Knee Rotary Instability
Original Editors - Mary Harris
Top Contributors - Bryan Jacobson, Shannon Davis, Mary Harris, Laura Ritchie, Misty Hillin, Kim Jackson, Yoni Strackx, 127.0.0.1, Admin, WikiSysop, Wanda van Niekerk, Tony Lowe, Evan Thomas, Johnathan Fahrner, Scott Buxton, Vinit Kothekar and Kai A. Sigel - Mary Harris, Shannon Davis, Misty Hillin, Bryan Purkey, Bryan Jacobson
Definition/Description[edit | edit source]
Knee rotary instability is observed excessive rotation of the tibia in relation to the femur. There are multiple types of rotary instability, however the majority of research focuses on the impact of the structures in the posterolateral corner and their influence on rotary instability. Injuries to the Posterolateral Corner (PLC) can result in posterolateral rotatory instability (PLRI) of the knee, which is a pathological instability that is caused by posterolateral tibial subluxation when an external rotational force is applied to the knee joint [1], or a direct blow to the anteromedial knee. [2] A rotary instability often occurs with concomitant ligamentous injuries making it difficult to detect/diagnose. [3]
Epidemiology/Etiology[edit | edit source]
- Isolated injury of the PLC is reported to represent only 1.6% of all acute ligamentous knee injuries[4]
- Concurrent ligamentous knee injuries have been reported in 43% to 80% of patients in studies examining both acute and chronic PLC injuries.[5]
- 68% of cases had a PLC injury and 5 of 7 patients with a medial tibial plateau fracture had a PLC injury.
- ACL reconstruction causes a persistent pivot shift in over 15% of cases. Main cause of graft failure is the presence of unrecognized, and therefore untreated, PLRI.[6][2]
- Diagnosing PLRI is difficult because it occurs rarely and is slow to develop. In one study, PLRI was not recognized in 34 (50%) patients at the initial diagnosis. [3]
- One study reported mechanisms of injury were: traffic accidents accounted for (55%), Sports activities (30%), missteps/falls/other activities (15%)[3]
Characteristics/Clinical Presentation[edit | edit source]
Patients with knee rotatory instability will often present with joint line tenderness accompanied by swelling in the posterolateral corner of the knee. Due to the anatomical path of the common fibular nerve, injuries in this area up to 30% of the time present with neurological symptoms such as numbness, weakness, and paresthesias. Many patients with knee rotary instability report episodes of giving way or knee buckling during the stance phase of gate and pivoting or twisting movements. Some patients present with an unpredictable giving way of the knee without provocation or simply when just standing.(Ferarri) Standing posture can present with genu varum while the stance phase of gait can present with hyperextension varus thrust. If patient experiences this they may try to walk keeping the knee slightly flexed when walking to avoid. [7]
Differential Diagnosis[edit | edit source]
Damage to:
Or any combination of the above.
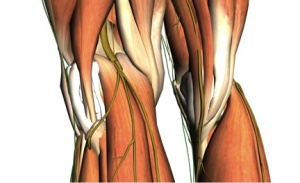
Relevant Anatomy[edit | edit source]
The Posteriolateral compartment (PLC) can be described as consisting of 5 structures (2 muscles and 3 ligaments); the lateral head of the gastrocnemius, the popliteus, the popliteofibular ligament, the lateral collateral ligament (LCL), and the arcuate ligament–fabellofibular ligament complex. The biceps femoris tendon and iliotibial band also contribute to the stability of the PLC of the knee, and may be damaged with injuries in this region.
The PLC serves as the primary restraint to both varus and external rotation forces, with the PCL acting as a secondary restraint. The LCL plays the greatest role in resisting varus stress, while the other components of the PLC play a larger role in resisting external rotation of the lateral side of the tibia on the femur. The popliteus and popliteofibular ligament, in particular, have been shown to be the most important structures in resisting external rotation.[7]
Disruption of the PLC with an intact PCL results in increased varus and external rotation of the knee, most pronounced at 30° of knee flexion, while disruption of the PCL with an intact PLC results in increased posterior translation of the tibia, most pronounced at 90° of knee flexion. Disruption of both the PLC and PCL causes increased varus angulation, external rotation, and posterior translation at all angles of knee flexion [7].
| Rotatory Instability | Primary Restraints | Tests |
|---|---|---|
| AMRI (Antero-medial Rotatory instability) |
PMC which includes posterior horn of Medial meniscus, POL, semimebraous expansions, Coronary ligament, OPL | Slocum test |
| ALRI (Antero-lateral Rotatory Instability) |
ACL and MCL | pivot shift test Anterior Drawer test Jerk Test of Hughston Losee test Side lying test of Slocum Noyes test/ Flexion rotation drawer test |
| PMRI (Postero-medial Rotatory Instability) |
Medial Capsular ligament tibial collateral ligament POL ACL |
|
| PLRI (Postero-Lateral Rotatory Instability) |
PLC which includes LCL, Arcuate ligament complex, fabellofibular ligament, postero-lateral capsule |
Dial test (prone external roation test) posterolateral drawer test (PLD test) Reverse pivot shift test External rotation recurvatum test posterolateral external rotation test |
Examination[edit | edit source]
Neuro Exam: pay special attention to the common fibular nerve
Check blood supply for possible arterial disruption[7]
Special Tests:[3]
| [8] |
Dial Test: 30* knee flexion, Tibial external rotation
Dial test video provided by Clinically Relevant
- Look for posterior sag, and apply anterior force if supine or test prone for neutral tibial positioning.
Reverse Pivot Shift Test: Original Pivot Shift
Reverse Pivot Shift Test video provided by Clinically Relevant
- (+) test, knee subluxation in flexion and posterior sag of proximal tibia
- False positive rate- 35%
External Rotation Recurvatum Test
- (+) Test, hyperextension, external rotation of tibia, and tibial varus
Posterolateral Drawer Test
- Significant increase in PL translation in 15* external rotation
Varus Stress Test
Varus Stress Test video provided by Clinically Relevant
In the above video, the following findings are observed;
(+) Dial test demonstrating Ext Rot, and Lateral tibial subluxation
(+) Posterior drawer test
(+) Varus test
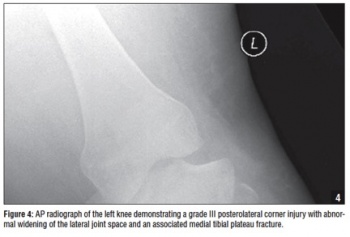
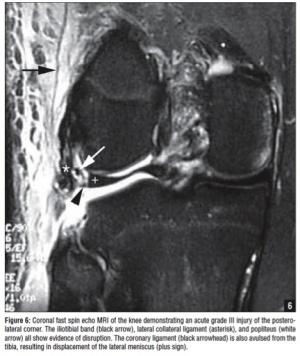
Imaging (photos used from Ricchetti)[7]
Standard radiographs of the knee can show several findings suggestive of acute PLC injury, including abnormal widening of the lateral joint space, fibular tip avulsion fracture or fracture of the fibular head, avulsion fracture off Gerdy’s tubercle in iliotibial band injuries, tibial plateau fracture, or even a Segond fracture.[7]
Although Segond fractures typically occur with ACL tears, they also can occur in isolated PLC injuries. Recent studies have shown that either T1- or T2-weighted coronal oblique images through the knee and including the entire fibular head and styloid process provide the best visualization of the individual structures of the PLC.[7]
Magnetic resonance imaging will also detect associated injuries, including ACL and PCL tears, fractures, and bone contusions, which typically occur in the medial femoral condyle or medial tibial plateau.
Outcome Measures[edit | edit source]
The same measures that are used during the examination process can be used post-op to test for knee instability. Additionally, you can observe tibial ER during gait and gather subjective information from the patient such as if episodes of giving way have decreased and their overall sense of stability of their knee.
Diagnosis[edit | edit source]
There is no single definitive tool exists in diagnosing posterolateral corner injuries.[3]
Grade 1:
- Tibial external rotation 5-10* difference, without varus instability[2]
Grade 2:
- Increased ER >10* difference, OR posterolateral subluxation of tibial plateau with grade 0-2 varus instability[2]
Grade3:
- Tibial exernal rotation >10* difference /s firm end point, with grade 3 varus instability from LCL injury[2]
Medical Management[1][9][10][11][edit | edit source]
Knee Rotary instability is commonly seen with injury to the cruciate ligaments. It is important with either type of injury to address the instability by reconstructing the PLC concurrently. Isolated reconstruction of the ACL and PCL alone is not enough to provide rotary stability. Reconstruction of the PLC is necessary to reset the knee to nearly physiological laxity patterns. Also, the PFL and PT have similar in situ forces that add to the idea that PLC components may play equally important roles in restoring knee stability.
Over time this strain from lack of stability leads to lengthening, laxity and an increased force on the ligament grafts leading to graft failures. It has been suggested numerous times that this instability is in fact the main cause of graft failure.
It was found that that reconstruction of the PLC is best done at the same time as the PCL and ACL reconstructions.
Management according to PLC Grade:[7]
- Grade III almost always require surgery.
- Grade II can be managed non-operatively. A more severe grade II injury or an injury associated with cruciate ligament tears or tibial plateau fractures should be addressed surgically.
- Grade I is treated nonoperatively with good results.
Surgery[edit | edit source]
| [12] |
If the patient is stable, surgery should be performed within 3 weeks of injury so that the PLC can be repaired primarily.[7]
Type
Reconstruction rather than repair is most common in patients who have posterolateral tears and injuries.[13]
Reconstructive procedures can again be divided into those that attempt to restore the normal anatomy of the PLC and those that nonanatomically stabilize the PLC by tightening specific structures.[7] The best way to reconstruct the PLC is being researched.
Grafts
Hamstring autograft, particularly the tendon of the biceps femoris long head has been shown to be effective.[9]
Other grafts being researched:[7]
- Achilles tendon allograft
- Anterior or posterior tibial tendon allograft
- Patellar tendon allograft or autograft
- Iliotibial band allograft or autograft
Procedures
A modified version of Larson’s technique called the modified posterolateral corner sling method is commonly used. The most important structures for reconstruction of the PLC are the popliteus tendon, LCL, and specifically the popliteofibular ligament.[14]
The two common techniques:[9]
- Passing through the lateral aspect of the tibia.
- Passing through the fibular head tunnel along with a 1 cm anterior lateral epicondyle tunneling by passing the tendon medially with a bioabsorbable screw fixation at the lateral side.
The fibular head tunnel shows better results than the tibial tunneling.
Advantages:
- Lower operation time leading to less surgical morbidity
- Better rotational stability
- Better isometricity
Complications:
- Fibular head fracture
- Fibular nerve injury
General complications:[7]
- Wound problems such as infection or hematoma formation
- Post- op knee stiffness (typically loss of flexion)
- Failure of the repair or reconstruction
- Hamstring weakness (especially in biceps tendon procedures)
- Hardware irritation
Physical Therapy Management[edit | edit source]
It has been shown that protected weight bearing of the extremity for the first 2 weeks is usually necessary, and should be followed by a progressive rehabilitation program. Rehabilitation should include quadriceps-strengthening and progressive resistance exercises, as well as protected range of motion activities.[7] Physical therapy should impairment-based treatment. The knowledge of the physical therapist and patient’s presentation should be used to determine where the patient should start and how rapidly they should progress. Exercises should start with basic muscle strengthening and then move to higher level sport specific drills.[7]
Opened Chain exercises have historically thought to produce extra shearing forces, however it has proven that greater quad strength gains can be made compared to closed chain.
- Opened Chain Exercises:
- Knee Extensions
- Active Flexion/ Extension of Knee with weight and/or resistance
- Quad Sets
Even though there is a proven benefit from open chain exercises, majority of time should be spent doing closed chain exercises because they can provide proprioceptive input and proper co-contraction of antagonist and agonists muscles. In addition it can help to improve the strength, function, and stability both a joint above and below.
- Closed Chain Exercises:
- Squats
- Lunges
- Single Leg Squats
- Stair Climbing
- Biking
Perturbation exercises help to provide protection of the joint, improve knee kinematics, and neuromuscular training.[15] Exercises that can be performed are: single leg stance and squats, double-leg activities, and lunges. These should be performed on surface that require the patient to create there own stability.
- Baps board
- Trampoline
- Rockerboard
- Rollerboard/Platform
All of these should initially begin anterior to posterior and medial to lateral then progress to diagonal and rotational movements.
Additional things that could be addressed are muscles of the hip and ankle, bracing and taping which would help to provide stability in the entire lower limb.[7]
Key Research[edit | edit source]
Acute and chronic management of posterolateral corner injuries of the knee
Ricchetti E, Sennett B, Huffman G. Acute and chronic management of posterolateral corner injuries of the knee [corrected] [published erratum appears in ORTHOPEDICS 2008 Jul;31(7):725]. Orthopedics [serial online]. May 2008;31(5):479-490. Available from: CINAHL Plus with Full Text, Ipswich, MA. Accessed July 13, 2011.
Clinical Bottom Line[edit | edit source]
Knee rotary instability occurs most commonly with concomitant ligamentous injuries. It is difficult to diagnose, treat and is often missed due to different clinical presentations and lack of protocol. Physical therapy treatment and surgical intervention will both depend on the severity, location, structures injured, and patient's abilities and goals.
References[edit | edit source]
- ↑ 1.0 1.1 Lee S, et al. Combined reconstruction for posterolateral rotatory instability with anterior cruciate ligament injuries of the knee. Knee Surg Sports Traumatol Arthrosc (2010) 18:1219–1225.
- ↑ 2.0 2.1 2.2 2.3 2.4 Young-Bok J, et al. The Inf uence of Tibial Positioning on the Diagnostic Accuracy of Combined Posterior Cruciate Ligament and Posterolateral Rotatory Instability of the Knee. Clinics in Orthopedic Surgery 2009;1:68-73.
- ↑ 3.0 3.1 3.2 3.3 3.4 Goo Kim, J et all. Correlation between the rotational degree of the dial test and arthroscopic and physical findings in posterolateral rotatory instability. Knee Surg Sports Traumatol Arthrosc (2010) 18:123–129
- ↑ Ricchetti E, Sennett B, Huffman G. Acute and chronic management of posterolateral corner injuries of the knee [corrected] [published erratum appears in ORTHOPEDICS 2008 Jul;31(7):725]. Orthopedics [serial online]. May 2008;31(5):479-490. Available from: CINAHL Plus with Full Text, Ipswich, MA. Accessed July 13, 2011.
- ↑ Ricchetti E, Sennett B, Huffman G. Acute and chronic management of posterolateral corner injuries of the knee [corrected] [published erratum appears in ORTHOPEDICS 2008 Jul;31(7):725]. Orthopedics [serial online]. May 2008;31(5):479-490. Available from: CINAHL Plus with Full Text, Ipswich, MA. Accessed July 13, 2011.
- ↑ Tiamklang T, Sumanont S, Foocharoen T, Laopaiboon M. Double-bundle versus single-bundle reconstruction for anterior cruciate ligament rupture in adults. Cochrane Database of Systematic Reviews 2010, Issue 3. Art. No.: CD008413. DOI: 10.1002/14651858. CD008413.
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 7.11 7.12 7.13 7.14 Ricchetti E, Sennett B, Huffman G. Acute and chronic management of posterolateral corner injuries of the knee [corrected] [published erratum appears in ORTHOPEDICS 2008 Jul;31(7):725]. Orthopedics [serial online]. May 2008;31(5):479-490. Available from: CINAHL Plus with Full Text, Ipswich, MA. Accessed July 13, 2011.
- ↑ Dr Bancha, Dial Test PLC Injury Knee Ligament Examination [Video]. YouTube. http://www.youtube.com/watch?v=4ffLZG8dLxs. Published June 27, 2008. Accessed July 16, 2011.
- ↑ 9.0 9.1 9.2 Jung Y, Jung H, Lee S, et al. Posterolateral corner reconstruction for posterolateral rotatory instability combined with posterior cruciate ligament injuries: comparison between fibular tunnel and tibial tunnel techniques. Knee Surgery, Sports Traumatology, Arthroscopy [serial online]. March 2008;16(3):239-248. Available from: CINAHL Plus with Full Text, Ipswich, MA. Accessed July 16, 2011.
- ↑ Tashiro Y, Okazaki K, Iwamoto Y, et al. Quantitative assessment of rotatory instability after anterior cruciate ligament reconstruction. American Journal of Sports Medicine [serial online]. May 2009;37(5):909-916. Available from: CINAHL Plus with Full Text, Ipswich, MA. Accessed July 16, 2011.
- ↑ Mauro C, Sekiya J, Stabile K, Haemmerle M, Harner C. Double-bundle PCL and posterolateral corner reconstruction components are codominant. Clinical Orthopaedics & Related Research [serial online]. September 2008;466(9):2247-2254. Available from: CINAHL Plus with Full Text, Ipswich, MA. Accessed July 16, 2011.
- ↑ ProPrioSense. Postero-lateral Corner Reconstruction of the Knee. Available from: http://www.youtube.com/watch?v=Zz_U2CWES3s [last accessed 21/09/14]
- ↑ Stannard J, Brown S, Farris R, McGwin G, Volgas D. The posterolateral corner of the knee: repair versus reconstruction. American Journal of Sports Medicine [serial online]. June 2005;33(6):881-888. Available from: CINAHL Plus with Full Text, Ipswich, MA. Accessed July 10, 2011.
- ↑ Veltri D, Warren R. Anatomy, biomechanics and physical findings in posterolateral knee instability. Clinics in Sports Medicine [serial online]. July 1994;13(3):599-614. Available from: CINAHL Plus with Full Text, Ipswich, MA. Accessed July 10, 2011.
- ↑ 15.0 15.1 Chmielewski T, et al. Perturbation Training Improves Knee Kinematics and Reduces Muscle Co-contraction After Complete Unilateral Anterior Cruciate Ligament Rupture. Phys Ther (2005) 85:740-749. (Level of evidence = 3B)
- ↑ Frobell R, Roos E, Roos H, Ranstam J, Lohmander L. A randomized trial of treatment for acute anterior cruciate ligament tears. New England Journal of Medicine [serial online]. July 22, 2010;363(4):331-342. Available from: CINAHL Plus with Full Text, Ipswich, MA. Accessed July 16, 2011. (Level of Evidence = 1B)