Leg and Foot Stress Fractures
Original Editors
Top Contributors - Melissa Osti, Brittany Buenteo, Holly Pulket, Brenda Walk, Kim Jackson, Corin Arundale, Admin, Wanda van Niekerk, WikiSysop, Ellyne De Prest, 127.0.0.1, Rachael Lowe, Naomi O'Reilly, Kai A. Sigel and Elise Audiens - Holly Pulket, Corin Arundale, Brenda Walk, Brittany Buenteo, Melissa Osti
Definition/Description[edit | edit source]
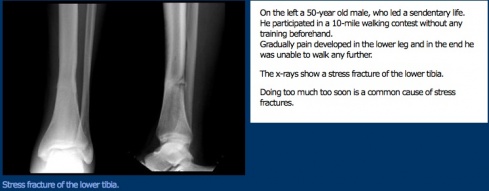
Stress fractures occur in bones that undergo mechanical fatigue.[1] They are a consequence of exceeding repetitive submaximal loads, which creates an imbalance between bone resorption and bone formation.[2] The fractures usually begin in locations of great stress; this is called “crack initiation”.[2] If this microscopic crack is not able to heal and is subjected to further loading, the microdamage will increase and the crack will enlarge. This increase in damage can cause the bone to break on a macroscopic level.[2]
Epidemiology/Etiology[edit | edit source]
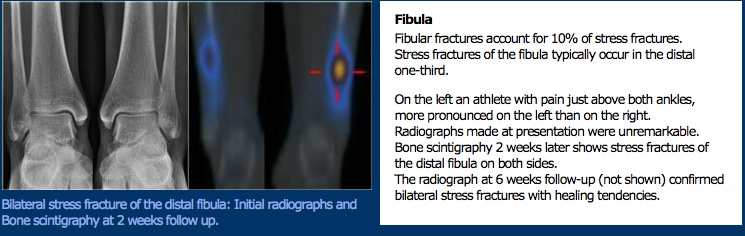
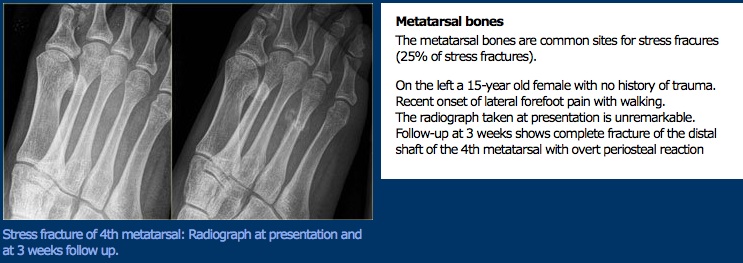
It is estimated that 15-20% of overuse injuries are stress fractures.[1] Activities of impact with repetitive loading such as marching and running are associated with these types of fractures.[3] About 50% of stress fractures take place in the tibia; however, a stress fracture can occur in any bone. The foot, especially the second metatarsal, is another common place for stress fractures.[4] It has been reported that females have a 1.5 to 12 times higher risk of getting a stress fracture as compared to males.[5]
Stress fractures may be due to multiple factors including activity level, bone quality, anti-inflammatory drugs, radiation, nutritional status,osteoporosis, imbalanced hormones, sleep deprivation, and collagen anomalies. The frequency of stress fractures is dependent upon the composition of bone, adjacent muscle attachments, the vasculature, systemic factors, and the mode of athletic activity.[2] Other possible risks include age, sex, footwear, and training regimen.[6] High level female athletes who are inclined to the athlete triad (amenorrhea,eating disorders, and osteoporosis) and male endurance athletes who have unusually low levels of sex hormones are also at risk for stress fractures.[2]
From a biomechanical perspective, stress fractures may be a consequence of fatigued muscle, which then causes the bone to receive excess force.[2] In addition, the alignment of the lower extremity has been proposed to play a role in the risk of stress fractures.[3] Furthermore, earlier studies have shown that narrow tibias, a high degree of hip external rotation, a varus ankle and forefoot, ankle hyperpronation, pes cavus, and leg-length discrepancy may increase an athlete’s risk for stress fractures.[6] Evidence is inconclusive for some of these factors.
Clinical Presentation[edit | edit source]
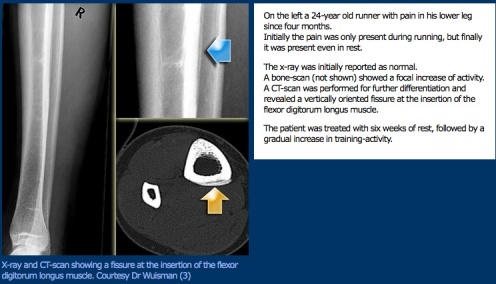
Clinical presentations can vary among patients; therefore, obtaining a thorough history is imperative to determine whether a patient may have a stress fracture. A patient may describe their symptoms to progressively get worse over time with activity, and no specific mechanism of injury. Initially the pain may only occur during activity but eventually become constant over time. It is important to consider that patients may not mention increases in activity or activity modifications that are key findings for the physical therapist.[7] Patients may present with mild edema and erythema in the area of pain, focal/point tenderness (covered by a single finger), leg length discrepancy, and increased pain with weight bearing activities encouraging an antalgic gait. A tuning fork test along the area of pain should exacerbate the patient’s symptoms.[8] Runners, athletes, and military members are commonly affected with stress fractures.[7] Without sufficient rest between workouts or competitions, patients are at increased risk. The young female athlete is more predisposed to stress fractures due to the triad of risk factors within this population, which are also detrimental to bone mass.[7]
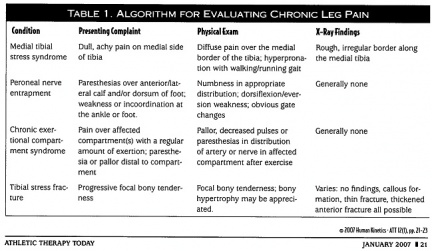
Differential Diagnosis [edit | edit source]
The differential diagnosis will vary depending on location of pain. Other possible diagnoses include infection, tumor, compartment syndrome, arthritis, nerve entrapment, medial tibial stress syndrome, and other soft tissue injuries.[7]
Compartment syndrome develops from pressure within the muscle compartments of the lower leg, which are divided by fascial layers. Pressure within the compartments can result from increased oxygen demand and subsequent blood flow to the exercised muscle.[8] Patients may present with leg cramps, muscle tightness, severe pain, foot drop, and paresthesia of the foot.[8] If the compartment syndrome is considered an acute episode, it is a medical emergency, and surgical fasciotomy is the preferred treatment.[8]
Medial tibial stress syndrome (MTSS) comprises periostitis at the junction of the middle and distal thirds of the medial tibial border. This syndrome can result from traction stress of the soleus, flexor digitorum longus, or deep crural fascia.[7] Bone scans can be used to diagnose MTSS, and will show increased uptake of longer segments of the bone, compared to focal areas that show up with stress fractures.[7] During the exam, patients with MTSS may experience diffuse tenderness along the tibial border.
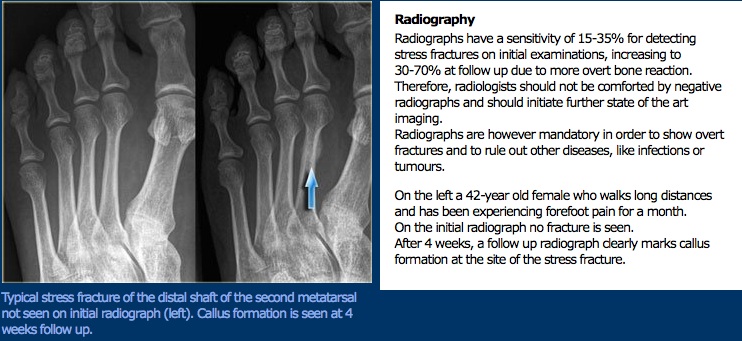
If a stress fracture is suspected after the initial evaluation, the therapist should refer for medical imaging to rule in or out the diagnosis. Radiographs are typically the first tool used,[9] despite poor sensitivity for diagnosis of stress fractures.[10] Stress fractures usually don't appear on x-rays for two to six weeks post-injury;[11][9] when they are visible, they will appear as radiolucent lines and may have cortical thickening.[12][9][13] The gold standard imaging for stress fractures is the bone scan; stress fractures are visible within 2-3 days of injury.[10]
Examination[edit | edit source]
When evaluating an adult with a lower extremity stress fracture, a thorough history is important.
Key history findings of an individual with a stress fracture:[9][12]
- Pain with weight bearing
- Recent increase in activity (i.e. high intensity and/or high frequency)
- Gradual onset
- Begins as pain with stress, eventually progressing to pain at rest and during the night
During the physical examination, the clinician will want to take an impairment based approach. Important aspects of the evaluation will include observation of posture and biomechanics, gait analysis, leg length discrepancy, tenderness with palpation, and range of motion.[13] Patients with stress fractures typically will have tenderness to palpation and edema in surrounding soft tissues.[9] According to Hatch et al 2007,[11] during the physical examination it may be important to perform all of the following: a neurological screen for sensation, a vascular examination (capillary refill and lower extremity pulses), inspect the skin for deformity, edema, or ecchymosis, and range of motion to determine if there is a disproportionate amount of pain with movement.
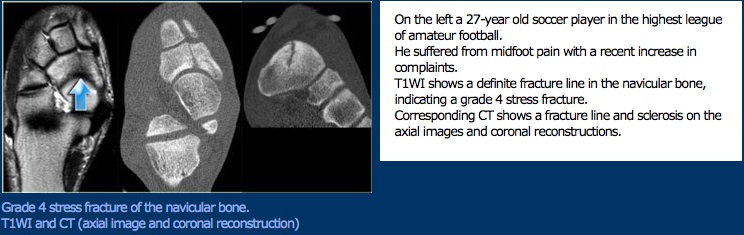
With regards to navicular stress fractures, which are one of the most common types of foot stress fracture, foot shape has been implicated as a risk factor, but evidence is inconsistent.[7][14] Injuries appear to occur in patients with pes planus, pes cavus, and normal feet.
Medical Management[edit | edit source]
Operative and non-operative treatment options exist for leg and foot stress fractures. There are several factors that contribute towards whether or not surgery is used to repair a stress fracture. One factor is location--the vascularity of the region will impact how well the stress fracture heals. Brockwell et al[15] identify areas of "high-risk" as the talus, navicular, medial malleolus, hallux sesamoids, and the base of the 5th metatarsal bone. As these areas are considered higher risk, surgery is recommended as the first intervention. However, the metatarsals have a good blood supply, and thus, a more conservative form of treatment is possible. Recommendations include complete cessation of the activity that caused the stress fracture for 4-8 weeks, and the weight bearing status can be determined by the level of the patient's pain. On the other hand, medial malleolar stress fractures are considered high-risk, due to the likelihood of progression from stress fracture to acute fracture.[16] These fractures can be treated with open reduction and internal fixation surgery, which leads to a faster recovery than the 6-8 months needed through conservative treatment.
Another factor to consider in the medical management of stress fractures is the profile of the patient. Sometimes, with high-level athletes (a population particularly at risk for this type of injury), surgery is regarded as a more desirable option due to the reduced time-frame to return to normal activity. In a systematic review conducted by Torg et al[17] in 2010, researchers found no significant difference in outcomes between surgical intervention and conservative non-weight bearing with casting. However, another study showed a difference in average time for athletes to return to sport, with conservative management rehabilitation lasting an average of 5.6 months, as opposed to 3.8 months after surgery.[18] The same study found an 86% success rate in the healing of non-displaced stress fractures through casting and non-weight bearing for 6-8 weeks. In the Torg review, it was also noted that conservative treatment that included some degree of weight bearing (either weight bearing with rest, or activity limitation) can lead to re-injury or frank fracture. In a study by Burne et al in 2005, researchers concluded that "there is limited evidence to support surgical intervention as a first line of management." For surgery, it is also important to consider the type of stress fracture, and if it is displaced, fragmented, or if conservative treatment has already been attempted and has been ineffective. Surgery typically consists of open reduction with internal fixation with a screw, and sometimes includes a bone graft.
Physical Therapy Management[edit | edit source]
Physical therapy strategies include patient education and guidance for activity modification.
Initial treatment should be to decrease the abnormal stresses on the bone to a level within normal physiological limits, allowing healing to occur.[19] This usually consists of decreased or non-weight bearing for 1-2 months, depending on severity of fracture.[13] Aquatic exercise, cycling, and upper-body weight training allows the affected lower extremity to rest while the patient maintains aerobic conditioning. Once the affected area is pain-free and cleared by the physician, weight bearing should be reintroduced for bone remodeling to occur.[13] Complete rest could prevent bone from healing correctly and cause muscle atrophy and deconditioning, and should be avoided.[19] Using pain or discomfort as the guiding factor in determining appropriate activities and stress load,[13] the patient may cross train or perform other physical activity to maintain health, keeping the intensity below that which provokes symptoms.[19] Crutches or other assistive devices may be prescribed to decrease weight bearing or correct for a limp.[19] The lower extremities should be assessed for alignment, and orthotics used to correct predisposing biomechanical factors.[19] A period of relative rest and activity modification is extremely important to healing. Progressive muscle strengthening will also help the patient return safely to their normal activities after the fracture has healed, and may be key to preventing recurrence.[19]
Patient Education
Patient education will help the patient define the cause of the stress fracture and avoid recurrence. Running is often the cause of stress fracture, and usually occurs when training conditions are changed abruptly, especially excess mileage.(level of evidence 2a)[20] Longevity of training (year-round) is also correlated.[20] Therefore, it is important for runners to assess their training program and other factors, like foot type and running surface. In a study of recurrent stress fractures, 60% of the affected athletes were runners; 40% of those had cavus feet, compared to 13% in the control group of non-injured runners. Since no prospective data indicates that treating cavus feet will lessen injury risk,[20] it may be useful for the patient to simply know their foot type and the correlation to injury for personal training guidance. Strong evidence for preventing running injury exists only for controlling training errors, mainly by limiting total mileage. Moderate evidence identifies cavus feet as a risk factor, and weaker evidence identifies leg length discrepancy. Orthotics may lessen the risk of stress fracture, but studies do not draw an identifiable connection to specific anatomical variations.[20] Runners can also make changes to stride length and running pace to decrease risk of tibial stress fracture by decreasing strain magnitude.[21][22] The greater a person’s stride length and the faster the running speed, the greater the strain magnitude on the tibia. A 10% reduction in stride length and a 1 m/s reduction in running speed (both of which increase the number of steps per mile) may help runners decrease their probability for tibial stress fracture.[21][22] Patient education for runners should focus on limiting excess mileage and sudden changes to training schedules. Individualized training programs are recommended to help each patient adapt to the stresses of running.[20]
Bottom Line
Whether or not a runner, to prevent stress fracture, the patient should gradually increase frequency and intensity of exercise, and avoid sudden increases in training that may overwhelm the bone’s ability to repair in response to load.[19] The physical therapist should assess a patient's movements along the entire kinetic chain to help determine their particular needs in activity modification.
Resources[edit | edit source]
Mayo Clinic Information on Stress Fractures
Clinical Bottom Line[edit | edit source]
Stress fractures are a result of excess load on bone occurring during activity. They are preventable with gradual changes to exercise and performing activity in moderation. Stress fractures are generally treated with non-weight bearing and relative rest. Emerging research may provide more evidence for factors that can help cause or prevent stress fractures. These areas include minimalist footwear, foot anatomics, and training parameters.
Note on Emerging Research:
A recent study was published regarding two experienced runners who made the change to minimalist footwear, and developed metatarsal stress fractures.[23] Due to the increasing popularity of minimalist or barefoot-simulating footwear, this is a topic where further research is needed, in order to determine the potential risks and benefits of using this type of running shoe.
References[edit | edit source]
- ↑ 1.0 1.1 Edwards WB, Taylor D, Rudolphi TJ, Gillette JC, Derrick TR. Effects of running speed on a probabilistic stress fracture model. Clinical Biomechanics. 2010;25:372-377.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Maffulli N, Longo UG, Denaro V. Femoral Neck Stress Fractures. Operative Techniques in Sports Medicine. 2009;17:90-93.
- ↑ 3.0 3.1 Milner CE, Hamill J, Davis IS. Distinct Hip and Rearfoot Kinematics in Female Runners With a History of Tibial Stress Fracture. Journal of Orthopaedic and Sports Physical Therapy. 2010;40(2):59-66.
- ↑ Bargfeldt C, Krogsgaard M, Rasmussen SW. Stress fracture in combination with avulsion from the tibia in a marathon runner: a case report. Scandinavian Journal of Medicine and Science in Sports. 2011;21:330-332.
- ↑ Queen RM, Abbey AN, Chuckpaiwong B, Nunley JN. Plantar Loading Comparisons Between Women With a History of Second Metatarsal Stress Fractures and Normal Controls. The American Journal of Sports Medicine. 2009;37(2):390-395.
- ↑ 6.0 6.1 Korpelainen R, Orava S, Karpakka J, Siira P, Hulkko A. Risk Factors for Recurrent Stress Fractures in Athletes. American Orthopaedic Society for Sports Medicine. 2001;29(3):304-310.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 Tuan K, Wu S, Sennett B. Stress Fractures in Athletes: Risk Factors, Diagnosis, and Management. Orthopedics. 2004;27(6):583-586.
- ↑ 8.0 8.1 8.2 8.3 Bettcher S, Asplund C. Exertional Leg Pain. Athletic Therapy Today. 2008;13(6):20-24.
- ↑ 9.0 9.1 9.2 9.3 9.4 Lassus J, Tulikoura I, Konttinen Y, Salo J, Santavirta S. Bone stress injuries of the lower extremity. Acta Orthop Scand 2002; 73 (3): 359–68.
- ↑ 10.0 10.1 Rosenthal MD, Moore JH, DeBerardino TM. Diagnosis of Medial Knee Pain: Atypical Stress Fracture About the Knee Joint. Journal of Orthopaedic and Sports Physical Therapy. 2006;36(7):526-534.
- ↑ 11.0 11.1 Hatch R, Alsobrook J, Clugston J. Diagnosis and Management of Metatarsal Fractures. Am Family Physician 2007;76,817-26.
- ↑ 12.0 12.1 Van der Velde G, Hsu W. Posterior tibial stress fracture: a report of three cases. J Manipulative Physiol Ther 1999;22:341-6.
- ↑ 13.0 13.1 13.2 13.3 13.4 Duran-Stanton A, Kirk K. "March fractures" on a female military recruit. Military Medicine. 2011;176(1):53-55. (Level of Evidence 3a)
- ↑ Oddy M, Davies M. Stress Fractures of the Navicular. Oper Tech Sports Med 2009, 17:115-8.
- ↑ Brockwell J, Yeung Y, Griffith JF. Stress fractures of the foot and ankle. Sports Med Arthrosc. 2009;17(3): 149-59
- ↑ Donley BG; Ilaslan H. Stress fractures of the medial malleolus. Foot Ankle Clin. 2009;14(2):187-204
- ↑ Torg JS, Moyer J, Gaughan JP, Boden B. Management of Tarsal Navicular Stress Fractures Conservative Versus Surgical Treatment: A Meta-Analysis. The American Journal of Sports Medicine. 2010;38(5):1048-1053
- ↑ Khan KM, Fuller PJ, Brukner PD, Kearney C, Burry HC. Outcome of conservative and surgical management of navicular stress fracture in athletes: eighty-six cases proven with computerized tomography. The American Journal of Sports Medicine. 1992;20(6):657-66
- ↑ 19.0 19.1 19.2 19.3 19.4 19.5 19.6 van den Bekerom MP, Kerkhoffs GM, van Dijk CN. Treatment of medial malleolar stress fractures. Operative Techniques in Sports Medicine. April 2009;17(2):106-111. (Level of Evidence 3b)
- ↑ 20.0 20.1 20.2 20.3 20.4 Fields KB, Sykes JC, Walker KM, Jackson JC. Prevention of running injuries. Current Sports Medicine Reports. May 2010;9(3):176-182. (Level of Evidence 2a)
- ↑ 21.0 21.1 Edwards WB, Taylor D, Rudolphi TJ, Gillette JC, Derrick TR. Effects of stride length and running mileage on a probabilistic stress fracture model. Medicine and Science in Sports and Exercise. December 2009;41(12):2177-2184. (Leven of Evidence 2b)
- ↑ 22.0 22.1 Teyhen DS. Feet, Shoes and Injuries: Static and Dynamic Foot Posture. PowerPoint. 2011. (Level of Evidence 3b)
- ↑ Giuliani J, Masini B, Alitz C, Owens BD. Barefoot-simulating Footwear Associated With Metatarsal Stress Injury in 2 Runners. Orthopedics. 2011;34(7):320-323