Forgotten Joint Score-12
Introduction[edit | edit source]
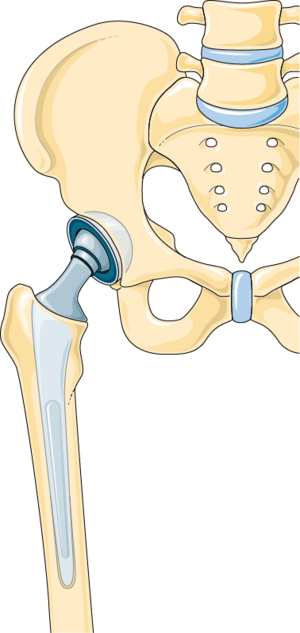
The Forgotten Joint Score-12 (FJS-12) is a patient-reported outcome measure specifically designed to assess the extent to which patients are unaware of their artificial joints in everyday life. It is beneficial for evaluating outcomes after joint replacement surgeries, such as total hip arthroplasty (THA) and total knee arthroplasty (TKA).
Objective[edit | edit source]
The primary objective of the FJS-12 is to evaluate the extent to which patients "forget" their artificial joints during daily activities. A higher score indicates that the patient is less aware of their joint, suggesting better surgical outcomes and higher levels of patient satisfaction[1].
Intended Population[edit | edit source]
The FJS-12 is intended for patients who have undergone joint replacement surgeries, including:
- Total Hip Arthroplasty (THA)
- Total Knee Arthroplasty (TKA)
It is especially useful for patients in the postoperative phase to assess the long-term success of the surgery and the functional integration of the prosthetic joint into their daily lives[2].
Significance of Joint Awareness[edit | edit source]
Joint replacement surgeries, such as total hip arthroplasty (THA) and total knee arthroplasty (TKA), aim to restore function, alleviate pain, and improve the quality of life for patients suffering from severe joint conditions.
Traditional outcome measures have focused on pain relief, range of motion, and functional capabilities. However, these measures do not fully capture the patient's subjective experience and overall satisfaction with the surgery.
This is where the concept of joint awareness, as measured by the Forgotten Joint Score-12 (FJS-12), becomes critically important.
- Psychological and Emotional Well-being[2]
- High joint awareness can lead to frustration, anxiety, and dissatisfaction.
- "Forgetting" the joint indicates seamless integration, contributing to mental comfort and life satisfaction.
- Indicator of Surgical Success[3]
- Complements traditional measures of pain relief and functional improvement.
- High FJS-12 scores indicate successful surgery and effective rehabilitation.
- Quality of Life and Daily Functioning[1]
- High joint awareness can limit social, recreational, or occupational activities.
- Higher FJS-12 scores suggest improved quality of life and unrestricted daily functioning.
- Enhanced Patient-Clinician Communication[4]
- Provides a clear measure of joint awareness for better patient-clinician communication.
- Helps tailor postoperative care and rehabilitation to improve outcomes and satisfaction.
- Long-Term Satisfaction and Prosthesis Longevity[2]
- Associated with long-term satisfaction and reduced need for revision surgeries.
- Encourages better adherence to follow-up care and prosthesis maintenance.
Advantages[edit | edit source]
- Focuses on the patient's subjective experience of their joint.
- More sensitive to high-level outcomes compared to traditional measures.
- Simple and quick to administer and score.
Limitations[edit | edit source]
- May not be suitable for patients with severe functional impairments where joint awareness is consistently high.
- May require adaptation for different languages and cultural contexts to maintain validity.
Method of Use[edit | edit source]
Administration
The FJS-12 is a self-administered questionnaire consisting of 12 items. Patients rate their awareness of the joint during various activities on a five-point Likert scale:
- Never
- Almost Never
- Seldom
- Sometimes
- Mostly
Scoring[edit | edit source]
Scores for each item are summed and then transformed to a 0-100 scale, with higher scores indicating better outcomes (less awareness of the joint).
Reliability[edit | edit source]
The FJS-12 has demonstrated high reliability, with a Cronbach's alpha greater than 0.9, indicating excellent internal consistency. Test-retest reliability studies have also shown consistent results over time, making it a dependable measure for repeated assessments[5]
Validity[edit | edit source]
The FJS-12 has strong construct validity, correlating well with other established measures such as the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and the Oxford Hip and Knee Scores. It effectively differentiates between patients with varying levels of joint awareness and function[3] .
Responsiveness[edit | edit source]
The FJS-12 is highly responsive to clinical changes, making it suitable for detecting improvements or deteriorations in joint awareness post-surgery. It is sensitive to differences in surgical techniques and rehabilitation protocols, capturing subtle changes in patient outcomes[5] .
References[edit | edit source]
- ↑ 1.0 1.1 Behrend H, Giesinger K, Giesinger JM, Kuster MS. The "forgotten joint" as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J Arthroplasty. 2012;27(3):430-6
- ↑ 2.0 2.1 2.2 Hamilton DF, Loth FL, MacDonald DJ, Patton JT, Simpson AHRW, Howie CR, et al. Validation of the English language Forgotten Joint Score-12 as an outcome measure for total hip and knee arthroplasty in a British population. Bone Joint J. 2017;99-B(2):218-24.
- ↑ 3.0 3.1 Thienpont E, Schwab PE, Fennema P. Efficacy of total knee arthroplasty for osteoarthritis in patients aged 80 years or older: a systematic review and meta-analysis. Bone Joint J. 2014;96-B(10):1257-63.
- ↑ Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: Patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. 2005;452:35-43.
- ↑ 5.0 5.1 Hossain FS, Konan S, Patel S, Rodriguez-Merchan EC, Haddad FS. The assessment of outcome after total knee arthroplasty: are we there yet? Bone Joint J. 2017;97-B(1):3-9.