Periventricular Leukomalacia (PVL)
Introduction[edit | edit source]
Periventricular Leukomalacia (PVL) is a form of brain injury occuring in both term and preterm infants. It has been cited as one of the leading causes of brain injury of a non-haemorragic nature in the cerebral white matter of the premature infant. It is an injury which can lead to deficits of physical, cognitive or behavioral deficits and is the leading cause of cerebral palsy in preterm infants..[1]The term leukomalacia has roots in the words 'Leukos' meaning white and 'malacia' meaning softening.[2]
Clinically Relevant Anatomy[edit | edit source]
- PVL refers to damage both focal or diffuse in nature, occuring in the cerebral white matter.[3]
- White matter is the network of nerve fibers which serve as communication exchange between different regions of gray matter in the brain. White matter lies beneath the gray matter and superficial to the spinal cord. [4]
- This white matter is made up of bundles of axons (both myelinated and unmyelinated) as well as glial cells. These glial cells include myelin-producing oligodendrocytes, micoglia, astrocytes and oligodendrocyte progenitor cells.[4]
Mechanism of Injury / Pathological Process
[edit | edit source]
Incidences of PVL have been linked to:[2][5]
- Neonatal hypocarbia
- Hypotension
- Prolonged cardiac surgery
- Hypocarbia
- Patent Ductus Arteriosus (PDA)
- Inflammatory or infectious occurrences - both in the maternal or foetal system, which may increase the activity of proinflammatory cytokines.
- Sick infants where events lead to the failure of areolar autoregulation of cerebral perfusion.[5]
Between the gestational ages of 23-32 weeks, the developing brain is particularly sensitive to hypoperfusion due to a still-developing arteriol system in the brain.[2]
At 32 weeks and less (gestation age), the germinal matrix (GM) of the neonate is particularly sensitive to bleeding. [5]
Hemorrhages confined to the GM generally do not have a major effect on the prognostic outcome. When bleeding extends into the ventricles, hydrocephalus may result. If this is severe, distortion of the corticospinal tracts ensues. This has been linked to more severe spastic diplegic presentation in those affected.[5]
There are 2 components of a PVL injury.[1][2]
- The first component is the focal component. This is characterized by localized necrosis of all cellular elements. This then leads to cyst formation.
- The second component is the diffuse component. This is cell-specific death of oligodendroglia - those cells which will mature into oligodendrocytes (forming the myelin of the cerebral white matter). It is characterized by reactive gliosis in the surrounding white matter of the focal site.
By 22 weeks gestation, microglial cells (which can produce toxic inflammatory mediators, free radicals and reactive oxygen intermediates) are dispersed throughout white matter.
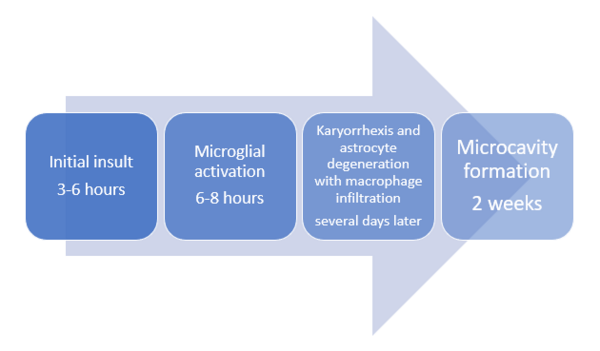
When a PVL insult occurs:
- Microglia become activated leading to a release of toxic products thought to lead to the death of premylinating oligodendroglia in the periventricular area.
- There is also the death of subplate neurons (susceptible to ischemia). These subplate neurons are important in the formation of mature thalamocortical connections. Damage to these neurons results in loss of cortical and thalamic volumes.[5][2]
Damage to the various regions of the white matter can produce deficits in motor, sensory, visual and even higher cortical functions.[2]
Epidemiology[edit | edit source]
The incidence of PVL increases with decreasing gestational age. Peak occurrence is seen between 24 and 32 weeks gestational age and in those infants weighing 1500g or less.[2]
In the United States, improved survival rates in the NICU of infants weighing less than 1500g has also lead to more infants exhibiting various developmental defects. This includes between 5% and 10% of those surviving displaying motor defects and 25%-50% displaying sensory, cognitive, and behavioral deficits.[5]
Clinical Presentation[edit | edit source]
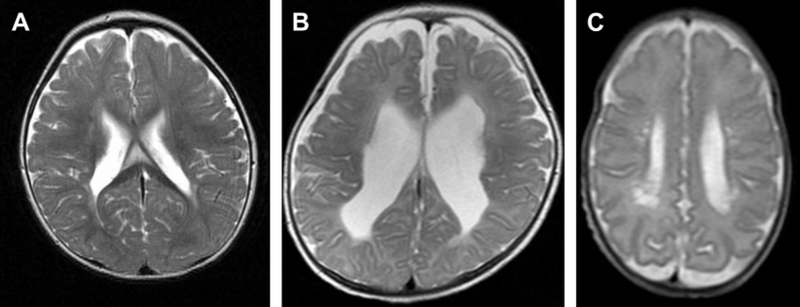
Severity of a PVL insult can be graded 1,2 or 3.[6]
- Grade 1 : Abnormally high intensity (tissue appearing 'brighter') in periventricular white matter on T2-weighted images. T2-weighted MRI images are those used to highlight fatty tissue and water.[7] There are also fluid-attenuated inversion recovery images. Inversion recovery sequences provide a high contrast between tissue and lesion.
- Grade 2: Loss of periventricular white matter with abnormally high signal intensities, as well as ventricular enlargement adjacent to the regions of the lateral ventricles.
- Grade 3: Both focal and extensive cystic changes occurring in the white matter.
In a study done in Japan[6]the risk of cystic PVL was increased with the presence of IVH grade III and IV.
Interesting notes:
The presentation of spastic diplegia is most often linked to an incidence of PVL, both in pre-term and term infants. However, term infants may exhibit more variable patterns of motor disturbances exhibit. [8]
The presence of epilepsy in PVL acquired injuries often associated with multiple seizure types and diseases which are often resistant to multiple drug treatments.[6]
Secondary microcephaly and disturbances of attention are common presentations with a PVL insult.[8]
It is important to consider a PVL injury in term infants presenting with motor abnormalities or developmental delay, even when there has been an absence of obvious perinatal difficulties.[8]
Diagnostic Procedures[edit | edit source]
Brain imaging[edit | edit source]
Ultrasonography - Can be used in utero and postnatally. Cystic changes and increased echogenicity are indicators of PVL. After 1 week of birth, ultrasonography which yields no abnormalities can exclude PVL as a diagnosis.[5]
MRI - Can be used earlier than ultrasonography. Repeated MRIs and diffuse tension imaging can be used to determine prognostic information by tracking grey matter atrophy and tract degeneration.[5]
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions
[edit | edit source]
Prevention is the best form of treatment. An important aspect in this regard is ensuring arterial CO2 (PCO2)does not fall below 35mmHg. [5]
In low-birth-weight infants, inhalation of NO has been seen to decrease the incidence of PVL. [5]
Cooling, as done for HIE has had little attention in the research and thus has no definable outcomes.[5]
Resources
[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 Volpe JJ. Neurobiology of periventricular leukomalacia in the premature infant. Pediatric research. 2001 Nov;50(5):553-62.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Ahya KP, Suryawanshi P. Neonatal periventricular leukomalacia: current perspectives. Research and Reports in Neonatology. 2018 Jan 10:1-8.
- ↑ Gallagher A, Bulteau C, Cohen D, Michaud JL. Neurocognitive Development: Normative Development. Elsevier; 2019 Sep 22.
- ↑ 4.0 4.1 Sharma R, Sekhon S, Cascella M. White matter lesions.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 Deng W, Pleasure J, Pleasure D. Progress in periventricular leukomalacia. Archives of neurology. 2008 Oct 13;65(10):1291-5.
- ↑ 6.0 6.1 6.2 Imamura T, Ariga H, Kaneko M, Watanabe M, Shibukawa Y, Fukuda Y, Nagasawa K, Goto A, Fujiki T. Neurodevelopmental outcomes of children with periventricular leukomalacia. Pediatrics & Neonatology. 2013 Dec 1;54(6):367-72.
- ↑ Radiology Masterclass. MRI interpretation T1 vs T2 images. Available from https://www.radiologymasterclass.co.uk/tutorials/mri/t1_and_t2_images (Accessed 28th September 2023)
- ↑ 8.0 8.1 8.2 Miller SP, Shevell MI, Patenaude Y, O’Gorman AM. Neuromotor spectrum of periventricular leukomalacia in children born at term. Pediatric neurology. 2000 Aug 1;23(2):155-9.
- ↑ Anne Hansen. Periventricular Leukomalacia. Available from: https://www.youtube.com/watch?v=069Eita-PZk [last accessed 27/09/2023]
- ↑ Brain - Bit by Bit. Periventricular leukomalacia on neonatal ultrasound; white matter injury of prematurity, DESHI. Available from: https://www.youtube.com/watch?v=DXy1ptfVzGQ [last accessed 04/10/2023]