Ventricular Tachycardia: Difference between revisions
Justin Bryan (talk | contribs) No edit summary |
Justin Bryan (talk | contribs) No edit summary |
||
| Line 5: | Line 5: | ||
== Introduction == | == Introduction == | ||
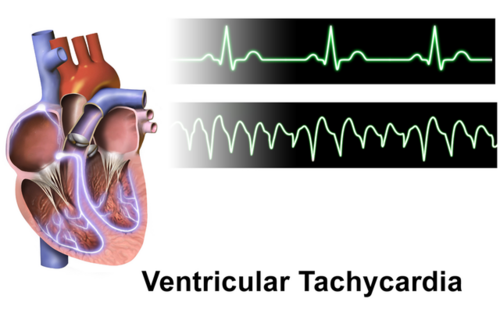
[[File:Ventricular Tachycardia.png|right|frameless|500x500px]] | [[File:Ventricular Tachycardia.png|right|frameless|500x500px]] | ||
Ventricular tachycardia (V-Tach) is a type of cardiac arrhythmia where the ventricle beats at 100 or more beats per minute for 3 or more consecutive beats. Unlike more | Ventricular tachycardia (V-Tach) is a type of cardiac arrhythmia where the ventricle beats at a rate of 100 or more beats per minute for a duration of 3 or more consecutive beats. Unlike the more common form of [[tachycardia]] that originates from the atria (supraventricular tachycardia), the increased rate seen with V-Tach originates from the cells of the ventricles themselves. At rates greater that 100 bpm, the pumping ability of the ventricles is severely degraded, resulting in significant risk for severe symptoms and even [[Cardiac Arrest|cardiac arrest]]. V-Tach is considered a life-threatening cardiac arrhythmia.<ref name=":0">Foth C, Gangwani MK, Ahmed I, et al. [https://www.ncbi.nlm.nih.gov/books/NBK532954/ Ventricular Tachycardia] [Internet]. StatPearls. Treasure Island (FL): StatPearls Publishing; 2023. Available from: <nowiki>https://www.ncbi.nlm.nih.gov/books/NBK532954/</nowiki></ref> | ||
Types of Ventricular Tachycardia<ref name=":0" /><ref name=":1">Johns Hopkins Medicine. [https://www.hopkinsmedicine.org/health/conditions-and-diseases/ventricular-tachycardia Ventricular Tachycardia]. Available from: <nowiki>https://www.hopkinsmedicine.org/health/conditions-and-diseases/ventricular-tachycardia</nowiki></ref> | Types of Ventricular Tachycardia<ref name=":0" /><ref name=":1">Johns Hopkins Medicine. [https://www.hopkinsmedicine.org/health/conditions-and-diseases/ventricular-tachycardia Ventricular Tachycardia]. Available from: <nowiki>https://www.hopkinsmedicine.org/health/conditions-and-diseases/ventricular-tachycardia</nowiki></ref> | ||
Revision as of 20:44, 29 March 2023
Top Contributors - Justin Bryan, Lucinda hampton and Kirenga Bamurange Liliane
Introduction[edit | edit source]
Ventricular tachycardia (V-Tach) is a type of cardiac arrhythmia where the ventricle beats at a rate of 100 or more beats per minute for a duration of 3 or more consecutive beats. Unlike the more common form of tachycardia that originates from the atria (supraventricular tachycardia), the increased rate seen with V-Tach originates from the cells of the ventricles themselves. At rates greater that 100 bpm, the pumping ability of the ventricles is severely degraded, resulting in significant risk for severe symptoms and even cardiac arrest. V-Tach is considered a life-threatening cardiac arrhythmia.[1]
Types of Ventricular Tachycardia[1][2]
- Sustained V-Tach - tachycardia lasting longer than 30 seconds
- Non-sustained V-Tach - tachycardia lasting less than 30 seconds; non-sustained V-Tach does no effect the hearts ability to pump to the same degree as sustained V-Tach, symptoms are often more limited and have far less impact on the heart's ability to function
- Idiopathic V-Tach - No know cause, generally considered benign
- Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT) - An inherited genetic condition resulting in V-Tach
Causes and Risk Factors[edit | edit source]
A number of factors can increase the risk of developing V-Tach. Generally, these factors are associated with the pre-existance of cardiac conditions such as acute coronary syndrome or ischemic heart disease. A broad range of cardiomyopathies, including hypertrophic cardiomyopathy, infiltrative cardiomyopathy, and arrhythmogenic right ventricular cardiomyopathy have also been found to be associated with V-Tach. Certain congenital heart defects also carry risk. Other circumstances such as electrolyte imbalances and illicit drug use also increases risk. In the presence of factors such as these, V-Tach can be triggers by situations where the heart is put under certain stresses such as myocardial ischemia, sepsis, or metabolic acidosis. In general, risk is increased by conditions that change the normal conduction of electrical impulses in the heart, such conditions as a heart attach, which results in scaring of myocardial tissue.[1][2]
Certain ion channel pathologies, defects that effect the functioning of the the cellular membrane and passage of ions, also carry an increased risk for V-Tach due to their impact on the conduction and generation of impulses in the heart:[1][3]
- Long QT syndrome
- Brugada syndrome
- Catecholaminergic polymorphic ventricular tachycardia
- Short QT syndrome
- Malignant early repolarization syndrome
V-Tach can also be idiopathic, and in this form is considered benign. Treatment usually involved prescription of calcium channel blockers, and outcomes are generally very positive.[1]
Clinical Presentation[edit | edit source]
Signs and symptoms of sustained V-Tach include those associated with a reduction in the ability of the heart to pump blood such as dizziness, shortness of breath, and fainting or loss of consciousness. Patients may also experience chest pain, a feeling of the heart "fluttering." Cardiac arrest can also occur as a result of V-Tach.[1][2]
The exact characteristics of reduced cardiac function resulting from V-Tach is strongly dependent on the cardiac conditions that the patient has (i.e. cardiomyopathy vs. ischemic heart disease). In general, reduced cardiac output in the main consequence of V-Tach, due directly to a reduction in the ventricle's ability to stretch and fill with blood (preload), as well as the lower volume of blood that is actually pumped with each beat (stroke volume). With cardiac output reduced, the patients, especially those whose heart is already compromised by conditions such as coronary artery disease, may experience hypotension and reduced blood flow to the brain, which can result in syncope. Blood flow to the heart is also reduced, which can lead to a further reduction in cardiac output, ventricular fibrillation, cardiac arrest, or even sudden cardiac death.[1]
Diagnostic Procedures[edit | edit source]
The first line of diagnosis is the administration of an electrocardiogram (ECK or EKG) to monitor the rhythm of the heart. An ECG will be captured when the patient is not experiencing V-Tach, to allow for determination of underlying causes. Then, if possible, an ECG is capture when the patient has an episode of V-Tach to allow for comparison. In patients who have a history of syncope or a diagnosis of CPVT (see above), practitioners may wish to capture an ECG a graded or non-graded exercise test. If the frequency of symptoms makes capturing the event difficult, a loop recorder may be used.[1]
An echocardiagram may also be performed to determine the presence of such conditions as cardiomyopathies, which can increase the risk of developing V-Tach. In more specialized cases, imaging can also be performed through the use of cardiac CT and cardiac MRI procedures. These more advanced forms of testing can help identify features such as myocardial scarring, which may have contributed to the onset of V-Tach. For patients with cardiac ischemia, a cardiac angiogram can be performed to determine the need for revascularization procedures.[1]
Blood testing for levels of tropinin, potassium, and other lab values associated with cardiac function are also important in the diagnosis and management of V-Tach.[1]
Management / Interventions[edit | edit source]
Management of acute V-Tach is aimed at returning the heart to normal sinus rhythm. If sustained V-Tach results in neamdynamic instability, the first line of treatment is cardioversion. If cardioversion is unsuccessful in preventing recurrent episodes of V-Tach, drugs such as amiodarone can be used to help maintain normal sinus rhythm. Further management is then dictated by underlying causes or cardiac comorbidities. Patients with ischemic heart disease may be immediately referred for assessment for or receiving of revascularization procedures.[1]
A variety of IV medications can also be used in the management of acute V-Tach:[1]
- Antiarrhythmia drugs are used in cases of V-Tach and concurrent structures hearth diseases (i.e. cardiomyopathies or valvular stenosis). I.e. procainamide or amiodarone
- Beta blockers and calcium channel blockers are often used for idiopathic V-Tach. I.e. varapramil
- Beta Blockers for the main drug used for patients with concurrent cardiac ion channel pathologies
Other interventions such as anti-tachycardia pacing or cardiac ablation may be considers in specific cases depending of the severity of the patient's condition and the underlying causes of V-Tach.[1]
Long term management is focused for heavily on the underlying cause or precipitating factors of a patient's V-Tach. Implantable Cardiac Defibrillators (ICD) are often considered in to prevent the occurrence of of sudden cardiac death, however, the the decision to utilize an ICD is often influenced by many factors and may not be appropriate depending on a patient's medical history and prognosis.[1]
Prescription beta blockers and calcium channel blockers are also a common method of long term treatment, especially in those with underlying cardiomyopathies and a variety of other cardiac conditions.[1]
In cases where drug intervention is ineffective at managing V-Tach, catheter ablation can be considered. Several recent studies support the effectiveness of ablation procedures in reducing the occurrence of V-Tach, as well as the need for ICD activation in patients who historically present with this condition.[1]
Differential Diagnosis[edit | edit source]
Providers should procure a through patient history, as well as other diagnostic testing such as ECG to rule out the presence of other arrhythmias such as certain types of supraventricular tachycardia.[1]
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 Foth C, Gangwani MK, Ahmed I, et al. Ventricular Tachycardia [Internet]. StatPearls. Treasure Island (FL): StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532954/
- ↑ 2.0 2.1 2.2 Johns Hopkins Medicine. Ventricular Tachycardia. Available from: https://www.hopkinsmedicine.org/health/conditions-and-diseases/ventricular-tachycardia
- ↑ Kim, J. Channelopathies. Korean journal of pediatrics. 2014; 57(1): 1-18. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3935107/