Arachnoiditis
Clinically Relevant Anatomy[edit | edit source]
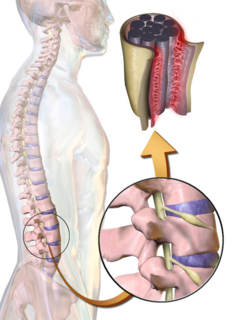
The central nervous system (CNS) which is made up of the brain and the spinal cord is covered and protected by meninges. Meninges are generally three membrane layers, the Dura Mater which is the outer layer, Arachnoid Mater which is the middle layer, and the Pia Mater which is the inner layer. There are 31 pairs of spinal nerves that exit the vertebral column, one on the right side and the other on the left, through vertebral foramina[1].
Pathological Process[edit | edit source]
Arachnoiditis is a progressive disorder that involves the brain and/or the spinal cord caused by inflammation of the arachnoid membrane. There are several types of Arachnoiditis including Adhesive Arachnoiditis which is the most severe type and occurs when spinal nerves stick together, Arachnoiditis ossificans which occurs when arachnoid turns to bone, Cerebral arachnoiditis which affects the membranes surrounding the brain, Hereditary arachnoiditis which is congenital and rare and occurs due to defects affecting the meninges, Neoplastic arachnoiditis which occurs due to cancer and Optochiasmatic arachnoiditis which involves optic nerve[2].
There are 3 main stages of Arachnoiditis.
- The first stage involves the inflammation of the spinal nerves, hyperemia, the disappearance of the subarachnoid space and the scar tissue begins to form.
- The second stage involves the scar tissue formation process increasing and the nerves further adhere to each other and to the dura.
- The third stage involves the complete encapsulation of the nerve roots, compression causes atrophy of the nerve roots and the scarring tissues prevent the production of spinal fluid in that area. In some cases, the scar tissue calcifies and is then termed Arachnoiditis Ossificans[3].
Etiologies[edit | edit source]
- Trauma/Surgery-induced: Arachnoiditis is considered a rare complication of spinal surgery specifically after multiple complex surgeries or trauma to the spine. Multiple lumbar punctures, advanced stages of spinal stenosis and chronic degenerative disc disease may also lead to arachnoiditis. This may result in blood penetration in the subarachnoid space causing inflammation[4].
- Chemical-induced: Myelograms have been considered recently to cause this condition. A myelogram which is a diagnostic test that contains a dye is usually injected in the area surrounding the spinal cord and nerves and is visible on various diagnostic imaging such as X-ray, MRI and CT scan. The repetitive exposure to oil-based radiographic contrast agents used in myelograms causes Arachnoiditis. In addition to that, medications found in epidural steroid injections can cause Arachnoiditis especially if they enter the cerebral spinal fluid (CSF). It's also important to note that, Arachnoiditis due to surgery is precisely localized, meanwhile the one due to epidural injections is more diffuse[5].
- Infection-induced: Arachnoiditis can also be caused by viral or bacterial meningitis, tuberculosis and syphilis affect the spine[6].
Arachnoiditis is also the third most common cause of Failed Back Surgery Syndrome (FBSS)[7].
Clinical Presentation[edit | edit source]
The most prominent symptom of Arachnoiditis would be persistent pain in the lower back and limbs[8]. Other symptoms which are experienced by 90% of patients include:
- tingling sensation and paresthesia
- weakness in the lower limbs
- cramps and spasms
- bladder and sexual dysfunctions[9]
- hyporeflexia
The pain tends to be worse at night and normally evoked by non-painful stimuli or no stimulus at all. This pain also tends to increase with activity where pain tends to be delayed at the onset of activity and persist after the cessation of physical activity[10]. In addition to that, pain can also be caused by other factors besides nerve damage involving the musculoskeletal system due to what this disorder causes from spine dynamic alteration. Patients with this disorder may experience muscle tension, an increase in muscle tone due to nerve damage and severe joint pain[11].
Diagnostic Procedures[edit | edit source]
Arachnoiditis is usually present in the subarachnoid space but can be clearly seen in the lumbar region where we find the cauda equina. There are various radiographic modalities that can help with the diagnostic procedure but an MRI is the most favorable and most sensitive modality[12]. The diagnosis of Arachnoiditis is usually based on 3 main findings which are the inflammation and enlargement of nerve roots on an axial view, their displacement from their normal position, and them appearing clumped together[13]. For patients where an MRI is contraindicated, computed tomography (CT) myelography is an acceptable alternative as a radiographic modality[14]. Other forms of diagnosis would be finding that C-reactive protein (CRP) or Erythrocyte Sedimentation Rate (ESR), inflammatory markers, levels being exceedingly high[15] in addition to other less known inflammatory markers like interleukins and myeloperoxidase having high levels as well. It's important to note that the presence of high levels of ESR and CRP indicate that Arachnoiditis is active and in need of immediate treatment[16].
Management[edit | edit source]
Arachnoiditis is a very difficult condition to treat and the treatment protocols for patients suffering from this condition mainly focus on relieving pain and improving symptoms that affect the patient's daily function.
Medical Management[edit | edit source]
In order to prevent arachnoiditis from progressing and worsening, the medical treatment protocol should focus on controlling and suppressing neuroinflammation. To treat inflammation, the use of non-steroidal anti-inflammatory drugs (NSAIDs) and pulse therapy is common, especially methylprednisolone[17]. However, there are only a few studies demonstrating its effectiveness in preventing scar tissue formation[18]. Other pharmacologic treatments include naltrexone, tricyclic antidepressants and muscle relaxants such as baclofen which are used to release neuropathic pain[19]. Invasive treatment such as intra-spinal narcotic analgesia (INA), epidural steroid and local anesthetic injections are not indicated even though they relieve pain because there is a risk of exacerbating the inflammation and worsening the patient’s condition[2].
Physiotherapy Management[edit | edit source]
Spinal Cord Electrostimulation (SCS) stands for electrical stimulation by implanted electrodes around the spinal cord in the area that is most involved in causing pain. Some studies indicate a 50% success rate when all types of chronic pain are considered[20]. There are several physical therapy modalities that can be used for patients suffering from Arachnoiditis including heat therapy to relieve muscle spasms and LASER therapy which aids in reducing inflammation and breaking adhesions as well as relieving nerve irritation[21]. The treatment of patients diagnosed with Arachnoiditis requires special consideration specifically gentle, individually-prescribed exercises. The main focus should be restoring motion, preserving function and remaining active. It is particularly important that patients improve and maintain the range of motion of their spine and extremities as much as possible to avoid limitation through daily stretching so that eventually the patient can attain full range of motion specifically in their arms and legs and for that reason, patients are advised to walk outside their home daily[22].
Surgical Management[edit | edit source]
The surgical treatment mainly focuses on releasing the cicatricial adhesions and repair the CSF flow. Its effects are short-term relieving the symptoms experienced by patients suffering from this condition and it's often not recommended because it causes more scar tissue and more trauma to the already irritated spinal cord[23].
Differential Diagnosis[edit | edit source]
The clinical diagnosis of Arachnoiditis mainly focuses on the previous medical history of the patient, physical examinations and radiographic testing. There are various syndromes including tumors and infections to the spinal cord, its roots and its plexus that mimic the clinical features of Arachnoiditis. In order to rule out the possibility of other disorders, an MRI of the lumbar spine should be done in addition to screening lab tests to check the complete blood count, Erythrocyte Sedimentation Rate and anti-nuclear antibody testing. These tests should always be performed if the diagnosis of arachnoiditis is in question[6].
References[edit | edit source]
- ↑ Moore KL, Dalley AF, Agur AM. Clinically oriented anatomy. 7th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health; 2014.
- ↑ 2.0 2.1 Peng H, Conermann T. Arachnoiditis. InStatPearls. 2021 Nov 8. StatPearls Publishing.
- ↑ Deshmukh, V.R. Encyclopedia of the Neurological Sciences (Second Edition). Brain and Spine Institute, Portland, OR, USA. 2014.
- ↑ Arachnoiditis: What it is, causes, symptoms & treatment. Cleveland Clinic. Available at: https://my.clevelandclinic.org/health/diseases/12062-arachnoiditis (accessed 17/2/2023)
- ↑ Long DM. Chronic adhesive spinal arachnoiditis: pathogenesis, prognosis, and treatment. Neurosurgery Quarterly. 1992 Dec 1;2(4):296-320.
- ↑ 6.0 6.1 Waldman, S.D. Pain review. Philadelphia, PA: Elsevier.2009.
- ↑ Burgest S. Simopoulos TC. FAILED BACK SURGERY SYNDROME. Current Therapy in Pain. Elsevier. 2009.
- ↑ Tennant F. (228) Which chronic back pain patients have arachnoiditis?. The Journal of Pain. 2016 Apr 1;17(4):S32.
- ↑ MATLOCK, C.L. Physiotherapy and spinal nerve root adhesions: a caution. Physiotherapy research international. Vol: 9(4), p.164-173,2004.
- ↑ Mehta, N. Arachnoiditis. Spine Universe. Available at: https://www.spineuniverse.com/conditions/spinal-disorders/arachnoiditis (accessed 14/2/2023)
- ↑ Smith S. Adhesive Arachnoiditis: A Continuing Challenge. Practical Pain Management. 2004;4(2)
- ↑ Malani AN, Vandenberg DM, Singal B, Kasotakis M, Koch S, Moudgal V, et al. Magnetic resonance imaging screening to identify spinal and paraspinal infections associated with injections of contaminated methylprednisolone acetate. JAMA. Jun 19 2013;309(23):2465-72.
- ↑ Cohen MS, Wall EJ, Kerber CW, Abitbol JJ, Garfin SR. The anatomy of the cauda equina on CT scans and MRI. The Journal of bone and joint surgery. British volume. 1991 May;73(3):381-4.
- ↑ Patel DM, Weinberg BD, Hoch MJ. CT myelography: clinical indications and imaging findings. Radiographics. 2020 Mar;40(2):470-84.
- ↑ Tennant F. Erythrocyte sedimentation rate and C-reactive protein: old but useful biomarkers for pain treatment. Pract Pain Manage. 2013 Mar 1;13(2):61-5.
- ↑ Tennant F. Search for inflammatory markers in centralized, intractable pain. American Academy of Pain Management. 2013.
- ↑ Wright MH, Denney LC. A comprehensive review of spinal arachnoiditis. Orthopaedic Nursing. 2003 May 1;22(3):215-9.
- ↑ Kara T, Davulcu Ö, Ateş F, Arslan FZ, Sara HI, Akin A. What happened to cauda equina fibers? Adhesive arachnoiditis. Anaesthesia, Pain & Intensive Care. 2020 Jun 10;24(5):555-7.
- ↑ Jurga S, Szymańska-Adamcewicz O, Wierzchołowski W, Pilchowska-Ujma E, Urbaniak Ł. Spinal adhesive arachnoiditis: three case reports and review of literature. Acta Neurologica Belgica. 2021 Feb;121:47-53.
- ↑ FREY, M.E., MANCHIKANTI, L., BENYAMIN, R.M., SCHULTZ, D.M.,SMITH, H.S.,COHEN, S.P., ‘Spinal Cord Stimulation for Patients with Failed Back Surgery Syndrome: A Systematic Review’, Pain Physician, vol: 12:379-397, 2009
- ↑ Swain AR. Arachnoiditis: The Evidence Revealed. Anesthesiology. 2012 May;116(5):1167.
- ↑ Lewis C. Physiotherapy and spinal nerve root adhesion: a caution. Physiotherapy Research International. 2004 Nov;9(4):164-73.
- ↑ Morisako H, Takami T, Yamagata T, Chokyu I, Tsuyuguchi N, Ohata K. Focal adhesive arachnoiditis of the spinal cord: imaging diagnosis and surgical resolution. Journal of Craniovertebral Junction and Spine. 2010 Jul;1(2):100.