Lunate Instability
Original Editor - William Silvestri and Jamie Keller as part of the Temple University EBP Project
Top Contributors - Jamie Keller, Laura Ritchie, Admin, Rachael Lowe, Kim Jackson, Scott A Burns, William Silvestri, 127.0.0.1, Evan Thomas, Kai A. Sigel, WikiSysop, Abbey Wright and Anas Mohamed
Clinically Relevant Anatomy[edit | edit source]
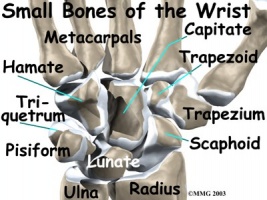
The lunate is one of the eight carpal bones located in the wrist. These eight bones are arranged into two rows with four bones in each.
The proximal row, laterally to medially, consists of:
scaphoid, lunate, triquetrum and pisiform.
The distal row, laterally to medially:
trapezium, trapezoid, capitate and hamate.
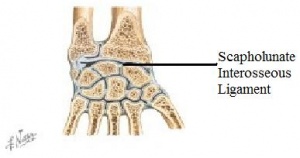
The lunate articulates laterally with the scaphoid, medially with the triquetrum, and inferiorly with the capitate and hamate.
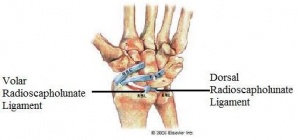
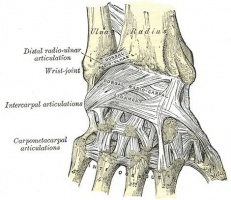
There are several ligaments that attach to the dorsal and palmar surfaces of the carpal bones and hold them together and provide stability in the wrist. Most of the ligaments are named with respect to the two bones they connect.
Mechanism of Injury[edit | edit source]
Scapholunate instability (the most common instability in the wrist) occurs when a person experiences a fall onto an outstretched hand (FOOSH) with the wrist positioned in extension, ulnar deviation, and intercarpal supination.[1][2] Scapholunate instability is considered to be present if at least two of the following three ligaments are injured: volar radioscapholunate ligament, scapholunate interosseous ligament, and dorsal scapholunate ligament. [3] If not treated, dynamic scapholunate instability can progress to rotatory subluxation of scaphoid, scapholunate dissociation, dorsal intercalated segment instability, and then scapholunate advanced collapse.[2]
Clinical Presentation[edit | edit source]
A patient presenting with lunate instability will most likely have a history of trauma to the wrist that has resulted in some type of lesion to the stabilising ligaments of the carpal bones. Additionally, a patient with a history of certain degenerative inflammatory diseases such as chondrocalcinosis, gout, aseptic bone necrosis of the scaphoid or lunate bones, or Madelung deformity (a form of misalignment) can also lead to carpal instability. [4] The patient will have complaints of pain in the involved wrist, specifically around the scaphoid and lunate bones. The pain can be chronic if there is no history of trauma, or acute if the injury is the result of trauma. The pain is typically exacerbated by overuse activities, such as typing on a computer or doing push-ups, or gripping. The patient may deny “clicking” in the wrist, but report a feeling of “instability” with some activities.
Diagnostic Procedures[edit | edit source]
Physical Exam[edit | edit source]
The wrist will most likely not be oedematous or tender when palpated if there has been no history of trauma. Full range of motion may be preserved with a chronic type of injury. A tender dorsal scapholunate interval may be evident but it may appear normal in radiographs and the scaphoid shift test will either cause a “clunking” sound or it will be painful to the patient.[5]
Palpation of Scapholunate Articulation[edit | edit source]
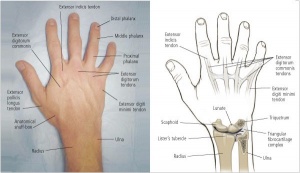
Palpate Lister’s tubercle on the distal radius. Move slightly distal to the tubercle and you will find the scapholunate joint.
Scaphoid Shift Test (Watson Test)[edit | edit source]
Procedure[edit | edit source]
- Examiner palpates and provides compression force over scaphoid (thumb on volar surface of hand—use anatomical snuff box for reference—and first finger on palmar surface) with one hand, while grasping the hand at the level of the metacarpal with the other.
- Examiner passively moves patient’s wrist into ulnar deviation and slight extension.
- Examiner passively and slowly moves patient’s wrist into radial deviation and slight flexion.
- Examiner releases compression on the scaphoid.
| [6] |
Interpretation[edit | edit source]
The test is positive if a “thunk” is produced OR the patient’s symptoms are reproduced when compression of the scaphoid is released.
Diagnostic Accuracy[5][edit | edit source]
- Sensitivity = .69
- Specificity = .66
- +LR = 2.0
Diagnostic Exam[edit | edit source]
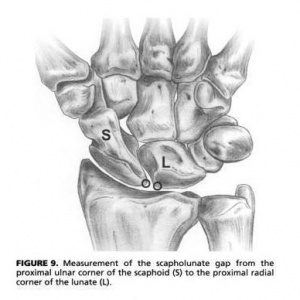
Scapholunate Interval—This measurement is the distance between the proximal medial corner of the lunate and the proximal lateral corner of the scaphoid. A separation of greater than 2 mm may be indicative of scapholunate instability and it is referred to as the “Terry Thomas sign.” This can be measured through radiographs and should be compared with the patient’s uninvolved side. A “clenched-fist” view in a radiograph may help accentuate the space between the two bones.
Outcome Measures[edit | edit source]
Potential self-report measures for individuals presenting with wrist pain are listed below.
- Disability of Arm, Shoulder, and Hand questionnaire (DASH)
- Quick DASH –This outcome measure is a shortened version of the DASH and is used to determine the patient’s physical function and symptoms.
- Brigham and Women’s Hospital Carpal Tunnel Questionnaire (CTQ) – This outcome measure is intended to assess functional status along with severity of symptoms in patients with carpal tunnel syndrome.
- Patient-Rated Wrist Evaluation Score (PRWE) – This outcome measure attempts to quantify wrist pain and disability, according to the patient, to assess the potential outcome for patients with distal radius fractures.
- Gartland and Werley Score – This is one of the most widely used outcome measures used in the clinic to evaluate wrist and hand function.
Management / Interventions[edit | edit source]
Conservative[edit | edit source]
Conservative treatments are performed to provide symptom relief. The patient may benefit from immobilization with a long opponens or a wrist control splint, shown below. The patient should also be instructed to avoid any axial loading of the wrist (i.e. resistive fisting), which can be done by using a splint with a distal block that prevents finger flexing.[7]

|

|
Surgical[edit | edit source]
Surgery is recommended if there is a significant degree of injury to the ligaments in question or if conservative interventions fail.[3] Surgery can be performed to repair the damaged ligaments that are causing instability or to fixate or fuse the carpal bones.[3][8] It has been found that soft tissue repair is the preferred surgical intervention in acute cases, while there is no stated preference in chronic cases.[9] Outcomes are best after soft tissue repair but there is no significant difference between acute and chronic cases.[9]
| [10] |
Post-Surgical Management[edit | edit source]
Patients may benefit from early, controlled mobilisation post-operatively through the use of a hinged wrist splint.[11] After surgical repair by use of a tendon transfer, the wrist is immobilised. However, immediate mobilisation should occur at the shoulder, elbow, forearm, and digits and the patient should resume light activities.[12] At 4 weeks post-operatively, protected wrist exercises may begin; torsion and the use of hand tools are to be avoided. Progressive strengthening and conditioning may begin at 6-8 weeks post-operatively and progress is determined per patient. Manual work and recreation may resume (slowly) at 3 months.
Differential Diagnosis[edit | edit source]
As with all other cases, other potential diagnoses must be ruled out before a final diagnosis of lunate instability can be determined. These other potential diagnoses for the wrist can be categorised depending on the location of the patient’s pain/symptoms.
Radial Wrist Pain[edit | edit source]
- Carpal Tunnel Syndrome
- First Carpometacarpal Osteoarthritis
- DeQuervain’s (Stenosing tenosynovitis of the tendons on the lateral border of the anatomical snuffbox)
- Colles' Fracture
- Scaphoid Fracture
- C6-C7 Radiculopathy
Non-Specific Wrist Pain[edit | edit source]
Mechanical Wrist Pain – Individuals who have symptoms suspicious of scapholunate instability with unremarkable findings on further workup may have an injury such as wrist strain or sprain, joint dysfunction, or repetitive strain injuries. Tests that differentiate between these diagnoses often do not have known reliability or diagnostic accuracy. Thus, if a specific diagnosis cannot be made with certainty, and red flags are ruled less likely, the most accurate diagnosis may be referred to as “mechanical wrist pain,” which is largely a diagnosis of exclusion. Intervention would consist of addressing the identified impairments such as joint hypomobility, decreased muscle length, or decreased strength
References[edit | edit source]
- ↑ Mayfield JK, Johnson RP, Kilcoyne RK. Carpal dislocations: pathomechanics and progressive perilunar instability. J Hand Surg Am. 1980;5 (3): 226-41
- ↑ 2.0 2.1 Wheeless C. Scapholunate Instability. Duke Orthopaedics presents Wheeless' Textbook of Orthopaedics Web site. http://www.wheelessonline.com/ortho/scapholunate_instability. Updated 2011. Accessed 03/02, 2011
- ↑ 3.0 3.1 3.2 Scapholunate Instability. UW MSK Resident Projects Web site. http://uwmsk.org/residentprojects/scapholunate.html. Updated 2005. Accessed 03/02, 2011.
- ↑ Redeker J, Vogt PM. Carpal instability. Chirurg. 2011 Jan; 82(1):85-93.
- ↑ 5.0 5.1 Dyer GS. Predynamic scapholunate instability. J Hand Surg Am. 2010 Nov;35(11):1879-1880.
- ↑ CRTechnologies. Scaphoid Shift Test (CR). Available from: http://www.youtube.com/watch?v=DGH-pHmeLnQ [last accessed 12/10/17]
- ↑ LaStayo P, Michlovitz S, Lee M. Wrist and Hand. In: Kolt GS, Snyder-Mackler L, eds. Physical Therapies in Sport and Exercise. 2nd ed. Philadelphia, PA: Elsevier Limited; 2007:338-346.
- ↑ Wheeless C. Lunotriquetral Dissociation. Duke Orthopaedics presents Wheeless' Textbook of Orthopaedics Web site. http://www.wheelessonline.com/ortho/lunotriquetral_dissociation. Accessed 03/02, 2011.
- ↑ 9.0 9.1 Zarkadas PC, Gropper PT, White NJ, Bertrand HP. A survey of the surgical management of acute and chronic scapholunate instability. J Hand Surg Am. 2004;29(5):848-57.
- ↑ Dr. Alejandro Badia, MD. Scapholunate ligament Repair Wrist Surgery Center Dr. Alejandro Badia Wrist Injury Repair. Available from: http://www.youtube.com/watch?v=57Olb3XkswQ [last accessed 12/10/17]
- ↑ Chinchalkar SJ, Pipicelli JG, Richards R. Controlled active mobilization after dorsal capsulodesis to correct capitolunate dissociation. J Hand Ther. 2010;23(4):404-10.
- ↑ Peterson SL, Freeland AE. Scapholunate stabilization with dynamic extensor carpi radialis longus tendon transfer. J Hand Surg Am. 2010;35(A):2093-2100.