N, Willoughby K, et al. Australian hip surveillance guidelines for children with cerebral palsy: 5-year review. Dev Med Child Neurol. 2015;57(9):808-820.</ref>. Early identification is an essential part of the strategy for the prevention of hip dislocation and its sequelae.<br> | In Cerebral Palsy (CP), the original brain lesion is non-progressive. Unfortunately even though the original brain lesion does not worsen, the children’s musculo-skeletal (muscles and bone) functions deteriorate as they get older and grow into adulthood. Hence one of the greatest practical challenges in CP is maintaining and improving musculo-skeletal function. The hip joint is a common site of musculo-skeletal problems.<br>Hip displacements is related directly to gross motor function as determined by the Gross Motor Function Classification System (Soo et al, 2006, Hagglund et al 2007, Connelly et al 2009, Kentish et al, 2011)<br>Spastic hip displacement is the second most common deformity seen in children with Cerebral Palsy (CP) <ref name="Shore">Shore B, Spence D, Graham H. The role for hip surveillance in children with cerebral palsy. Curr Rev Musculoskelet Med. 2012;5(2):126-134.</ref><br>Hip displacement in CP often occurs already at 2–3 years of age. <ref name="Hägglund">Hägglund G. Characteristics of children with hip displacement in cerebral palsy. BMC musculoskeletal disorders. 2007;8:101-101.</ref> <br>The reported rates of hip displacement and hip dislocation in CP children vary widely and have been reported from 2% to 75% (Bagg et al, 1993)<br>A user-friendly hip surveillance programme that allows for early identification and monitoring is the keystone of management.<br>Hip Surveillance is the process of identifying and monitoring the critical early indicators of progressive hip displacement <ref name="Wynter">Wynter M, Gibson N, Willoughby K, et al. Australian hip surveillance guidelines for children with cerebral palsy: 5-year review. Dev Med Child Neurol. 2015;57(9):808-820.</ref>. Early identification is an essential part of the strategy for the prevention of hip dislocation and its sequelae.<br> | ||
== | == Effects of Hip Displacements. == | ||
1. Progressive hip displacements can lead to hip dislocations<br>2. Severe pain<br>3. Impaired function i.e. loss of mobility, inability to be correctly positioned, compromised personal and hygiene care<br>4. Decrease in quality of life<br> | 1. Progressive hip displacements can lead to hip dislocations<br>2. Severe pain<br>3. Impaired function i.e. loss of mobility, inability to be correctly positioned, compromised personal and hygiene care<br>4. Decrease in quality of life<br> | ||
== | == Mechanism of Hip Displacement, Dislocation and sequelae == | ||
The actual mechanism is not fully understood. It is believed that the hip joint in CP children is normal at birth <ref name="Gibson">Gibson N.CEREBRAL PALSY The importance of monitoring hips in Cerebral Palsy. Princess Margaret Hospital, Perth July 2012</ref>. In CP, hip displacement appears to be associated with muscle imbalances around the hip joint and changes to the shape of the acetabulum and femoral head.<br>Progressive hip displacement refers to the gradual displacement of the femoral head laterally out of the acetabulum. This displacement is expressed as a migration percentage (MP)<br>[[Image:Hip dislocation1.png|center]]<br> | The actual mechanism is not fully understood. It is believed that the hip joint in CP children is normal at birth <ref name="Gibson">Gibson N.CEREBRAL PALSY The importance of monitoring hips in Cerebral Palsy. Princess Margaret Hospital, Perth July 2012</ref>. In CP, hip displacement appears to be associated with muscle imbalances around the hip joint and changes to the shape of the acetabulum and femoral head.<br>Progressive hip displacement refers to the gradual displacement of the femoral head laterally out of the acetabulum. This displacement is expressed as a migration percentage (MP)<br>[[Image:Hip dislocation1.png|center]]<br> | ||
| Line 17: | Line 17: | ||
[[Image:Hip dislocation2.jpg|center|718x1010px]]<br> | [[Image:Hip dislocation2.jpg|center|718x1010px]]<br> | ||
== Common Management Method | == Common Management Method == | ||
Assessment of range of movement (ROM) of the hip. Unfortunately, hip ROM is not an indicator of risk and not useful for screening <ref name="Hägglund" /><br> | Assessment of range of movement (ROM) of the hip. Unfortunately, hip ROM is not an indicator of risk and not useful for screening <ref name="Hägglund" /><br> | ||
== | == Recommended Management Approach == | ||
1. A screening programme based on Gross Motor Function Classification System (GMFCS).<br>2. X-ray of hips as early as possible.<br>3. Clinical assessment including relevant documentation, care, comfort, pain; child’s spine, pelvis and lower limbs.<br>3. Frequency of surveillance: Regularly until skeletal maturity or until discharge <ref name="Gibson" /><br><br> | 1. A screening programme based on Gross Motor Function Classification System (GMFCS).<br>2. X-ray of hips as early as possible.<br>3. Clinical assessment including relevant documentation, care, comfort, pain; child’s spine, pelvis and lower limbs.<br>3. Frequency of surveillance: Regularly until skeletal maturity or until discharge <ref name="Gibson" /><br><br> | ||
| Line 56: | Line 56: | ||
<br><br> | <br><br> | ||
[[Category:Occupational Health]] | |||
Revision as of 19:57, 3 October 2018
Introduction[edit | edit source]
In Cerebral Palsy (CP), the original brain lesion is non-progressive. Unfortunately even though the original brain lesion does not worsen, the children’s musculo-skeletal (muscles and bone) functions deteriorate as they get older and grow into adulthood. Hence one of the greatest practical challenges in CP is maintaining and improving musculo-skeletal function. The hip joint is a common site of musculo-skeletal problems.
Hip displacements is related directly to gross motor function as determined by the Gross Motor Function Classification System (Soo et al, 2006, Hagglund et al 2007, Connelly et al 2009, Kentish et al, 2011)
Spastic hip displacement is the second most common deformity seen in children with Cerebral Palsy (CP) [1]
Hip displacement in CP often occurs already at 2–3 years of age. [2]
The reported rates of hip displacement and hip dislocation in CP children vary widely and have been reported from 2% to 75% (Bagg et al, 1993)
A user-friendly hip surveillance programme that allows for early identification and monitoring is the keystone of management.
Hip Surveillance is the process of identifying and monitoring the critical early indicators of progressive hip displacement [3]. Early identification is an essential part of the strategy for the prevention of hip dislocation and its sequelae.
Effects of Hip Displacements.[edit | edit source]
1. Progressive hip displacements can lead to hip dislocations
2. Severe pain
3. Impaired function i.e. loss of mobility, inability to be correctly positioned, compromised personal and hygiene care
4. Decrease in quality of life
Mechanism of Hip Displacement, Dislocation and sequelae[edit | edit source]
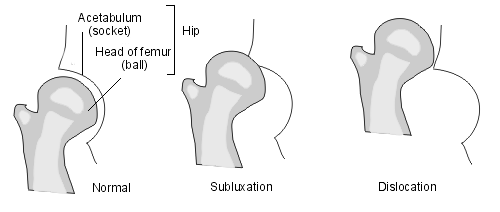
The actual mechanism is not fully understood. It is believed that the hip joint in CP children is normal at birth [4]. In CP, hip displacement appears to be associated with muscle imbalances around the hip joint and changes to the shape of the acetabulum and femoral head.
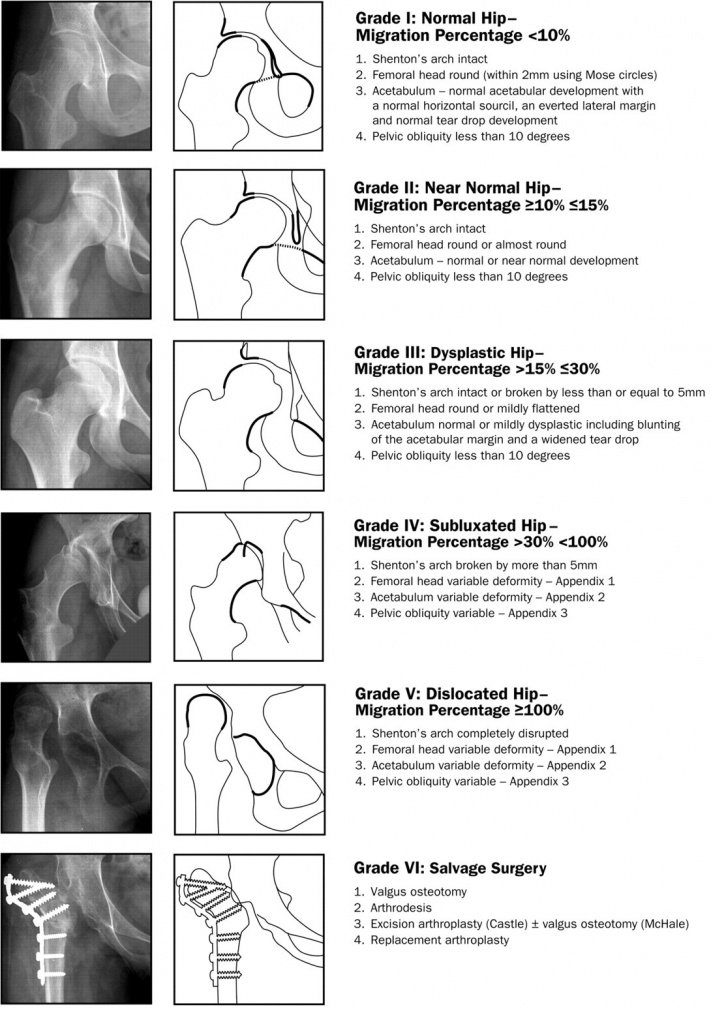
Progressive hip displacement refers to the gradual displacement of the femoral head laterally out of the acetabulum. This displacement is expressed as a migration percentage (MP)
Hip displacement/ subluxation: Refers to hip displacement where MP is between 10% to 99% [3]. Hip dislocation: refers to when the femoral head is completely displaced laterally out of the acetabulum. MP = 100% [4]
Common Management Method[edit | edit source]
Assessment of range of movement (ROM) of the hip. Unfortunately, hip ROM is not an indicator of risk and not useful for screening [2]
Recommended Management Approach[edit | edit source]
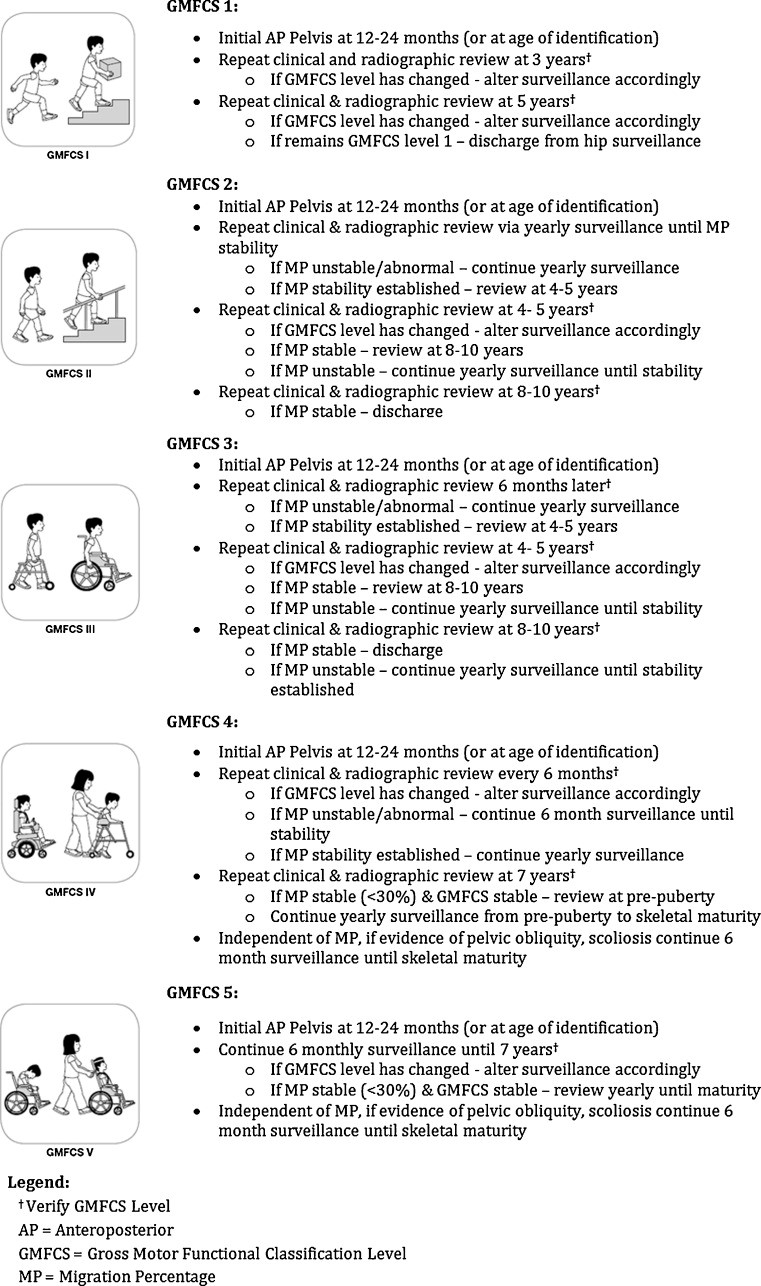
1. A screening programme based on Gross Motor Function Classification System (GMFCS).
2. X-ray of hips as early as possible.
3. Clinical assessment including relevant documentation, care, comfort, pain; child’s spine, pelvis and lower limbs.
3. Frequency of surveillance: Regularly until skeletal maturity or until discharge [4]
Recommended Frequency of Hip Surveillance According to GMFCS (Adapted from Wynter et al)
Challenges to Hip Surveillance in the South African Context[edit | edit source]
- Many therapists are not adequately trained to use the GMFCS, which is the recommended basis for developing a Hip Surveillance Screening Tool.
- There is a lack of a standardized, universal Hip Surveillance Screening tool and guidelines with sufficient training for users.
- Lack of resources.
References[edit | edit source]
- ↑ Shore B, Spence D, Graham H. The role for hip surveillance in children with cerebral palsy. Curr Rev Musculoskelet Med. 2012;5(2):126-134.
- ↑ 2.0 2.1 Hägglund G. Characteristics of children with hip displacement in cerebral palsy. BMC musculoskeletal disorders. 2007;8:101-101.
- ↑ 3.0 3.1 Wynter M, Gibson N, Willoughby K, et al. Australian hip surveillance guidelines for children with cerebral palsy: 5-year review. Dev Med Child Neurol. 2015;57(9):808-820.
- ↑ 4.0 4.1 4.2 Gibson N.CEREBRAL PALSY The importance of monitoring hips in Cerebral Palsy. Princess Margaret Hospital, Perth July 2012