Tibialis posterior rupture: Difference between revisions
Tim Hendrikx (talk | contribs) No edit summary |
Tim Hendrikx (talk | contribs) No edit summary |
||
| Line 46: | Line 46: | ||
== Examination == | == Examination == | ||
'''<u></u>Observation:'''<ref name="Randall E. Marcus">Randall E. Marcus, M. E. . The enigmatic diagnosis of posterior tibialis tendon rupture. The Iowa Orthopedical Journal , 1993, 2B: 171-177</ref> | |||
Posterior tibialis tendon rupture is strongly suspected in patients presenting a complex of findings. These include: | |||
• Eversion ankle injury<br>• Generalized medial ankle pain<br>• Medial ankle swelling<br>• Flexible, asymmetric pes planus and forefoot pronation<br>• Gait disturbance secondary to deformity<br>• Talonavicular sag in lateral standing radiograph | |||
The first four findings are nondiagnostic, however, seen together they are helpful in identifying patients with posterior tibialis tendon pathology. Manual testing of the posteroir tibialis tendon should be performed in the presence of these findings to confirm the tendon's functional status. | |||
<br>'''Tests:'''<ref name="A. Foster">A. Foster, N. T. Rupture of the tibialis posterior tendon: an important differential in the assessment of ankle injuries. Ermergency Medical Journal , 2005 (4): 915-916</ref> | |||
• Palpation from area between malleolus medialis and os naviculare<br>• “Too many toes” sign secondary to an increase in forefoot abduction and heel eversion<br>• Nonfunctional posterior tibialis tendon on manual testing<br>• Motion of the ankle and subtalar joints<br>• Positive first metatarsal rise sign test<br>• Positive single-limb heel rise-test<br>• [http://www.physio-pedia.com/Ottawa_Ankle_Rules Ottawa ankle rules test] to exclude fractures within the first week after an ankle injury<br> | |||
[[Image:Too_many_toes.JPG]] | |||
<br> | |||
== Medical Management <br> == | == Medical Management <br> == | ||
Revision as of 13:48, 30 December 2012
Original Editors
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Search Strategy[edit | edit source]
Databases Searched: Pubmed, ADB, web of knowledge, PEDro, The Journal of Joint and Bone Surgery, Dynamed, PhysioAdvisor
Keyword Searches: tibialis posterior tendon (TPT) , tibialis posterior rupture (TPR), tibialis posterior tendon rupture (TPTR), TPTR treatment, TPTR postoperative treatment, flatfoot, pes planovalgus, tendinitis
Definition/Description[edit | edit source]
Whenever the tibialis posterior muscle contracts or is stretched, tension is placed through the tibialis posterior tendon. If this tension is excessive due to too much force or repetition, damage to the tibialis posterior tendon may occur. This can range from minor tearing of the tendon with subsequent inflammation to a complete tibialis posterior tendon rupture. Early diagnosis and surgical repair will restore full normal function. [1]
A rupture of the posterior tibial tendon can be easily missed because the symptoms of this injury resemble the symptoms of a normal ankle sprain. Some physicians may feel that posterior tibial tendon rupture is a rare condition, one that they have never seen.
Clinically Relevant Anatomy[edit | edit source]
Epidemiology /Etiology[edit | edit source]
Posterior tibialis tendon ruptures occur predominantly in the late middle-aged population (average age 57 years). For posterior tibialis dysfunction, the patient is typically a female over the age of 40 who exhibits ligamentous laxity in multiple joints and has an occupation that requires extended periods of standing. They usually do not recall any acute traumatic event. There is another subset of the populations in which posterior tibial tendon insufficiency occurs and that consists of the 20- to 40-year old athletes. They usually recall a traumatic event, usually a direct blow to the medial malleolus. Or, they present with years of involvement in athletics with a pronated foot.[1]
Characteristics/Clinical Presentation[1][edit | edit source]
• Swelling along the medial aspect of the foot and ankle
• Absence of the classical sudden severe pain of a tendon rupture
• Tenderness along the posterior tibialis tendon
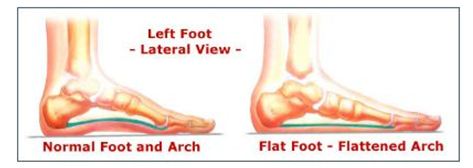
• Progressive loss of longitudinal arch → pes planus and heel valgus
• Palpable pain between medial malleolus and navicular
• Pain in the plantar medial arch
Differential Diagnosis[2][edit | edit source]
• Attenuation or rupture of the calcaneonavicular (spring) ligament complex
• Degenerative arthritis of the ankle joint with valgus talar
• Arthritis of the talonavicular joint
• Posttraumatic tarsometatarsal (Lisfranc) joint arthritis
• Inflammatory arthritis of the hindfoot, usually secondary to rheumatoid disease
Diagnostic Procedures[edit | edit source]
add text here related to medical diagnostic procedures
Outcome Measures[edit | edit source]
add links to outcome measures here (also see Outcome Measures Database)
Examination[edit | edit source]
Observation:[3]
Posterior tibialis tendon rupture is strongly suspected in patients presenting a complex of findings. These include:
• Eversion ankle injury
• Generalized medial ankle pain
• Medial ankle swelling
• Flexible, asymmetric pes planus and forefoot pronation
• Gait disturbance secondary to deformity
• Talonavicular sag in lateral standing radiograph
The first four findings are nondiagnostic, however, seen together they are helpful in identifying patients with posterior tibialis tendon pathology. Manual testing of the posteroir tibialis tendon should be performed in the presence of these findings to confirm the tendon's functional status.
Tests:[4]
• Palpation from area between malleolus medialis and os naviculare
• “Too many toes” sign secondary to an increase in forefoot abduction and heel eversion
• Nonfunctional posterior tibialis tendon on manual testing
• Motion of the ankle and subtalar joints
• Positive first metatarsal rise sign test
• Positive single-limb heel rise-test
• Ottawa ankle rules test to exclude fractures within the first week after an ankle injury
Medical Management
[edit | edit source]
add text here
Physical Therapy Management
[edit | edit source]
add text here
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
add appropriate resources here
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 1.2 William M. Geideman, J. E. Posterior Tibial Tendon Dysfunction. Journal of Orthopedic & Sports Physical Therapy , 2000, (2A SR): 68-77
- ↑ Johnson KA, S. D. (1989). Posterior Tibialis Tendon Dysfunction. Clinical Orthopedical Rel. , 1989, 196-206
- ↑ Randall E. Marcus, M. E. . The enigmatic diagnosis of posterior tibialis tendon rupture. The Iowa Orthopedical Journal , 1993, 2B: 171-177
- ↑ A. Foster, N. T. Rupture of the tibialis posterior tendon: an important differential in the assessment of ankle injuries. Ermergency Medical Journal , 2005 (4): 915-916