Ulnar Impaction Syndrome
Original Editors
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Search Strategy[edit | edit source]
Databases Searched: Academic Search Complete, CINAHL Plus, Medline, SPORTDiscus
Keywords: ulnar impaction, ulnar impaction syndrome, ulnar wrist pain
Search Timeline: October 5 - November 20, 2011
Definition/Description
[edit | edit source]
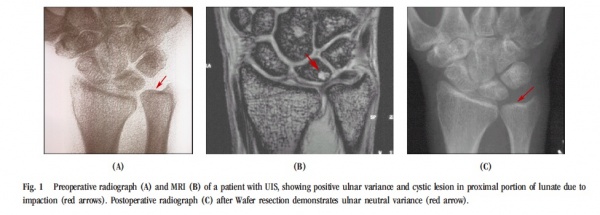
Ulnar impaction syndrome, also called ulnocarpal abutment syndrome, is a common cause of ulnar-sided wrist pain (Sammer, Katz).[1] It is a degenerative condition in which the ulnar head abuts the triangular fibrocartilage complex (TFCC) and ulnar-sided carpals (Harvey, Baek). This abutment results in increased load bearing across the ulnar head, TFCC and ulnar carpals, and subsequent degeneration of the TFCC, chondromalacia of the osseous structures involved (ulna and carpals, especially the lunate), and disruption of the triquetrolunate ligament (Katz, Masahiro).
Epidemiology/Etiology[edit | edit source]
The most common pre-disposing factor for Ulnar Impaction Syndrome (UIS) is positive ulnar variance - that is, an increased ulnar length relative to the radius. Positive ulnar variance has been found to inversely relate to TFCC thickness; thus, in the positive ulnar variance wrist, the TFCC is stretched and thin, and greater biomechanical forces, particularly rotation forces, impact the joint. This positive variance can result from[2] [3](LaStayo, Sachar, Baek, Katz):
- a congenital positioning of the ulnar articular surface more distally than the radial articular surface
- acquired radial shortening secondary to trauma - for example, a malunion of the radius after a distal radius fracture, an Essex-Lopresti injury, proximal migration of the radius after radial head excision, or premature physeal closure of the radius
- excessive dynamic ulnar variance -- greater than normal distal movement of the ulna during forearm pronation and gripping
Wrists that do not have a positive ulnar variance, but are considered "ulnar neutral" or "ulnar negative" can also acquire UIS because variance can increase during functional activities, especially those that include forearm pronation and gripping (Tomaino, Webb, LaStayo).[2][4] When ulnar variance increases in wrists that are ulnar negative or neutral (and thus have a thicker TFCC), ulnocarpoal load also increases (Sammer).[1] Therefore, although UIS is most common in those with an ulnar positive wrist, it can also occur in wrists with either negative or neutral variance (Tomaino).
Characteristics/Clinical Presentation[edit | edit source]
Ulnar impaction syndrome is insidious and progressive, so patients can have the syndrome without symptoms or can be severely symptomatic when presenting to physical therapy. Common symptoms are: pain, occasional edema, decreased wrist range of motion, decreased forearm rotation, and tenderness to palpation dorsally just distal to the ulnar head and just volar to the ulnar styloid process. The symptoms are commonly aggravated by forceful grip, forearm pronation, and ulnar deviation.[1] (SAMMER 2010)
Differential Diagnosis
[edit | edit source]
Ulnar wrist pathologies often present very similarly in impairment and pain pattern. Thus, radiographic imaging is required to confirm diagnosis in almost all cases of ulnar-sided wrist pain, and should be considered after the history-taking and clinical exam.
Note: TFCC Injury often occurs secondary to or in conjunction with ulnar impaction syndrome.
| DISORDER | SIGNS & SYMPTOMS | TESTS |
|---|---|---|
| TFCC Injury | - Ulnar wrist pain - Snapping or clicking |
- TFCC compression test - Piano key sign - Supination lift test - Palpation |
| Lunotriquetral Interosseous Ligament (LTIL) Injury | - Joint tenderness - Decreased ROM - Decreased grip strength - Painful clunk with radial& & ulnar deviation |
- Ballottement test - Shuck test - Shear test - Ulnar snuffbox test |
| Arthritis - DRUJ -Pisotriquetral |
- Pain & crepitus with loading - Decreased ROM - Decreased grip strength - Localized pain |
- Grind tests - Palpation of joint lines - Ballottement tests - ROM |
| DRUJ Instability | - Pain with forearm rotation | - Grind test - Palpation |
| ECU Pathology[1] | - Pain specific to ECU tendon - ECU subluxation |
- Palpation of ECU tendon over ulnar head - Resisted wrist extension & ulnar deviation - Active forearm supination & ulnar deviation |
| Fracture - Ulnar styloid - Triquetrum - Hamate . |
- Tenderness & edema - Decreased ROM - Decreased wrist strength - Pain with motion |
- Palpation of bony landmarks - DRUJ stability (ulnar styloid) - Resisted 5th digit flexion (hamate) |
| Midcarpal Instability | - Midcarpal clunk with ulnar deviation & pronation - Volar sag at ulnar wrist - Often bilateral |
- Midcarpal shift test |
| Kienbock's Disease | - Chronic wrist pain without trauma - Tender dorsal lunate - Decrease ROM - Decreased grip strength - Arthritis (late stage) |
- Palpate lunate |
| Ulnar Nerve Entrapment | - Paresthesia to 4th & 5th digits - Hand intrinsic weakness |
- Tinel's to Guyon's Canal - History/pattern of symptoms |
| Ulnar Artery Thrombosis | - Night pain - Pain with repetitive activity - Cold intolerance - Exquisite tenderness at site of pathology - Dependent rubor or ulceration or 4th or 5th fingertips - Sympathetic fiber excitation of ulnar proper digital nerves |
- Allen test |
| DUCN Neuritis | - Sensory changes to 4th & 5th digits - Pain or sensory changes at elbow and/or hand weakness, indicative of more proximal ulnar nerve pathology . |
- Sensory exam - Palpation - Wartenburg sign (motor pathology) - Froment sign (motor pathology) |
Outcome Measures[edit | edit source]
add links to outcome measures here (also see Outcome Measures Database)
Examination[edit | edit source]
To diagnose ulnar impaction syndrome,a comprehensive wrist exam must be completed. Diagnostic imaging should be performed to support the findings from the clinical exam. The physical therapist should pay specific attention to the following:
• Palpation[4][5] (Vezeridis 2010, Webb)
o Tenderness dorsally just distal to ulnar head
o Tenderness just volar to the ulnar styloid process
o Positive ulnar variance, while static or dynamic
• Range of Motion[6][4][5] (Tatebe, Vezeridis, Webb)
o Painful passive ulnar deviation and forceful pronation
o Decreased flexion, extension, radial & ulnar deviation
• Strength[4][5] (Tomaino, Vezeridis, Webb)
o Decreased grip strength, using dynamometer
• Ulnocarpal stress test[7] (Nakamura)
o Place wrist in maximum ulnar deviation
o Apply axial load to wrist
o Passively rotate forearm through supination and pronation
o + Test = reproduction of patient’s pain
NOTE- Test is sensitive for UIS but can get positive with other pathologies, such as LTIL injury, TFCC injury or isolated arthritis.
• Gripping Rotary Impaction Test (GRIT)[2] (LaStayo)
o Place arm by side and elbow in 90 degrees of flexion
o Using a grip dynamometer, measure grip in 3 positions: neutral, full supination, full pronation
o GRIT Ratio=(supinated grip strength)/(pronated grip strength)
GRIT ratio is greater than 1.0 indicates UIS
Examination of the TFCC and lunotriquetral ligament integrity may be necessary, especially in patients with suspected long-term ulnar impaction syndrome due to commonly seen degeneration of these structures.[3] (Sachar)
• Imaging – used to support physical examination findings
o Radiograph[1][8][6][4] (Sammer, Tatebe, Webb, Watanabe)
Views:
• Neutral rotation P-A radiograph with elbow in 90° flexion
• Pronated grip P-A radiograph
May have subchondral sclerosis, cystic changes, or osteophyte formation
Positive ulnar variance is the hallmark of UIS
o MRI[8][4][5] (Vezeridis, Webb, Watanabe)
Detects tears to TFCC and other soft tissue injuries
May detect decrease in vascular profusion of the lunate and ulnar head or anatomical abnormalities
o Arthrography[8][4][9] (Webb, Watanabe, Shin 2004)
Currently, considered “gold standard” at detecting damage to TFCC
Although, recent research is refuting this because of high rates of false-negatives and poor correlation between findings and patient presentation, and stating MRI is more effective
Criteria for Ulnocarpal Abutment Syndrome[7] (Nakamura 1997)
1. Ulnar wrist pain with tenderness just distal to the ulnar head (dorsal and/or palmar)
2. Ulceration or cystic lesion of the lunate ulnar base and/or ulnar head of radiography, OR low signal intensity of the lunate ulnar base on T1-weighted images of MRI, OR degenerative lesions of the TFCC on arthroscopy (Palmer’s class 2 lesion).
Medical Management[edit | edit source]
Diagnosed:[3] (Sachar 2008)
o Standard radiographs allows measurements of scapholunate, scapocapitate, ulnar variance and carpal alignment
o CT scan for pathology of DRUJ
o Arthroscopy is the “gold standard” for identifying lesions
o Magnetic Resonance Arthrography with contrast is accurate in ruling in and out TFCC tears
o Fluoroscopy used to assess dye leakage
Surgery options:
- Ulnar shortening osteotomy
o Ulna is shortened, 2-3mm removed and held together by plate
o Baek et al showed significant improvement in Gartland & Werley scores.
- Pre-Op: 24 wrist rated poor , 7 fair
- Post-Op: 24 excellent, 5 good, 1 fair
- Reduced subluxation of distal radio-ulnar jt and degenerative cystic changes of ulnar carpal bones resolved.
o Chen et al showed 100% union in 6-8 wks, 72% excellent results on Gartland & Werley
- Arthroscopic wafer procedure[10]
Meftah et al
- TFCC debridement before 2.3mm resection from distal ulna
- Good to excellent results 85-100%. Near full ROM, but grip strength did not improve.
- Those who have history of distal radius fracture had more pain after surgery
Tomanino et al
- combined arthroscopic TFCC debridement and wafer resection.
- complete pn relief in 8/12 patients and increase in grip strength 36%
Feldon et al
- 69% excellent and 31% good results for open wafer procedure
- Longer recovery
-Bowers procedure
- resection of ulnar articular head, leaving shaft and styloid relationship intact
- Used if TFCC is intact or able to be reconstructed (Wheeles website)
- Darrach Procedure
- ulnar head excision if TFCC is not able to be reconstructed (Wheeles website)
Complications[11][10]:
- Scars, infection, dorsal sensory branch of ulnar nerve damage, delayed or non-union (www.pncl.co.uk/belcherl/information/ulnar%20ossteotomy.pdf), tendonitis of ECU sheath (Meftah et al)
Pre-op:[10] (Meftah et al)
- Brace immobilization
- Occupational therapy
- Cortisone injections
- Activity modifications ~ 3 months
Post-op[11][10]:www.pncl.co.uk/belcherl/information/ulnar%20ossteotomy.pdf
- Immobilization 1-2 wks, referred to OT (Meftah et al)
- Hand elevation to prevent swelling
- X-ray at 6wks to make sure bones are uniting
- 12-16 weeks before returning to heavy activities
Physical Therapy Management
[edit | edit source]
Conservative treatment should be attempted before surgery.[1] (Sammer & Rizzo 2010)
Treatment is symptom based and can include immobilization for 6-12 weeks, NSAIDs, corticosteroid injection and limiting aggravating movements such as pronation, gripping and ulnar deviation. Lack of improvement with conservative management is an indication for surgery[1] (Sachar 2008, Sammer & Rizzo 2010, LaStayo 2001).[2][3]
UIS can be associated with class 2 TFCC injury [3][12] and treatment should also address this if present (Sacher 2008, EORIF.com, Wantanabe 2010) as well as impairments resulting from immobilization.
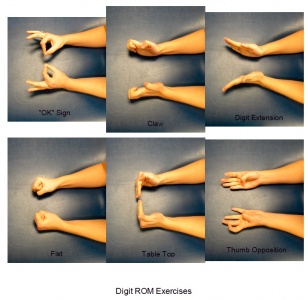
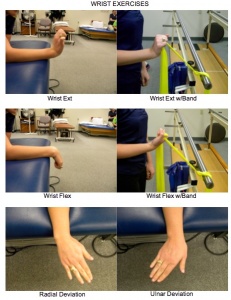
Example Post-Surgery Protocol[1][12][11][13]</(EORIF.com, Sammer 2010, PNCL, Marti 2008)
| Timeframe | Goals | Bracing/Splinting | Physical Agents | TherEx | Manual Techniques |
|---|---|---|---|---|---|
| 0 - 2 wks | - Control pain & swelling - Protect surgical site - Maintain ROM in unaffected jts |
- Sugar-tong splint - Long-arm cast |
- Ice - Pain medication |
- NWB - Elevation for edema - Shoulder ROM - Digit ROM |
|
| 2 - 6 wks | - Protect surgical site - Maintain ROM in unaffected jts - Increase elbow & wrist ROM - Prevent contractures |
- Removable elbow-hinged splint or wrist cock-up brace |
- See above - as needed |
- Limited wrist & forearm ROM oustide splint - Stretching of elbow & wrist - Avoid loaded pronation & supination - Continue shoulder & digit ROM |
- Soft tissue massage |
| 6 - 8 wks | - Increase elbow & wrist ROM - Increase UE strength |
- Removable splint worn at night |
- See above - as needed |
- Full AROM of elbow & wrist - Stretching of elbow & wrist - Isometric elbow flex/ext & supi/pronation |
- Soft tissue massage |
| 12 - 16 wks | - Address remaining ROM & strength impairments |
- Splint may still be worn at night |
- See above - as needed |
- Full AROM of elbow & wrist - UE strength training |
- Soft tissue massage - Mobilization of elbow forearm & wrist* |
*If evidence of bony union present, Full union expected by 3 months.
Return to unrestricted activity is expected by 6 months to 1 year post-surgery.
ROM exercises should be low-load and high repetition within pain limitations and as per MD protocol.
Example Exercises
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Sammer DM, Rizzo M. Ulnar impaction. Hand Clin. 2010; 26: 549-557.
- ↑ 2.0 2.1 2.2 2.3 LaStayo P, Weiss S. The GRIT: A qualitative measure of ulnar impaction syndrome. J Hand Ther. 2001; 14(3): 173-179.
- ↑ 3.0 3.1 3.2 3.3 3.4 Sachar K. Ulnar-sided wrist pain: Evaluation and treatment of triangular fibrocartilage complex tears, ulnocarpal impaction syndrome, and lunotriquetral ligament tears. J Hand Surg. 2008; 33A: 1669-1679.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Webb B, Rettig L. Gymnastic wrist injuries. Current Sports Medicine Reports. September 2008;7(5):289-295.
- ↑ 5.0 5.1 5.2 5.3 Vezeridis PS, Yoshioka H, Han R, Blazar P. Ulnar-sided wrist pain. Part 1: anatomy and physical examination. Skeletal Radiol. 2010; 39:733-745.
- ↑ 6.0 6.1 Tatebe M, Nakamura R, Horii E, Nakao E, Inagaki H. Ulnocarpal impaction syndrome restricts even midcarpal range of motion. J Hand Surgery. July 2005;10(1):23-27.
- ↑ 7.0 7.1 Nakamura R, Horii E, Imaeda T, Nakao E, Kato H, Watanabe K, The ulnocarpal stress test in the diagnosis of ulnar-sided wrist pain, J Hand Surg. 1997; 22B:719–723.
- ↑ 8.0 8.1 8.2 Watanabe A, Souza F, Vezeridis PS, Blazar P, Yoshioka H. Ulnar-sided wrist pn II. Clinical imaging and treatment. Skeletal Radiol. 2010; 39: 837-857.
- ↑ Shin AY, Deitch MA, Sachar D, Boyer MI. Ulnar-Sided Wrist Pain: Diagnosis and Treatment. J Bone Joint Surg. July 2004;86A(7):1560-1574.
- ↑ 10.0 10.1 10.2 10.3 Meftah M, Keefer EP, Panagopoulos G, Yang SS. Arthroscopic wafer resection for ulnar impaction syndrome: Prediction of outcomes. J Hand Surg. 2010; 15(2): 89-93.
- ↑ 11.0 11.1 11.2 Belcher HJ. Ulnar Osteotomy. Available at: http://www.pncl.co.uk/~belcher/information/Ulnar%20osteotomy.pdf. Accessed November 18, 2011.
- ↑ 12.0 12.1 Ulnocarpal Impaction Syndrome. Available at: http://eorif.com/WristHand/UlnocarpalImpaction.html. Accessed November 18, 2011.
- ↑ Marti RK, van Heerwaarden RJ. Osteotomies for posttraumatic deformities. Thieme; 2008: 221-22.