Introduction to Gait Rehabilitation in Spinal Cord Injury
Original Editor -Ewa Jaraczewska based on the course by Maha Tayseer Mohammad
Top Contributors - Ewa Jaraczewska, Jess Bell and Kim Jackson
Introduction[edit | edit source]
Regaining walking function is a goal for many individuals with spinal cord injury, and it is a target of various rehabilitative approaches. It is, however, essential to understand the "natural course of walking recovery"[1] in individuals with spinal cord injury (SCI), as well as prognostic factors that influence walking recovery when establishing goals and selecting interventions.[1] This article discusses two approaches to gait rehabilitation, the plasticity approach and the compensatory approach. It also explores factors that help predict ambulation recovery for patients with a spinal cord injury.
Plasticity-Based Approach[edit | edit source]
The plasticity-based approach to gait rehabilitation in spinal cord injury arises from activity-dependent neural adaptation and training research. Afferent input influences the activity-dependent plasticity of the spinal cord, which affects the neurobiological control of walking.[2]
Early research:
- Sherrington[3] proposed that "proprioceptors responding to hip extension are important for initiating swing"[4]
- Grillner and Rossignol[5] found that preventing hip extension in chronic spinal cats "inhibited the generation of the flexor burst and thus the onset of the swing phase"[4]
- Hiebert et al.[6] found that vibration of iliopsoas during stance resulted in an "earlier onset of swing in walking decerebrate cats"[4]
As a result of these studies, rehabilitation strategies to achieve ambulation in individuals with a spinal cord injury focused on hip extension, load and other sensory elements to facilitate walking.
In the plasticity-based approach, a patient intensively practices a specific task, like locomotion, in a specific training environment while an appropriate sensory input is provided.
The training environment for individuals with spinal cord injury may include a treadmill with body-weight support (BWS), a lokomat, or an Exoskeleton. Sensory input can be provided through limb loading and unloading, trunk posture, hip extension, or limb kinematics.
Example: Locomotor training (Lokomat or treadmill with a body-weight support system):[7]
- the goal of training is to generate stepping in response to specific afferent input associated with the task of walking
- general guidelines focus on maximising loading of the lower limbs through body-weight support systems or overground walking with assistive devices
Compensatory Approach[edit | edit source]
Compensation is "a rehabilitation strategy for non-remediable deficits of strength (force-generating capacity), voluntary motor control, sensation, and balance."[4]
The compensatory approach is based on the principle that patients learn to compensate - i.e. they use their remaining abilities to complete a task, or the task or environment is modified to achieve the established goal.[4] In this approach, walking is accomplished using orthoses and assistive devices, and the outcome depends on the degree of motor and sensory loss.
Definitions of Walking Recovery in Spinal Cord Injury[edit | edit source]
General Definitions[edit | edit source]
Functional ambulation is “the ability to walk, with or without the aid of appropriate assistive devices (such as prostheses, orthoses, canes or walkers), safely and sufficiently to carry out mobility-related activities of daily living.”[8]
Ambulatory capacity is "the highest level of walking function achieved within a standardised environment."[9]
Community ambulation is “independent mobility outside the home, which includes the ability to confidently negotiate uneven terrain, private venues, shopping centres, and other public venues.”[10]
Dimensions of community ambulation:
- Ability to manage distances
- Temporal characteristics
- gait velocity, cadence, step length, and step time
- Speed
- Ambient conditions
- lighting, air temperature and weather conditions
- Terrain
- Promkeaw et al.[12] found that the temporal spatial characteristics of ambulatory patients with spinal cord injury are affected by the surfaces they walk on
- compared to a hard surface, the average stride length, cadence, and walking speed of individuals with spinal cord injury are decreased when walking on artificial grass, soft, and pebble surfaces[12]
- Physical load
- poor road conditions, side-walks with cracks, pot-holes, etc can affect ambulation in individuals with spinal cord injury
- Attentional demands
- gait changes in response to obstacles
- Postural transitions
- ability to maintain dynamic balance affects ambulation
- Density
- the number of people and objects in the immediate surroundings affects ambulation
Definitions of Ambulation in Spinal Cord Injury Research[edit | edit source]
There is no consistent definition of walking recovery after spinal cord injury. The following definitions have been used in publications that discuss predictors for the functional outcome of walking.
Walking recovery is defined as regaining the "ability to walk independently in the community, with or without the use of devices and braces."[1]
Functional ambulation is defined as:
- "The capacity to walk reasonable distances in and out of home unassisted by another person"[13]
- "Independent mobility outside the home to access goods and services in the community”[14]
Van Hedel found that gait speeds can help to distinguish between different levels of ambulation:[15]
- To be considered a "supervised walker" or better, an individual with spinal cord injury must have a mean minimal walking speed of 0.09 ± 0.01 m/s
- To be considered at least an "indoor walker" (i.e. walks indoors with a walking aid but uses a wheelchair outdoors), a minimal walking speed of 0.15 ± 0.08 m/s is required
- To be considered at least an "assisted walker" (i.e. uses a walking aid outdoors), a minimal walking speed of 0.44 ± 0.14 m/s is required
- To be considered a "walker who does not use a walking aid", a minimal walking speed of 0.70 ± 0.13 m/s is required
Outdoor walking is "the self-reported ability to walk more than 100 m outside using one cane, leg orthosis only, or no assistive devices."[16]
Managing curbs is considered a critical task for independent community ambulation.
Predictors for Walking[edit | edit source]
Motor and Sensory Loss[edit | edit source]
- Moon et al.[17] have found that the strength of the hip flexors, followed by the knee extensors, are the most important contributors to regaining independent walking in patients with incomplete spinal cord injury
- Van Middendorp et al.[18] developed a clinical prediction rule (CPR) for ambulation outcomes after traumatic spinal cord injury. A combination of age, motor scores for L3 (quadriceps femoris) and S1 (gastrocsoleus), and light touch sensation of L3 and S1 had "excellent discrimination in distinguishing independent walkers from dependent walkers and non-walkers"[18]
- Draganich et al.[16] validated a CPR for predicting outdoor walking one year after spinal cord injury. In this CPR, L3 motor score (quadriceps), L5 motor score (big toe extensors), and S1 sensory score (light touch) were used as predictor variables[16]
- According to Cathomen et al.,[19] the motor score of the L2 and L3 myotomes allow us to differentiate between walkers and non-walkers. The motor score of the L4-S1 myotomes is considered a prognostic factor for indoor versus outdoor walkers (with and without aids).
Level of Injury and Severity of the Spinal Cord Lesion[edit | edit source]
The International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) is performed 72 hours after a spinal cord injury. The ISNCSCI allows clinicians to determine the neurological level of injury and the severity of the lesion. The ASIA Impairment Scale (AIS) defines complete and incomplete spinal cord lesions.
Severity of the Spinal Cord Lesion[edit | edit source]
- AIS A:[1]
- very limited possibility of achieving functional walking
- 14% of patients who convert from complete to incomplete injury recover some walking function
- patients with an AIS A spinal cord injury at the thoracic or lumbar levels (T12-L3) who regain some walking abilities will need the support of braces (orthoses) and devices to walk
- gait is characterised by slow average velocities and great energy expenditure, which may not be functional for the patient
- AIS B:[1]
- about 33% of patients will recover the ability to ambulate
- pinprick preservation is a positive factor in walking recovery compared to the preservation of light touch only (the preservation of pinprick sensation and light touch suggests there has been less extensive damage to the spinothalamic tracts and posterior column)
- AIS C:[1]
- around 75% of patients have a positive prognosis for walking recovery (this includes patients who convert to AIS D and those who remain AIS C but who achieve some walking function)
- walking recovery is more likely in patients with low thoracic or lumbar lesions
- will need braces and devices to ambulate
- age is a strong prognostic factor
- 80-90% of patients younger than 50 years can walk functionally
- 30-40% of older patients can achieve the same
- AIS D:[1]
- very good ambulation prognosis at one year post-injury
- regardless of age, most patients will likely be able to walk upon discharge from the rehabilitation facility
Level of Injury[edit | edit source]
Patients with the following levels of spinal cord injury may or may not recover their walking ability:[20]
- T11-T12 levels
- may be able to ambulate at home with lower extremity orthoses and a walker
- L1-L2 levels
- may be able to ambulate with knee-ankle-foot orthoses (KAFOs) for short distances, but need a wheelchair for long distances
- L3-L4 levels
- may be able to ambulate socially with elbow crutches and ankle-foot orthoses (AFO)
- L5 and lower
- may be independent in all activities
Range of Motion of the Lower Extremities[edit | edit source]
Spasticity or contracture can impact whether an individual with spinal cord injury can achieve adequate joint range of motion for walking recovery:
- full knee extension range is needed to use a KAFO for ambulation[21]
- adequate ankle dorsiflexion is necessary for foot clearance[22]
- to achieve standing when the hip extensors are absent, an individual with a spinal cord injury needs full hip extension range to lean backwards and move the centre of gravity of their trunk posterior to the hip joint[23]
- individuals with spinal cord injury need 110 degrees of hip flexion to transition from sitting to standing with locked KAFOs[23]
Cardiovascular Endurance[edit | edit source]
"Walking requires increased energy demands on the body and the cardiovascular system, and walking with assistive devices will pose further increased demands."[21] -- Dr. Maha Tayseer Mohammad
- Individuals with spinal cord injury using a swing-through crutch-assisted gait with bilateral KAFOs had an average oxygen consumption rate of 43% more than wheelchair users and 38% more than individuals without spinal cord injuries walking[24]
- Individuals with paraplegia (with hip flexors and knee extensors intact) using a reciprocal crutch-assisted gait without AFOs had an average oxygen consumption rate of 20% more than wheelchair users and 15% more than individuals without spinal cord injuries walking[24]
Age[edit | edit source]
Age is an important factor in predicting ambulation outcomes following spinal cord injury:[25]
- older individuals with a spinal cord injury have worse functional outcomes than younger individuals
- it is more difficult to predict walking abilities for older individuals with spinal cord injury as the outcomes are more variable
Assistive Devices[edit | edit source]
The primary goals of gait rehabilitation of individuals with spinal cord injury are to increase independence and to improve health status. Prolonged wheelchair use has disadvantages, including:[26]
- restriction to mobility due to physical / built barriers in the environment
- decubitus ulcers
- osteoporosis
- joint deformities, including hip joint adduction contracture
However, the use of orthoses for ambulation in spinal cord injury also has challenges, such as:[26]
- significant time spent donning and doffing orthoses
- a high percentage of the force can be applied to the upper limbs depending on the walking style (e.g. up to 55% of body weight can be applied to an elbow crutch during walking, leading to shoulder pain)
- high energy demand during ambulation with orthoses and slow walking speed
Orthoses[edit | edit source]
"The performance of SCI patients and the efficiency of treatment approaches should be evaluated about all aspects of functions, such as activities of daily living and participation."[27]
The evaluation for orthoses for individuals with spinal cord injury should be completed by a multidisciplinary team and must include the patient in the decision-making process. It should: [28]
- establish the goal of the orthosis and rehabilitation
- clarify the limitations of the orthosis
The patient must receive early education on orthosis use, and a follow-up must be scheduled to ensure the patient's safety.
The most commonly used orthoses in gait rehabilitation in spinal cord injury are:
- hip-knee-ankle-foot orthosis (HKAFO)
- knee-ankle-foot orthosis (KAFO)
- ankle-foot orthosis (AFO)
Hip-Knee-Ankle-Foot Orthosis (HKAFO)[edit | edit source]
HKAFOs are a static device that can be made with with hybrid metal and plastic. They have drop lock knee joints and a plastic AFO positioned in neutral.[28] When made of plastic, HKAFOs can be designed to enable some reciprocal gait.[29]
Example of patient who may benefit from an HKAFO: an individual with a T12, AIS A spinal cord injury who presents with the following:
- bilateral lower extremity paralysis
- good trunk and arm control
- absent sensation
- mild lower extremities oedema
- 1+ increased tone based on the Modified Ashworth Scale
The following optional video shows a person with a spinal cord injury mobilising with a HKAFO.
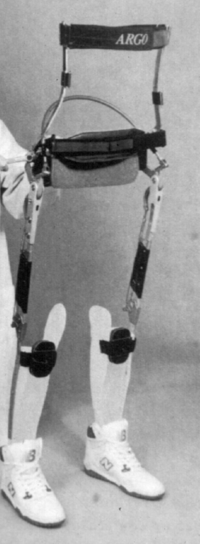
Reciprocating gait orthosis[edit | edit source]
A reciprocating gait orthosis (RGO) is a type of HKAFO that enables a reciprocating gait pattern. With an RGO, one leg can pass in front of the other, creating a more typical pelvic rotation. It controls hip extension and assists with reciprocal hip flexion during the swing phase of gait. The lower limbs and the trunk are stabilised in sagittal and frontal planes. A reciprocal gait is possible due to a double or a single cable built between hip joints.
Advantages of using RGOs:[31]
- psychological benefit of assuming the upright position and talking to others at the same level
- possibility to achieve a functional level of home ambulation with limitations
Disadvantages of using RGOs:[31]
- high cost of the orthosis
- discomfort while wearing the orthosis
- poor fitting
- difficulties with donning and doffing the orthosis
- slow walking speed when compared to using a wheelchair
- individuals wearing an RGO have difficulty getting in and out of cars, walking outside, and climbing stairs
Example of patient who may benefit from an RGO: an individual with an AIS A T1 spinal cord injury who presents with:
- no severe lower limb spasticity
- no lower limb oedema
- between 25 and 50 years old
The following optional video shows an individual mobilising with an RGO and elbow crutches.
Knee-Ankle-Foot Orthosis (KAFO)[edit | edit source]
KAFOs can be metal, plastic or carbon, or they can be hybrid and have the following knee joint options:
- free knee
- drop lock
- bail lock
- trigger lock
- ratchet lock
- offset
- trick knee
The most common design for a KAFO in spinal cord injury gait rehabilitation is plastic with a drop lock.
There is a new generation of stance controlled KAFOs. This type of orthosis locks the knee joint automatically in stance but allows flexion during swing. The option video below demonstrates gait training with bilateral stance controlled KAFOs.
Please watch this video if you would like to see a patient with a T12 spinal cord injury demonstrating walking with crutches and negotiating stairs with one crutch and one rail while wearing a KAFO.
However, patients with a spinal cord injury who require bilateral KAFOs and elbow crutches for swing-through gait tend to prefer to primarily use a wheelchair for mobility.[24] They often discontinue gait training due to:[24][26]
- high energy demands during ambulation
- slow walking speed when compared with wheelchair propulsion or normal walking[24]
Ankle-Foot Orthosis (AFO)[edit | edit source]
AFOs can be made of metal, plastic or carbon, or they can be hybrid. They have anterior trim lines, mid-mall trim lines or posterior leaf springs. Plastic AFOs with posterior leaf springs (PLS) are the most commonly used AFO in gait rehabilitation for individuals with lower lumbar spinal cord injuries. Individuals with thoracic or lumbar incomplete spinal cord injury may require AFOs with an anterior shell or anterior trim lines. You can read more about different types of AFOs here.
Example of patient who may benefit from bilateral posterior leaf AFOs: individual with an L4-5 spinal cord injury, AIS C who presents with:
- flaccid footdrop
- mild sensory loss at the dorsum of the foot
- no oedema
The optional video below shows a patient with an incomplete T7 spinal cord injury ambulating with bilateral AFOs with anterior shells:
Ambulatory Devices[edit | edit source]
The two most common ambulatory devices used by individuals with a spinal cord injury are walkers and crutches.
Walkers[edit | edit source]
A walker is a walking aid that provides a wide base of support. It usually has three sides. The side closest to the patient is open. You can read more about walkers here.
Crutches[edit | edit source]
Crutches allow people to ambulate with an increased base of support. They transfer weight from the legs to the upper body and are often used by individuals with spinal cord injuries who cannot use their legs to support their weight. You can read more about crutches here.
Footwear[edit | edit source]
When wearing orthotics, patients cannot "slip back" into their favourite pair of shoes.[36]
It is essential to emphasise the importance of appropriate footwear in promoting safe walking habits and minimising injury or falls. Remember to prioritise using suitable footwear to support the patient's rehabilitation journey.
- A proper shoe assessment must be performed, and the following should be considered:
- presence of oedema in the lower extremities
- pressure points after the shoes are removed
- complete a thorough assessment of the ankles, heels, and toes; a patient may not be able to feel their feet and is, therefore, at risk of developing a pressure sore
- When using orthotics, it is recommended that shoes have:[37]
- an enclosed heel and toe
- secure lace or velcro fastening
- removable insole
- heel height as recommended by the orthotist
Resources[edit | edit source]
- Ambulation Prediction After Spinal Cord Injury: What Have We Learned In The Past 10 Years?
- Fallahzadeh Abarghuei A, Karimi MT. The Effects of Lower Limb Orthoses on Health Aspects of the Spinal Cord Injury Patients: A Systematic Review Using International Classification of Functioning, Disability, and Health (ICF) as a Reference Framework. Med J Islam Repub Iran. 2022 Dec 14;36:153.
- Behrman AL, Bowden MG, Nair PM. Neuroplasticity after spinal cord injury and training: an emerging paradigm shift in rehabilitation and walking recovery . Phys Ther. 2006 Oct;86(10):1406-25. Please also see the Supplementary Data section at the bottom of this article for a video demonstration of the plasticity-based approach to walking recovery.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Scivoletto G, Tamburella F, Laurenza L, Torre M, Molinari M. Who is going to walk? A review of the factors influencing walking recovery after spinal cord injury. Frontiers in human neuroscience. 2014 Mar 13;8:141.
- ↑ Van de Crommert HW, Mulder T, Duysens J. Neural control of locomotion: sensory control of the central pattern generator and its relation to treadmill training. Gait Posture. 1998 May 1;7(3):251-263.
- ↑ Sherrington CS. Flexion-reflex of the limb, crossed extension-reflex, and reflex stepping and standing. J Physiol. 1910 Apr 26;40(1-2):28-121.
- ↑ 4.0 4.1 4.2 4.3 4.4 Behrman AL, Bowden MG, Nair PM. Neuroplasticity after spinal cord injury and training: an emerging paradigm shift in rehabilitation and walking recovery. Phys Ther. 2006 Oct;86(10):1406-25.
- ↑ Grillner S, Rossignol S. On the initiation of the swing phase of locomotion in chronic spinal cats. Brain Res. 1978 May 12;146(2):269-77.
- ↑ Hiebert GW, Whelan PJ, Prochazka A, Pearson KG. Contribution of hind limb flexor muscle afferents to the timing of phase transitions in the cat step cycle. J Neurophysiol. 1996 Mar;75(3):1126-37.
- ↑ Angeli CA, Boakye M, Morton RA, Vogt J, Benton K, Chen Y, Ferreira CK, Harkema S. Recovery of Over-Ground Walking after Chronic Motor Complete Spinal Cord Injury. N Engl J Med 2018; 379:1244-1250.
- ↑ Stroke Engine. Glossary of Terms. Available from http://www.medicine.mcgill.ca/strokengine/definitions-en.html. [last access 11.01.2023]
- ↑ Lam T, Noonan VK, Eng JJ; SCIRE Research Team. A systematic review of functional ambulation outcome measures in spinal cord injury. Spinal Cord. 2008 Apr;46(4):246-54.
- ↑ Lord SE, McPherson K, McNaughton HK, Rochester L, Weatherall M. Community ambulation after stroke: how important and obtainable is it and what measures appear predictive? Arch Phys Med Rehabil. 2004 Feb;85(2):234-9.
- ↑ 11.0 11.1 11.2 11.3 11.4 Salbach NM, O'Brien K, Brooks D, Irvin E, Martino R, Takhar P, Chan S, Howe JA. Speed and distance requirements for community ambulation: a systematic review. Arch Phys Med Rehabil. 2014 Jan;95(1):117-128.e11.
- ↑ 12.0 12.1 Promkeaw D, Arrayawichanon P, Thaweewannakij T, Mato L, Amatachaya P, Amatachaya S. Various surfaces challenge gait characteristics of ambulatory patients with spinal cord injury. Spinal Cord 2019; 57: 805–813.
- ↑ Hussey RW, Stauffer ES. Spinal cord injury: requirements for ambulation. Arch Phys Med Rehabil. 1973 Dec;54(12):544-7.
- ↑ Brehm MA, Ploeger HE, Nollet F. Self-reported functional ambulation is related to physical mobility status in polio survivors; a cross-sectional observational study. Ann Phys Rehabil Med. 2021 Jul;64(4):101428.
- ↑ Van Hedel HJ; EMSCI Study Group. Gait speed in relation to categories of functional ambulation after spinal cord injury. Neurorehabil Neural Repair. 2009 May;23(4):343-50.
- ↑ 16.0 16.1 16.2 Draganich C, Weber KA 2nd, Thornton WA, Berliner JC, Sevigny M, Charlifue S, Tefertiller C, Smith AC. Predicting Outdoor Walking 1 Year After Spinal Cord Injury: A Retrospective, Multisite External Validation Study. J Neurol Phys Ther. 2023 Jul 1;47(3):155-161.
- ↑ Moon J, Yu J, Choi J, Kim M, Min K. Degree of contribution of motor and sensory scores to predict gait ability in patients with incomplete spinal cord injury. Annals of Rehabilitation Medicine. 2017 Dec 28;41(6):969-78.
- ↑ 18.0 18.1 Van Middendorp JJ, Hosman AJ, Donders AR, Pouw MH, Ditunno JF, Curt A, Geurts AC, Van de Meent H. A clinical prediction rule for ambulation outcomes after traumatic spinal cord injury: a longitudinal cohort study. The Lancet. 2011 Mar 19;377(9770):1004-10.
- ↑ Cathomen A, Maier D, Kriz J, Abel R, Röhrich F, Baumberger M, Scivoletto G, Weidner N, Rupp R, Jutzeler CR, Steeves JD; EMSCI study group; Curt A, Bolliger M. Walking Outcome After Traumatic Paraplegic Spinal Cord Injury: The Function of Which Myotomes Makes a Difference? Neurorehabil Neural Repair. 2023 May;37(5):316-327.
- ↑ Nas K, Yazmalar L, Şah V, Aydın A, Öneş K. Rehabilitation of spinal cord injuries. World J Orthop. 2015 Jan 18;6(1):8-16.
- ↑ 21.0 21.1 Mohammad MT. Gait Rehabilitation Using Orthotics in Spinal Cord Injury Course. Plus, 2024.
- ↑ Hope JM, Field-Fote EC. Assessment of Dorsiflexion Ability across Tasks in Persons with Subacute SCI after Combined Locomotor Training and Transcutaneous Spinal Stimulation. Bioengineering. 2023; 10(5):528.
- ↑ 23.0 23.1 Waters RL, Miller L. A Physiologic Rationale for Orthotic Prescription in Paraplegia. Clinical Prosthetics and Orthotics 1987;11(2):66-73.
- ↑ 24.0 24.1 24.2 24.3 24.4 Waters RL, Lunsford BR. Energy cost of paraplegic locomotion. J Bone Joint Surg Am. 1985 Oct;67(8):1245-50.
- ↑ Engel-Haber E, Zeilig G, Haber S, Worobey L, Kirshblum S. The effect of age and injury severity on clinical prediction rules for ambulation among individuals with spinal cord injury. Spine J. 2020 Oct;20(10):1666-1675.
- ↑ 26.0 26.1 26.2 Karimi MT. The physiological benefits and problems associated with standing and walking orthoses in individuals with spinal cord injury - a meta-analytic review. Journal of Orthopaedics, Trauma and Rehabilitation 2012; 16(1): 37-40.
- ↑ Fallahzadeh Abarghuei A, Karimi MT. The Effects of Lower Limb Orthoses on Health Aspects of the Spinal Cord Injury Patients: A Systematic Review Using International Classification of Functioning, Disability, and Health (ICF) as a Reference Framework. Med J Islam Repub Iran. 2022 Dec 14;36:153.
- ↑ 28.0 28.1 Uustal H. Lower Extremity Orthotics. Pathology and Prescription. Available from https://medicine.missouri.edu/sites/default/files/orthotics%20review%20case/LowerExtremityOrthotics.pdf [last access 13.01.2023]
- ↑ Fisher D. Introduction to Complex Orthoses Course. Plus. 2022.
- ↑ Hope Rehab.HKAFO - Hip Knee Ankle Foot ORTHOSIS, Helping To Rehabilitate Ahmed. Available from: https://www.youtube.com/watch?v=Zsbxak-mBNo [last accessed 13/01/2024]
- ↑ 31.0 31.1 Scivoletto G, Petrelli A, Lucente LD, Giannantoni A, Fuoco U, D'Ambrosio F, Filippini V. One year follow up of spinal cord injury patients using a reciprocating gait orthosis: preliminary report. Spinal Cord. 2000 Sep;38(9):555-8.
- ↑ Jaco Deist. Tania van Twisk, Reciprocating Gate Orthosis. Available from: https://www.youtube.com/watch?v=VoDVZjAoh7M [last accessed 18/01/2024]
- ↑ Good Shepherd Rehabilitation Network. Spinal Cord Injury: Kevin Oldt Walks in KAFO Leg Braces. Available from: https://www.youtube.com/watch?v=ikRZZMR8Wkc [last accessed 13/01/2024]
- ↑ Health is Wealth. Spinal Cord Injury: paraplegic T12 walking with elbow crutch and stair climbing training. Available from: https://www.youtube.com/watch?v=Nrr-YkVixeo [last accessed 10/02/2024]
- ↑ Jaime Newell. Walking in AFOs - T7 Incomplete spinal cord injury. Available from: https://www.youtube.com/watch?v=vSiwEqcw_5U [last accessed 13/01/2023]
- ↑ Wearing Shoes After A SCI: Three Things You Should Know. Available from https://passionatepeople.invacare.eu.com/wearing-shoes-sci-three-things-know/ [last access 9.2.2024]
- ↑ KAFO Buying Guide: What Physicians Should Know When Selecting One for Their Patients. Available from https://www.anatomicalconceptsinc.com/articles/kafo-buying-guide-what-physicians-should-know-when-selecting-one-for-their-patients [last access 9.2.2024]