Erb's Palsy
Original Editor - Rachael Lowe
Top Contributors - Admin, Vidya Acharya, Simisola Ajeyalemi, Kim Jackson, Laura Ritchie, Naomi O'Reilly, Shaimaa Eldib, Rachael Lowe, Wendy Walker, WikiSysop, Claire Knott and Ahmed M Diab
Definition/Description[edit | edit source]
Erb's palsy or Erb–Duchenne palsy is a form of obstetric brachial plexus palsy. It occurs when there's an injury to the brachial plexus, specifically the upper brachial plexus at birth. The injury can either stretch, rupture or avulse the roots of the plexus from the spinal cord[1]. It is the most common birth-related brachial plexus injury (50- 60%).[2]
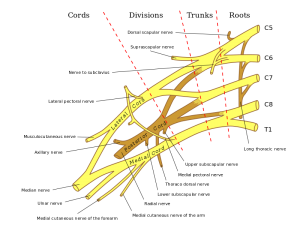
It is a lesion of C5 & C6 nerve roots (in some cases C7 is involved as well) usually produced by widening of the head shoulder interval. Injuries to the brachial plexus affects movement and cutaneous sensations in the upper limb. Depending on the severity of the injury, the paralysis can either resolve on its own over a period of months, require rehabilitative therapy or surgery.[1]
Clinically Relevant Anatomy[edit | edit source]
Neurologically, the Erb's point is a site at the upper trunk of the Brachial Plexus located 2-3cm above the clavicle[3]. It's formed by the union of the C5 and C6 roots which later converge. Affected nerves in Erb's palsy are the axillary nerve, musculocutaneous, & suprascapular nerve.
- Axillary nerve- originates from the terminal branch of posterior cord receiving fibers from C5 and C6. It exits the axillary fossa
posteriorly passing through the quadrangular space with posterior circumflex humeral artery. it fives rise to superior lateral brachial cutaneous nerve then winds around the surgical neck of the humerus deep to deltoid. It innervates the shoulder joint, teres minor and deltoid muscles, skin of superolateral arm. - Musculocutaneous nerve- originates from the terminal branch of lateral cord receiving fibers from C5-C7. It exits the axilla by piercing coracobrachialis, descends between biceps brachii and brachialis while supplying both, continues as lateral cutaneous nerve of forearm. It innervates the muscles of the anterior compartment of the arm and the skin of lateral aspect of the forearm.
- Suprascapular nerve- originates from the superior trunk receiving fibers from C5, C6 often C4. It passes laterally across lateral cervical region superior to brachial plexus then through scapular notch inferior to superior transverse scapular ligament. It innervates the supraspinatus, infraspinatus and shoulder joint.
Epidemiology[edit | edit source]
Frequency
An incidence of 0.8-1 per 1,000 births has been reported for brachial plexus birth palsy (BPBP) in the US.[4] Erb's palsy accounts for about 45% of BPBP.[5] Additional injury to C7 is commonly discovered in 20% of cases of BPBP.[5]
Mortality/Morbidity
Incidence of permanent impairment is 3-25%. The rate of recovery in the first few weeks is a good indicator of final outcome. Complete recovery is unlikely if no improvement has occurred in the first two weeks of life.
Race
A study by Weizsaeker et al 2007 found that being a member of the black population was independently predictive for Erb's palsy.[6]
Mechanism of Injury / Pathological Process[edit | edit source]
The most common cause of Erb's palsy is excessive lateral traction or stretching of the baby's head and neck in opposite directions during delivery usually associated with shoulder dystocia. This may happen during delivery of the head, the head may be deviated away from the axial plane. There can also be compression of the brachial plexus causing it to stretch and tear. Sometimes, pulling on the infant's shoulder during delivery or excessive pressure on the baby's raised arm during a breech delivery can cause brachial plexus injury. Two potential forces act on the brachial plexus during labor- natural expulsive force of the uterus, traction force applied by the obstetrician.[7]
Risk Factors[edit | edit source]
- Shoulder dystocia
- Fetal macrosomia
- Maternal obesity[6]
- Gestational diabetes[6]
- Duration of second stage of labor(over 60 minutes)
- Breech presentation
Clinical Presentation[edit | edit source]
The classical sign of erb's palsy is called Waiter's tip deformity. This is due to loss of the lateral rotators of the shoulder, arm flexors, and hand extensor muscles. The position of the limb, under such conditions, is characterized by : the arm hanging by the side and is rotated medially, the forearm extended and pronated and the wrist flexed. Also, there is loss of sensation in the lateral aspect of the forearm.
The arm cannot be raised from the side; all power of flexion of the elbow is lost, as is also supination of the forearm. Muscles most often affected, by either partial or total paralysis, are supraspinatus and infraspinatus. This occurs because the suprascapular nerve is fixed at the suprascapular notch, with the injury observed at Erb's point (described above). In more severely affected patients deltoid, biceps, brachialis, and subscapular are affected (C5 and C6). Elbow flexion is weakened because of weakness in biceps & brachialis. If roots are damaged above their junction, paralysis of rhomboids and serratus anterior is evident, producing weakness in retraction and protraction of scapula
| [8] | [9] |
Diagnosis[edit | edit source]
A thorough history and physical examination with focus on neurologic examination are used to confirm diagnosis.
History- aims to gather information about pregnancy complicated either by gestational diabetes or maternal obesity, fetal macrosomia, prolonged second stage labour, shoulder dystocia, use of assitive techniques-forceps to aid delivery.
Physical examination- most often shows decreased or absent movement of the affected arm.
Neurologic examination- assesses muscle power, sensation,reflexes- moro reflex is absent on the affected arm.
It might also be important to look for presence of cervical rib. In the report by Becker J, et al (2002), the authors noted that in a series of 42 infants found to have a cervical rib, 28 newborns had an Erb's palsy. They concluded that a cervical rib was a risk factor for an Erb's palsy[10].
Investigations[edit | edit source]
- X-rays of the chest - to rule out clavicular or humeral fracture
- MRI of the shoulder- may demonstrate shoulder dislocation; presence of pseudomeningoceles indicates avulsion injury of the affected spinal roots[11][12][13]
- CT Scan of the shoulder- may demonstrate shoulder dislocation; presence of pseudomeningoceles indicates avulsion injury of the affected spinal roots[11][12][13]
- EMG/Nerve conduction studies- presence of fibrillation potentials indicate denervation
Outcome Measures[edit | edit source]
- Toronto test score
- Active movement scale
- Mallet scale
- Toddler Arm Use Test
Management / Interventions[edit | edit source]
Some brachial plexus injuries may heal without treatment. Many children who are injured during birth improve or recover by 3 to 4 months of age, although it may take up to two years to recover. Fortunately, between 80% to 90% of children with such injuries will attain normal or near normal function[14]. Treatment for brachial plexus injuries includes physiotherapy and, in some cases, surgery.
Physiotherapy Management[edit | edit source]
During the first 6 months treatment is directed specifically at prevention of fixed deformities. Exercise therapy should be administered daily to maintain ROM and improve muscle strength. Parents must be taught to take an active role in maintaining ROM and keeping the functioning muscles fit. Exercises should include bimanual or bilateral motor planning activities.
Initial treatment in the first 1-2 weeks after birth will consist of[15][16][17]:
- Careful handling is required and extremes of motion are to be avoided for the first 1 to 2 weeks to allow for the initial inflammatory response to the injury to calm.
- Avoid picking a child up by the arm. or from under the armpit. This can compress or stretch the brachial plexus and cause further injury
- Placing a child on their back or in side-lying, with affected limb up, to avoid compression of the injured limb
- Place the affected arm into sleeves before the unaffected arm. This will help avoid extreme movement at the shoulder and will help make dressing quicker and easier.
A systematic review suggests physiotherapy interventions like constraint-induced movement therapy, kinesiotape, electrotherapy, virtual reality and use of splints or orthotics have positive outcomes for the affected upper limb functionality in obstetric brachial palsy from 0 to 10 years.[18]
- Activities and exercises to promote recovery of movement and muscle strength
- Exercises to maintain range of movement in the joints to prevent stiffness and pain
- Sensory stimulation to promote increased awareness of the arm
- Provision of splints to prevent secondary complications and maximise function
- Educating parents on appropriate handling and positioning of the child and home exercises to maximise the child’s potential for recovery
- Constraint induced movement therapy may be useful[19]
- Electrical Stimulation may be beneficial[20]
- Referral to Occupational Therapy for assessment of function in day to day activities.
Home exercises:
Encourage parents to carry out specific exercises with their child 2-3 a day in the comfort of their own home - although the exercises can be carried out anywhere appropriate and comfortable. The Home Exercise Programme may focus on the following[15][16][17]:
- Maintain movement at the joints – Ensuring that the joints of the affected limb, especially the shoulder, keep their full range of movement and avoid excessive shortening of the muscles, also called a contracture. This will include passive, assisted and active exercises.
- Increasing the strength of muscles in the affected limb.
- Increasing the child’s awareness of the arm through tactile touch and contact.
- Teaching parents, carers and the child how to handle the affected limb and how to position it for both comforts, prevention of complications and practicality.
- The use of Constraint-Induced Movement Therapy (CIMT) and bimanual/bilateral therapy are sometimes also considered by Physiotherapists.
| [21] | [22] |
Surgical Management [edit | edit source]
Surgical intervention is a possible treatment option and will be considered by the medical team after appropriate assessment[23][24]. Surgery is only considered when conservative treatment (such as physiotherapy) is deemed unsuitable[25]. This may be just after birth, as the severity of the BPBP injury requires surgical intervention, or it may be later in a child’s development. Surgery for BPBP can involve nerve transplants or tendon transfer of functioning muscles[26][27]. Many children show a complete recovery, but for those unfortunate not to recover fully, it is important to focus on helping a child to adapt to tasks and work on different strategies to complete activities in their daily life.
Living with BPBP[edit | edit source]
Dina Shafer, who also has a lasting disability affecting her right arm due to BPBP, has a Youtube channel showing how she carries out her activities of daily living such as driving her car and curling her hair as well as how she exercises at the gym where her workouts involve a range of different exercises from deadlifts to martial arts training.
A number of individuals diagnosed with BPBP went on to have successful careers in their chosen field, Martin Sheen was diagnosed with BPBP as was Adrain Clayborn, an American Football player who was drafted 20th overall in the 2011 Draft by the Tampa Bay Buccaneers.
There are also other inspiring individuals out there, including Emily Langridge, a young woman with BPBP who created a documentary following families, adults and children with the condition. Watch the film on the website of the Brachial Plexus Palsy Project.
Intervention Management[edit | edit source]
Indications for surgery is no clinical or EMG evidence of biceps function by 6 months. This represents 10% to 20% of children with obstetric palsies.
The three most common treatments for Erb's Palsy are: Nerve transplants (usually from the opposite leg), Sub Scapularis releases and Latissimus Dorsi Tendon Transfers.
Nerve transplants are usually performed on babies under the age of 9 months since the fast development of younger babies increases the effectiveness of the procedure. They are not usually carried out on patients older than this because when the procedure is done on older infants, more harm than good is done and can result in nerve damage in the area where the nerves were taken from. Scarring can vary from faint scars along the lines of the neck to full "T" shapes across the whole shoulder depending on the training of the surgeon and the nature of the transplant.
Subscapularis releases, however, are not time limited. Since it is merely cutting a "Z" shape into the subscapularis muscle to provide stretch within the arm, it can be carried out at almost any age and can be carried out repeatedly on the same arm; however, this will compromise the integrity of the muscle.
Latissimus Dorsi Tendon Transfers involve cutting the Latissimus Dorsi in half horizontally in order to 'pull' part of the muscle around and attach it to the outside of the biceps. This procedure provides external rotation with varying degrees of success. A side effect may be increased sensitivity of the part of the biceps where the muscle will now lie, since the Latissimus Dorsi has roughly twice the number of nerve endings per square inch of other muscles.
Prognosis[edit | edit source]
The prognosis is dependent on the severity of injury, timing of treatment- the earlier, the better the results and associated injuries (fractures of shoulder/arm). Mild cases of erb's palsy may resolve in three to six months with physical therapy. Erb's palsy resolves completely in the first year of life in approximately 70%- 80% of patients and nearly 100% if treatment begins in the first four weeks of birth.[28] Also, effective hand grasp during treatment is associated with good prognosis.
Differential Diagnosis[edit | edit source]
- Clavicular fracture[29]
- Osteomyelitis of the humerus or clavicle
- Septic arthritis of the shoulder[30][31]
References[edit | edit source]
- ↑ 1.0 1.1 Erb-Duchenne and Dejerine-Klumpke Palsies Information Page: National Institute of Neurological Disorders and Stroke(NINDS)
- ↑ Raducha JE, Cohen B, Blood T, Katarincic J. A review of brachial plexus birth palsy: Injury and rehabilitation. Rhode Island Medical Journal. 2017 Nov 1;100(11):17-21.
- ↑ Landers JT, Maino K. Clarifying Erb's point as an anatomic landmark in the posterior cervical triangle. Dermatologic surgery. 2012 Jun 1;38(6):954-7.
- ↑ Gilbert WM, Nesbitt TS, Danielsen B. Associated factors in 1611 cases of brachial plexus injurt. Obstet Gynecol.1999 Apr. 93(4): 536-40.
- ↑ 5.0 5.1 Smith NC, Rowan P, Benson LJ, et al. Neonatal brachial plexus palsy: outcome of absent biceps function at three months of age. J Bone Joint Surg Am. 2004;86-A:2163-2170.
- ↑ 6.0 6.1 6.2 Weizsaeker K, Deaver JE, Cohen WR; Labour characteristics and neonatal Erb's palsy.BJOG.2007 Aug 114(8):1003-9. Epub 2007 Jun 12.
- ↑ Doumouchtsis SK, Arulkumaran S. Are all brachial plexus injuries caused by shoulder dystocia?. Obstetrical & gynecological survey. 2009 Sep 1;64(9):615-23. [1]
- ↑ Emsmiles14.Part 1 - A Journey Through Erb's Palsy - A Documentary on Obstetrical Brachial Plexus Nerve Damage. Available from: http://www.youtube.com/watch?v=xzRhIyw85Xk [last accessed 26/03/14]
- ↑ Emsmiles14. Part 2 - A Journey Through Erb's Palsy - A Documentary on Obstetrical Brachial Plexus Nerve Damage. Available from: http://www.youtube.com/watch?v=zlGSlMXFSFk [last accessed 26/03/14]
- ↑ Becker MH, Lassner F, Bahm J, Ingianni G, Pallua N.. The cervical rib. A predisposing factor for obstetric brachial plexus lesions. J Bone Joint Surg Br. 2002 Jul;84(5):740-3.
- ↑ 11.0 11.1 Medina LS, Yaylali I, Zurakowski D, et al. Diagnostic performance of MRI and MR myelography in infants with a brachial plexus injury. Pediat Radiol. 2006;36:1295-1299.
- ↑ 12.0 12.1 Smith AB, Gupta N, Strober J, et al Magnetiic resonance neurography in children with birth-related brachial plexus injury. Pediatr Radiol. 2008;38:159-163.
- ↑ 13.0 13.1 Tse R, Nixon JN, Iyer RS, et al.The diagnostic value of CT myelography MR myelography and both in neonatal brachial plexus palsy. AJNR Am J Neuroradiol. 2014;35:1425-1432.
- ↑ Wheeless' Textbook of Orthopaedics. Erb's Palsy. http://www.wheelessonline.com/ortho/erbs_palsy
- ↑ 15.0 15.1 Clarke HM, Curtis CG. An approach to obstetrical brachial plexus injuries. Hand clinics. 1995 Nov;11(4):563-80.
- ↑ 16.0 16.1 Shenaq SM, Bullocks JM, Dhillon G, Lee RT, Laurent JP. Management of infant brachial plexus injuries. Clinics in plastic surgery. 2005 Jan 1;32(1):79-98.
- ↑ 17.0 17.1 Waters PM. Update on management of pediatric brachial plexus palsy. Journal of Pediatric Orthopaedics. 2005 Jan 1;25(1):116-26.
- ↑ Palomo R, Sánchez R. Physiotherapy applied to the upper extremity in 0 to 10-year-old children with obstetric brachial palsy: a systematic review. Revista de Neurologia. 2020 Jul 1;71(1):1-0.
- ↑ Vaz DV, Mancini MC, do Amaral MF, de Brito Brandão M, de França Drummond A, da Fonseca ST. Clinical changes during an intervention based on constraint-induced movement therapy principles on use of the affected arm of a child with obstetric brachial plexus injury: a case report. Occup Ther Int. 2010 Dec;17(4):159-67.
- ↑ Okafor UA, Akinbo SR, Sokunbi OG, Okanlawon AO, Noronha CC. Comparison of electrical stimulation and conventional physiotherapy in functional rehabilitation in Erb's palsy. Nigerian quarterly journal of hospital medicine. 2008;18(4):202-5.
- ↑ Erb's Palsy with LOVE. Erb's Palsy 3 weeks old Physical Therapy Routine. Available from: http://www.youtube.com/watch?v=V3KxSsZp_6c [last accessed 26/03/14]
- ↑ LurieChildrens. Brachial Plexus Palsy: Occupational Therapy Demonstrations. Available from: http://www.youtube.com/watch?v=U7umR9sPUqs [last accessed 26/03/14]
- ↑ Hale HB, Bae DS, Waters PM. Current concepts in the management of brachial plexus birth palsy. The Journal of hand surgery. 2010 Feb 1;35(2):322-31.
- ↑ Yang LJ. Neonatal brachial plexus palsy—management and prognostic factors. InSeminars in perinatology 2014 Jun 1 (Vol. 38, No. 4, pp. 222-234). WB Saunders.
- ↑ Zafeiriou DI, Psychogiou K. Obstetrical brachial plexus palsy. Pediatric neurology. 2008 Apr 1;38(4):235-42.
- ↑ Hale HB, Bae DS, Waters PM. Current concepts in the management of brachial plexus birth palsy. The Journal of hand surgery. 2010 Feb 1;35(2):322-31.
- ↑ Birch, R. 2011. Birth lesions of the brachial plexus. In:ed. Surgical disorders of the peripheral nerves, Springer, 429-481
- ↑ Volpe JJ. Neurology of the newborn 3rd Edn. Philadelphia, Pennsylvania: WB Saunders; 1995. pp 781-4
- ↑ Peleg D, Hasnin J, Shalev E. Fractured clavicle and Erb's palsy unrelated to birth trauma. American journal of obstetrics and gynecology. 1997 Nov 1;177(5):1038-40.
- ↑ Gabriel SR, ThometzJG, Jaradeh S. Septic arthritis associated with brachial plexus neuropathy. A case report. J Bone Joint Surg Am.1996;78:103-5.
- ↑ Sharma RR, Sethu AU, Mahapatra AK, Pawar SJ, Nath A. Neonatal cervical osteomyelitis with paraspinal abscess and Erb's palsy. A case report and brief review of the literature. Pediatr Neurosurg.2000;32:230-3.