Zellweger Syndrome
Original Editor - User Name
Top Contributors - Ayodeji Mark-Adewunmi
This article is currently under review and may not be up to date. Please come back soon to see the finished work!
Introduction[edit | edit source]
Zellweger syndrome(Zellweger Spectrum Disorders) is a rare congenital disorder characterized by the reduction or absence of functional peroxisomes in the cells of an individual.[1] It is one of a family of disorders called Zellweger spectrum disorders which are leukodystrophies. Zellweger syndrome is named after Hans Zellweger (1909–1990), a Swiss-American pediatrician, a professor of pediatrics and genetics at the University of Iowa who researched this disorder.
Zellweger spectrum disorder, also known as cerebrohepatorenal syndrome, is a rare inherited disorder characterized by the absence/reduction of functional peroxisomes in cells, which are essential for beta-oxidation of very long-chain fatty acids. It is autosomal recessive in inheritance, and the spectrum of the disease includes Zellweger syndrome (ZS), neonatal adrenoleukodystrophy (NALD), infantile Refsum disease (IRD), and rhizomelic chondrodysplasia punctata type 1 (RCDP1) depending on the phenotype and severity.[2]
Etiology[edit | edit source]
Zellweger syndrome is the result of a mutation in any of the 12 PEX genes. Most cases of Zellweger syndrome are due to a mutation in the PEX1 gene. These genes control peroxisomes, which are needed for normal cell function.
ZSDs are caused by mutations in one of the 13 different PEX genes. PEX genes encode proteins called peroxins and are involved in either peroxisome formation, peroxisomal protein import, or both. As a consequence, mutations in PEX genes cause a deficiency of functional peroxisomes.[3] Cells from ZSD patients either entirely lack functional peroxisomes, or cells can show a reduced number of functional peroxisomes or a mosaic pattern (i.e. a mixed population of cells with functional peroxisomes and cells without. Peroxisomes are involved in many anabolic and catabolic metabolic processes, like biosynthesis of ether phospholipids and bile acids, α- and β-oxidation of fatty acids and the detoxification of glyoxylate and reactive oxygen species. Dysfunctional peroxisomes therefore cause biochemical abnormalities in tissues,[4] but also in readily available materials like plasma and urine.[5]
Epidemiology[edit | edit source]
The incidence of ZSDs is estimated to be 1 in 50.000 newborns in the United States.[6] It is presumed that ZSDs occur worldwide, but the incidence may differ between regions. For example, the incidence of (classic) Zellweger syndrome in the French-Canadian region of Quebec was estimated to be 1 in 12. A much lower incidence is reported in Japan, with an estimated incidence of 1 in 500.000 births [19]. More accurate incidence data about ZSDs will become available in the near future, since newborn screening for X-linked adrenoleukodystrophy
Clinical Features[edit | edit source]
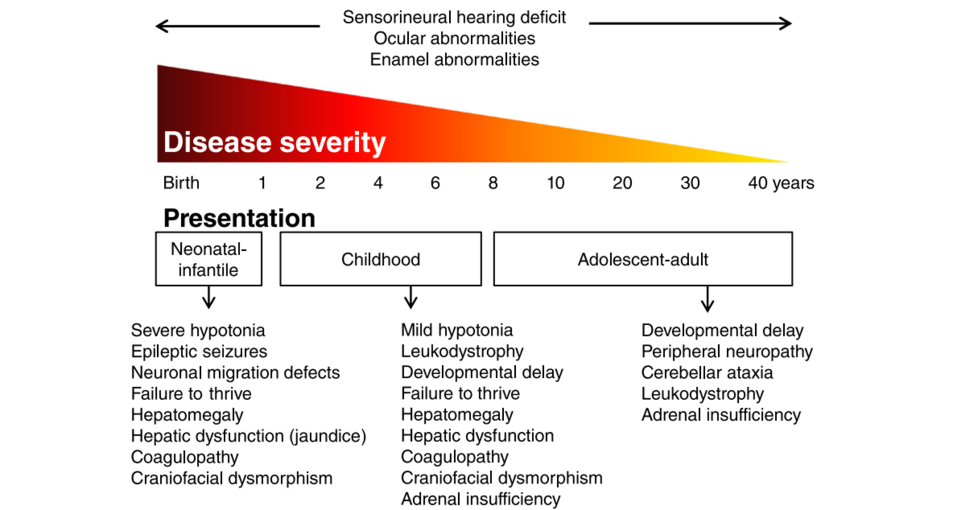
Patients with a ZSD can roughly be divided into three groups according to the age of presentation: the neonatal, infantile presentation, the childhood presentation and an adolescent-adult (late) presentation.
Neonatal-Infantile Presentation[edit | edit source]
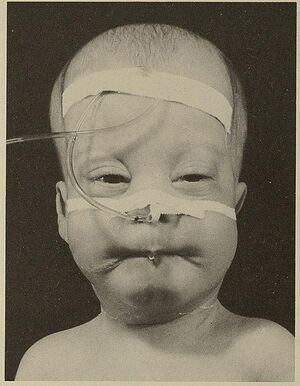
ZSD patients within this group typically present in the neonatal period with hepatic dysfunction and profound hypotonia resulting in prolonged jaundice and feeding difficulties. Epileptic seizures are usually present in these patients. Characteristic dysmorphic features can usually be found, of which the facial dysmorphic signs are most evident. Sensorineural deafness and ocular abnormalities like retinopathy, cataracts and glaucoma are typical but not always recognized at first presentation. Brain magnetic resonance imaging (MRI) may show neocortical dysplasia (especially perisylvian polymicrogyria), generalized decrease in white matter volume, delayed myelination, bilaterial ventricular dilatation and germinolytic cysts.[7] Neonatal onset leukodystrophy is rarely described.[8] Calcific stippling (chondrodysplasia punctata) may be present, especially in the knees and hips. The neonatal-infantile presentation grossly resembles what was originally described as classic ZS. Prognosis is poor and survival is usually not beyond the first year of life.
Childhood Presentation[edit | edit source]
These patients show a more varied symptomatology than ZSD patients with a neonatal-infantile presentation. Presentation usually involves delayed developmental milestone achievement. Ocular abnormalities comprise retinitis pigmentosa, cataract and glaucoma, often leading to early blindness and tunnel vision.[9]
Sensorineural deafness is almost always present and usually discovered by auditory screening programs. Hepatomegaly and hepatic dysfunction with coagulopathy, elevated transaminases and (history of ) hyperbilirubinemia are common. Some patients develop epileptic seizures. Craniofacial dysmorphic features are generally less pronounced than in the neonatal-infantile group.
Renal calcium oxalate stones and adrenal insufficiency may develop. Early-onset progressive leukodystrophy may occur, leading to loss of acquired skills and milestones in some individuals. The progressive demyelination is diffuse and affects the cerebrum, midbrain and cerebellum with involvement of the hilus of the dentate nucleus and the peridentate white matter.[10]
Sequential imaging in three ZSD patients showed that the earliest abnormalities related to demyelination were consistently seen in the hilus of the dentate nucleus and superior cerebellar peduncles, chronologically followed by the cerebellar white matter, brainstem tracts, parieto-occipital white matter, splenium of the corpus callosum and eventually involvement of the whole of the cerebral white matter.[11]
A small subgroup of patients develop a relatively late-onset white matter disease, but no patients with late-onset rapid progressive white matter disease after the age of five have been reported.[12] Prognosis depends on what organ systems are primarily affected (i.e. liver) and the occurrence of progressive cerebral demyelination, but life expectancy is decreased and most patients die before adolescence.
Adolescent-Adult Presentation[edit | edit source]
Symptoms in this group are less severe, and diagnosis can be in late child- or even adulthood.[13] Ocular abnormalities and a sensorineural hearing deficit are the most consistent symptoms. Craniofacial dysmorphic features can be present, but may also be completely absent.
Developmental delay is highly variable and some patients may have normal intelligence. Daily functioning ranges from completely independent to 24 h care. It is important to emphasize that primary adrenal insufficiency is common and is probably under diagnosed. In addition to some degree of developmental delay, other neurological abnormalities are usually also present:
- signs of peripheral neuropathy,
- cerebellar ataxia and
- pyramidal tract signs.
The clinical course is usually slowly progressive, although the disease may remain stable for many years. Slowly progressive, clinically silent leukoencephalopathy is common, but MRI may be normal in other cases.
Pathophysiology[edit | edit source]
Peroxisomes are single membrane-bounded organelles with a matrix containing over 50 enzymes for fatty acid metabolism. All human cells except erythrocytes contain peroxisomes. The liver and kidney have peroxisomes in abundance in comparison to other organs. Peroxins are necessary for the proper assembly of peroxisomes, and mutations in the peroxin gene (PEX) result in a defect in peroxisomal formation, which is associated with lower or undetectable levels of key internal enzymes. The peroxisomes are involved in beta-oxidation of very-long-chain fatty acids (VLCFA), alpha oxidation of branched-chain fatty acids, catabolism of amino acids and ethanol, biosynthesis of bile acids, steroid hormones, gluconeogenesis, and plasmalogen formation which are important constituents of the cell membrane and myelin. It is also involved in the degradation of cytotoxic hydrogen peroxide.[14]
Zellweger spectrum disorder is thus characterized by increased accumulation of VLCFA and increased C26 and C22 fatty acids in plasma, fibroblasts, and amniocytes.[15] Reduced steroid biosynthesis and accumulation of VLCFA in adrenal gland cells cause decreased levels of adrenocorticotropic hormone (ACTH) and some other steroidal hormones.[16] Reduced degradation of cytotoxic hydrogen peroxide and abnormal accumulation of VLCFA causes neuronal membrane injury and demyelination.[17]
Major abnormalities are present in the kidney (cortical cysts), liver (fibrotic), and brain (demyelination, centrosylvian polymicrogyria) - hence the name cerebrohepatorenal syndrome.
References[edit | edit source]
- ↑ Brul S, Westerveld A, Strijland A, Wanders RJ, Schram AW, Heymans HS, Schutgens RB, Van Den Bosch H, Tager JM. Genetic heterogeneity in the cerebrohepatorenal (Zellweger) syndrome and other inherited disorders with a generalized impairment of peroxisomal functions. A study using complementation analysis. The Journal of clinical investigation. 1988 Jun 1;81(6):1710-5.
- ↑ Powers JM, Tummons RC, Caviness Jr VS, Moser AB, Moser HW. Structural and chemical alterations in the cerebral maldevelopment of fetal cerebro-hepato-renal (Zellweger) syndrome. Journal of Neuropathology & Experimental Neurology. 1989 May 1;48(3):270-89.
- ↑ Waterham HR, Ebberink MS. Genetics and molecular basis of human peroxisome biogenesis disorders. Biochimica et Biophysica Acta (BBA)-Molecular Basis of Disease. 2012 Sep 1;1822(9):1430-41.
- ↑ Braverman NE, D'Agostino MD, MacLean GE. Peroxisome biogenesis disorders: Biological, clinical and pathophysiological perspectives. Developmental disabilities research reviews. 2013 Jun;17(3):187-96.
- ↑ Wanders RJ, Waterham HR. Peroxisomal disorders I: biochemistry and genetics of peroxisome biogenesis disorders. Clinical genetics. 2005 Feb;67(2):107-33.
- ↑ Steinberg SJ, Dodt G, Raymond GV, Braverman NE, Moser AB, Moser HW. Peroxisome biogenesis disorders. Biochimica et Biophysica Acta (BBA)-Molecular Cell Research. 2006 Dec 1;1763(12):1733-48.
- ↑ Poll-The BT, Gärtner J. Clinical diagnosis, biochemical findings and MRI spectrum of peroxisomal disorders. Biochimica et Biophysica Acta (BBA)-Molecular Basis of Disease. 2012 Sep 1;1822(9):1421-9.
- ↑ Poll‐The BT, Gootjes J, Duran M, De Klerk JB, Maillette de Buy Wenniger‐Prick LJ, Admiraal RJ, Waterham HR, Wanders RJ, Barth PG. Peroxisome biogenesis disorders with prolonged survival: phenotypic expression in a cohort of 31 patients. American Journal of Medical Genetics Part A. 2004 May 1;126(4):333-8.
- ↑ Hamel C. Retinitis pigmentosa. Orphanet journal of rare diseases. 2006 Dec;1(1):1-2.
- ↑ Poll-The BT, Gärtner J. Clinical diagnosis, biochemical findings and MRI spectrum of peroxisomal disorders. Biochimica et Biophysica Acta (BBA)-Molecular Basis of Disease. 2012 Sep 1;1822(9):1421-9.
- ↑ Van der Knaap MS, Wassmer E, Wolf NI, Ferreira P, Topçu M, Wanders RJ, Waterham HR, Ferdinandusse S. MRI as diagnostic tool in early-onset peroxisomal disorders. Neurology. 2012 Apr 24;78(17):1304-8.
- ↑ Barth PG, Gootjes J, Bode H, Vreken P, Majoie CB, Wanders RJ. Late onset white matter disease in peroxisome biogenesis disorder. Neurology. 2001 Dec 11;57(11):1949-55.
- ↑ Moser AB, Rasmussen M, Naidu S, Watkins PA, McGuinness M, Hajra AK, Chen G, Raymond G, Liu A, Gordon D, Garnaas K. Phenotype of patients with peroxisomal disorders subdivided into sixteen complementation groups. The Journal of pediatrics. 1995 Jul 1;127(1):13-22.
- ↑ Roth KS. Peroxisomal disease-common ground for pediatrician, cell biologist, biochemist, pathologist, and neurologist. Clinical pediatrics. 1999 Mar;38(2):73-5.
- ↑ Moser AB, Kreiter N, Bezman L, Lu SE, Raymond GV, Naidu S, Moser HW. Plasma very long chain fatty acids in 3,000 peroxisome disease patients and 29,000 controls. Annals of Neurology: Official Journal of the American Neurological Association and the Child Neurology Society. 1999 Jan;45(1):100-10.
- ↑ Knazek RA, Rizzo WB, Schulman JD, Dave JR. Membrane microviscosity is increased in the erythrocytes of patients with adrenoleukodystrophy and adrenomyeloneuropathy. The Journal of Clinical Investigation. 1983 Jul 1;72(1):245-8.
- ↑ Powers JM, Moser HW. Peroxisomal disorders: genotype, phenotype, major neuropathologic lesions, and pathogenesis. Brain Pathology. 1998 Jan;8(1):101-20.